По частоте обращений к врачам (невролог, терапевт) боль в спине стоит на втором месте после респираторных заболеваний. Боль в пояснице – наиболее частый и широко распространенный вариант дорсалгии [1, 2]. Ее распространенность в течение жизни достигает 80% [3], при этом часто заболеванием страдают люди трудоспособного возраста 30–45 лет. Боль в пояснице снижает качество жизни пациентов, негативно влияет на их семьи и общество в целом, поскольку это инвалидизирующая и дорогостоящая болезнь [4]. Экономическое бремя болей в спине увеличивается из-за невыхода на работу и потери производительности и довольно высокой стоимости лечения. В России половина всего трудоспособного населения ежегодно берет больничный лист из-за болей в спине.
ВЗГЛЯДЫ НА ЭТИОПАТОГЕНЕЗ
Боль в спине связана со множеством причин: она может возникать как проявление неврологических, а также различных соматических заболеваний, однако наиболее часто в практике встречаются боли невисцеральной природы (дорсопатии).
Боли неврологической природы делятся на специфические и неспецифические.
Специфическая боль включает ноцицептивные и невропатические боли, связанные с конкретным повреждением (мышц, фасций, сухожилий, остео-артрозом, остеопорозом, сдавлением корешка и т.д.).
Неспецифические боли составляют приблизительно 80–95% всех случаев болей в пояснице [5] и не имеют определенных патологоанатомических причин, таких как перелом позвоночника, инфекция, спондилоартропатия или сдавление корешка [6]. В развитии и рецидивах этого вида болей первоочередную роль играют функциональные и психосоциальные механизмы (например, страх перед движением), а не структурная патология [7]. При выборе тактики лечения таких больных всегда не хватает ясности из-за трудности определения источника боли и ее многофакторной этиологии.
По течению выделяют острые (длительность до 3 нед), подострые (6–12 нед) и хронические боли (до свыше 12 нед). У значительного количества пациентов с болями в спине (8,6–39%) заболевание приобретает хроническое течение [8, 9], что значительно ухудшает прогноз и усложняет лечение. Все это усугубляется сопутствующей депрессивной симптоматикой [10].
Хронические боли обычно тесно связаны с депрессивными расстройствами. Связь между этими состояниями продемонстрирована во многих исследованиях [11] и объясняется общими патогенетическими механизмами и нейромедиаторными сдвигами в ЦНС. Депрессия у пациентов с хронической болью в спине встречается в 3–4 раза чаще, чем в общей популяции. По данным последних публикаций, распространенность депрессии среди пациентов с хронической болью в пояснице колеблется от 20 до 64,8% [12, 13]. Показано, что в этой группе больных предикторами возникновения депрессии служат высокая интенсивность боли, злоупотребление алкоголем [14], артериальная гипертония (дисфункция симпатической нервной системы и генетические факторы рассматриваются как предположительно основные механизмы связи) [15], а также безуспешное лечение боли у врачей [16]. Депрессия негативно влияет на результаты лечения, в связи с чем терапия, направленная только на боль без устранения сопутствующих аффективных расстройств, с большой долей вероятности окажется безуспешной. К сожалению, неправильная диагностика депрессии при хронической боли в пояснице – распространенное явление, поскольку лечащий врач фокусируется на поиске физической причины боли, а пациент не осознает, что депрессия только часть данной проблемы.
Патогенез хронической боли в пояснице включает физиологические и психологические факторы, а также определенные изменения в мозге. При ее развитии включается особый болевой механизм – центральная сенситизация: посредством этого механизма из-за повышенной чувствительности нервной системы к стимулам (сенсорной гиперчувствительности) человек испытывает боль даже в отсутствие или при минимальной степени повреждения [17]. Центральная сенситизация определяется как нарушение регуляции центральной нервной системы (ЦНС) с развитием повышенной возбудимости нейронов, характеризующееся генерализованной гиперчувствительностью соматосенсорной системы к любым стимулам, как вредным, так и полезным [18, 19]. Люди, склонные к центральной сенситизации, как раз и составляют группу пациентов с неспецифической хронической болью в пояснице [20]. Показано, что наличие в преморбиде или на стадии острой боли сенсорной гиперчувствительности (установленной с помощью количественного сенсорного теста) и соматизации (психологический дистресс, проявляющийся в физических симптомах) служит предиктором развития центральной сенситизации через 3 и более месяцев после появления боли [21]. Предполагается, что определенные черты характера человека, индивидуальная чувствительность к сенсорным стимулам и/или более интенсивное физиологическое возбуждение, повышенная тревожность и другие факторы могут предрасполагать к развитию болевого синдрома и его хронизации [22].
В зависимости от происхождения выделяют следующие виды боли в спине [23]:
- дискогенные;
- корешковые (сдавление корешка вследствие грыжи диска, стеноза позвоночного канала, перидурального фиброза, спондилолистеза и спондилеза);
- боли при остеоартрозе (фасеточных суставов, крестцово-подвздошного сочленения);
- миофасциальные (при растяжении связок и мышц, спазмах мышц, травмах) [24–26].
ДИСКОГЕННАЯ БОЛЬ: ОСОБАЯ КАТЕГОРИЯ
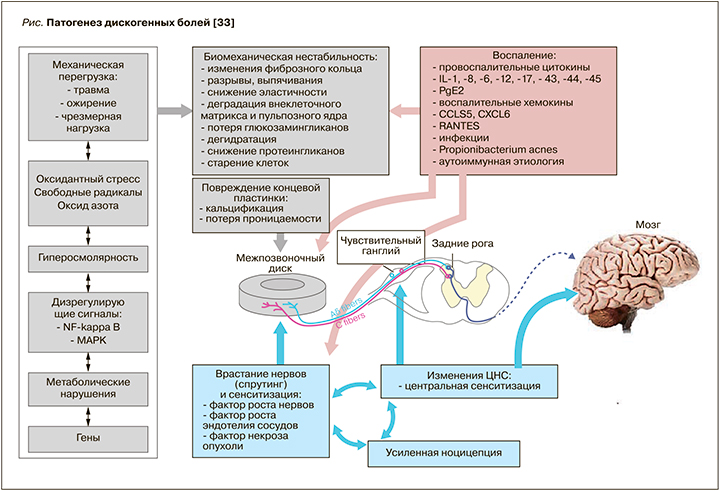
Дискогенная боль в основном включает ноцицептивный и невропатический компоненты (рис.), хотя конкретные ее причины обычно многофакторны, из-за чего этот вид болей сложно диагностировать и лечить. Обычно дискогенная боль описывается как ноющая боль различной интенсивности в области пораженного позвонка. Она усиливается при перкуссии остистых отростков, как правило, не иррадиирует в ногу; при ее развитии возможны парестезии (ощущение мурашек, покалывания) в области соответствующего дерматома.
Общепринятого определения дискогенной боли пока не сформулировано. Отчасти это можно объяснить тем, что ее трудно изолировать, и обычно она сочетается с патологией соседних структур позвоночника. Тем на менее термин «дискогенная боль» часто используется для описания боли, связанной с дегенеративными изменениями диска без грыж. Эти изменения можно увидеть на МРТ [27], когда они достигают достаточной степени выраженности (потеря высоты диска, остеофиты, кальцификация внутри пульпозного ядра, склероз кольцевой пластинки, нерегулярный хрящевой слой, смазанность границ фиброзного кольца и пульпозного ядра, избирательная потеря горизонтальных трабекул) [28–30]. Даже в отсутствие нарушений контура межпозвоночного диска множество процессов внутри него могут стимулировать болевые рецепторы и приводить к возникновению болей [31]. Показано, что ключевым фактором дискогенной боли служат воспаление и наличие свободных нервных окончаний в диске: в наружной трети фиброзного кольца и в замыкательной пластинке имеется значительное количество сосудов и нервов для генерации боли, кроме того, в межпозвонковом диске, где в норме нет сосудов и нервов, развиваются патологические ангио- и нейрогенез [32].
Дегенеративные изменения в межпозвонковых дисках считаются отправной точкой дегенеративного заболевания позвоночника и одним из важнейших факторов, предопределяющих не только появление, но и хронизацию боли в спине (см. рис.). Дальнейшее прогрессирующее старение диска и травматические воздействия ведут к морфологическим изменениям, включающим выпадение диска, грыжу, спондилез, спондилолистез, изменения по типу Модик (патологические изменения в костном мозге и концевых пластинах позвонков в виде отека костного мозга, жировой дегенерации или остеосклероза) и грыжи Шморля. Механическая перегрузка, окислительный стресс, гиперосмолярность, нарушение регуляции, расстройство системного метаболизма и генетические полиморфизмы способствуют прогрессированию структурных изменений и биомеханической нестабильности. Важное значение в дегенеративном каскаде имеет воспаление. Прямыми причинами дискогенной боли считаются врастание нервов, сенсибилизация и изменения в ЦНС. В настоящее время ведутся многочисленные доклинические исследования in vivo и in vitro, направленные на выявление источников и уточнение причин дискогенной боли, чтобы создать в будущем идеальную стратегию лечения с возможностью остановить необратимый каскад и восстановить организм до здорового состояния.
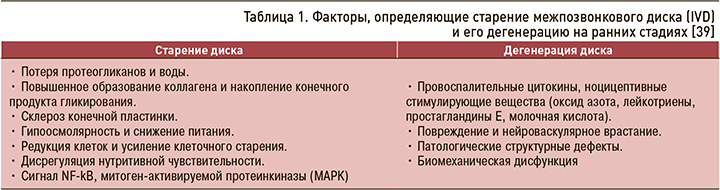
Для достижения оптимального терапевтического результата необходимо наиболее раннее выявление дегенерации и своевременно начатое лечение. Общепринятых клинических диагностических критериев дискогенной боли пока не разработано, однако предложен ряд признаков, определяющих старение межпозвонкового диска (IVD) и его дегенерацию на ранних стадиях заболевания (табл. 1). Их выявление подразумевает проведение инвазивной процедуры – провокационной КТ-дискографии. К преимуществам этого метода относится относительно высокая специфичность и чувствительность, к недостаткам – большой риск осложнений, который не позволяет широко применять провокационную КТ-дискографию для ранней диагностики дискогенной боли [34]. Кроме того, ее клиническое использование ограничено пациентами, планирующими хирургическое вмешательство.
Из неинвазивных методов для диагностики дискогенной боли предлагаются:
- клиническое обследование, выявление «красных флагов»;
- болевые опросники;
- биомаркеры сыворотки крови (новый метод, требующий уточнения и подтверждения). Их предлагается использовать в качестве индикаторов биологических процессов, вовлеченных в дискогенную боль или в качестве индикаторов системных заболеваний, таких как остеопороз. Основными кандидатами на сывороточные биомаркеры боли в спине являются хемокиновые лиганды ССL5 и CXCL6, интерлейкин-6, C-реактивный белок, фактор некроза опухоли (TNF-a), интерлейкин-1b и коллаген 2 типа [35–37], комплемент С3 и фибриноген. Также показана польза MALDI-TOF-MS-анализа [38];
- МРТ (характерны модические изменения 1 типа и гиперинтенсивные зоны).
Необходимо уточнить, что существующие методы визуализации не специфичны для дискогенной боли, тогда как более специфические методы дискографии имеют известные осложнения. В результате необходимы альтернативные неинвазивные и специфические методы диагностики для лучшей идентификации конкретного патологического состояния и источников боли, которые можно будет целенаправленно лечить.
ТРУДНОСТИ И ВОЗМОЖНОСТИ ТЕРАПИИ
На данный момент многофакторная этиология и частое отсутствие определенного источника боли предопределяют трудности в терапии дорсалгий. Основные доступные на сегодня в клинической практике лекарственные средства для лечения этого заболевания приведены в таблице 2. Однозначно установлено, что острые боли требуют срочного обезболивания пациента: чем раньше начато лечение и быстрее достигнут анальгетический эффект, тем лучше общий прогноз и меньше вероятность рецидива и хронизации боли. При острых болях рекомендуется пероральное и парентеральное введение анальгетиков, блокады с новокаином, нестероидными противовоспалительными препаратами (НПВП) и глюкокортикоидами в триггерные точки, фасеточные суставы, а также применение миорелаксантов.
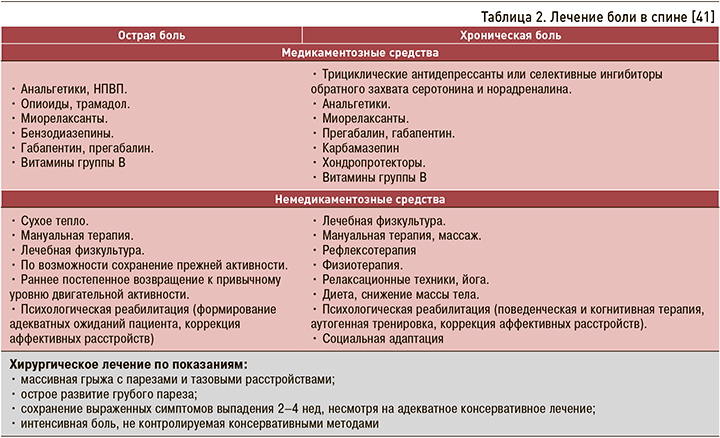
Для терапии болевых синдромов хронического течения используются иные подходы и препараты, чем при острой. По мере хронизации боли применение НПВП и простых анальгетиков становится все менее эффективным, так как в процессе формирования боли начинают преобладать центральные патофизиологические механизмы, а это требует назначения препаратов с центральным механизмом действия: анксиолитиков, трициклических антидепрессантов или селективных ингибиторов обратного захвата серотонина и норадреналина (СИОЗСН).
Важным моментом терапии хроничесой боли в спине становится воздействие на ее нейропатический компонент. Появление нейропатической боли свидетельствует о повреждении непосредственно нервных структур, обеспечивающих проведение болевой чувствительности на любом уровне, начиная с периферических нервов и кончая корой головного мозга. Для этого вида боли свойственен персистирующий характер, большая длительность, многообразие сенсорных проявлений (гиперестезия, гипералгезия, аллодиния, выпадение разных видов чувствительности), сочетание с вегетативными расстройствами (снижение кровотока, гипер- и гипогидроз в болевой области) и двигательными нарушениями [40]. Нейропатическая боль не реагирует на терапию анальгетиками и НПВП. Для ее купирования применяются:
- препараты, воздействующие на систему трансмиссии боли – блокаторы натриевых каналов (карбамазепин, ламотриджин), блокаторы кальциевых каналов (габапентин, прегабалин), блокаторы калиевых каналов (флупиртин);
- препараты, способствующие регенерации нервного волокна (витамины группы В, ипидакрин, тиоктовая кислота и др.).
ВИТАМИНЫ ГРУППЫ B: КОМПЛЕКСНЫЙ ПОДХОД
Витамины группы В широко назначаются пациентам с болевыми синдромами и рассматриваются как патогенетическая терапия при страдании нервных волокон, поскольку участвуют в целом ряде метаболических процессов (табл. 3).
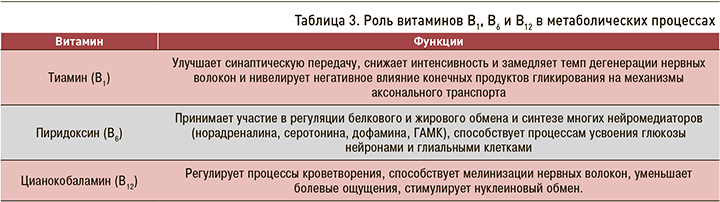
Считается, что витамины группы B обладают собственным анальгетическим действием, которое предположительно связано с подавлением синтеза и/или блокированием действия воспалительных медиаторов, торможением ноцицептивной активности в нейронах задних рогов и таламусе и усилением серотонинергической и норадренергической антиноцицептивной активности [42].
К настоящему времени накоплен большой опыт клинического применения витаминов группы В, и довольно хорошо изучена их клиническая эффективность. Проведено более 100 исследований, посвященных как отдельному, так и совместному применению витаминов В1, В6 и В12, а также их сочетанию с анальгетиками в комплексной терапии болевого синдрома.
Наибольшее количество исследований посвящено влиянию на болевой синдром цианкобаламина (В12): только в одном из более чем 90 клинических испытаний применения этого витамина не было достигнуто достоверного снижения интенсивности боли. В этих испытаниях изучались пациенты с различными нозологиями, включая боли при стенозе спинномозгового канала и с неспецифические боли в спине. Большое рандомизированное клиническое испытание у пациентов с хроническими болями в спине, проведенное в 2000 г., доказательно продемонстрировало снижение интенсивности болевого синдрома и улучшение двигательных функций на фоне внутримышечного введения В12 [43]. В 2011 г. еще одно плацебо-контролируемое исследование подтвердило эффективность и безопасность применения цианокобаламина при болях в спине. Авторы отметили, что витамин В12 действует на разные виды боли – и на ноцицептивную, и на невропатическую [44].
Комбинированное применение В1 + В6 + В12 обычно более предпочтительно, чем монотерапия, поскольку кумулирование действия трех витаминов способствует повышению эффективности терапии. Сочетание НПВП с витаминами группы B часто используется в комплексной терапии болевого синдрома. В этом плане интересно многоцентровое исследование с участием 418 пациентов с острой фазой болевого корешкового синдрома, в котором сравнивали эффективность монотерапии диклофенаком 25 мг и комбинации диклофенака 25 мг с витаминами В1 (50 мг) + В6 (50 мг) + В12 (0,25 мг) в течение 2 нед лечения. Его результаты продемонстрировали, что в случае комбинированной терапии клинический эффект развивался быстрее и был более выраженным, чем при монотерапии диклофенаком (оценивалось уменьшение болевого синдрома). Авторы при этом отмечают, что эффективность комбинированного лечения была выше у пациентов с выраженным корешковым синдромом [45]. Схожие результаты получены в других исследованиях у пациентов с болями в спине: в частности, в ряде российских работ установлено, что комбинированное лечение с включение витаминов группы B позволяет сократить сроки лечения и уменьшить эффективную дозу НПВП [46].
Показано, что при совместном назначении витамины группы B усиливают анальгетический эффект не только НПВП, но и габапентина, дексаметазона и вальпроатов [47], что позволяет снизить их дозу, уменьшаются сроки лечения и риск развития побочных эффектов.
ЗАКЛЮЧЕНИЕ
Таким образом, экспериментальные и клинические данные свидетельствуют об эффективности терапии витаминами группы B ряда заболеваний периферической и центральной нервной системы. Относительно терапии болевых синдромов можно сделать следующие выводы:
- витамины группы В обладают самодостаточной анальгетической активностью;
- их совместное применение более эффективно, чем монотерапия витаминами В1, В6, В12;
- в терапии острых болей комбинация витаминов В с НПВП демонстрирует лучший клинический результат и лучшую переносимость, чем монотерапия НПВП.
В будущем, скорее всего, показания к применению витаминов группы В будут расширяться.
В завершение следует отметить, что, несмотря на множество направлений и методик терапии болей в спине, ее лечение подчас оказывается безрезультатным, что подчеркивает необходимость новых разработок в области лечения. Наиболее многообещающими, считаются регенеративные методики, такие как биологические препараты, клеточная терапия, восстановление межпозвонкового диска и генная терапия, пока находящиеся в стадии разработки. Многочисленные клинические исследования направлены сегодня на разработку таргетной терапии, которая позволит остановить дегенеративный процесс и нормализовать состояние больного.



