Согласно данным статистического сборника по общей заболеваемости всего населения России, в 2017 г. было зарегистрировано 4446 случаев «других цереброваскулярных болезней» на 100 000 населения [1]. В нашей стране под рубрикой «другие цереброваскулярные болезни» в основном кодируется хроническая ишемия головного мозга (ХИГМ).
Стоит отметить, что диагностические критерии ХИГМ четко не определены и нуждаются в дальнейшем уточнении [2]. При анализе последних исследований можно сделать вывод, что самым надежным клиническим признаком ХИГМ служат когнитивные расстройства [3]. При этом как в случае сосудистой, так и дегенеративной патологии головного мозга они почти всегда сопровождаются некогнитивными нервно-психическими нарушениями (ННПР). К ННПР относятся эмоциональные и поведенческие симптомы; главным образом это расстройства эмоционально-аффективного спектра (тревога, депрессия, эмоциональная лабильность, раздражительность), поведенческие нарушения (апатия, ажитация, агрессия, нарушение сна и пищевого поведения), а также иногда психотические симптомы (бредовые идеи, галлюцинации). В отличие от когнитивных расстройств ННПР при церебральных заболеваниях изучены в меньшей степени [4].
В перекрестных исследованиях больных с деменцией распространенность ННПР составляет от 50 до 100%. Особенно часто они встречаются у пациентов, проживающих в домах престарелых и других социальных учреждениях. Пожизненный риск ННПР в таких случаях составляет около 100%. Наличие и выраженность эмоционально-поведенческих нарушений негативно коррелирует с показателями трехлетней выживаемости у пациентов с деменцией [5]. Следует также отметить фактор недооценки значения ННПР в повседневной клинической практике, в связи с чем не проводится их адекватная терапия. Последствием такой недооценки может стать более быстрое прогрессирование деменции, а также существенное снижение повседневной активности и качества жизни пациентов и их родственников [3, 6].
Пандемия, вызванная вирусом SARS-CoV-2, оказала влияние на различные аспекты клинической медицины, в том числе отразилась на пациентах с когнитивными расстройствами. Меры, принятые обществом для замедления распространения вируса, привели к социальному дистанцированию и снижению интенсивности когнитивной стимуляции. Ожидаемым результатом стало усугубление поведенческих симптомов и ухудшение когнитивных функций у пациентов с церебральными заболеваниями. Пандемия COVID-19 негативно повлияла на работу клиник памяти, исследовательских программ и клинических исследований в области дементирующих заболеваний [7, 8].
Подчеркнем, что пожилые люди в большей степени подвержены тяжелым последствиям COVID- 19 и осложнениям, вызванным социальной изоляцией [9, 10]. Доказано, что социальная изоляция и одиночество негативно влияют на психическое здоровье пожилых людей и являются фактором риска дальнейшего снижения когнитивных функций [10]. Поэтому пациенты с дементирующими заболеваниями в настоящее время предрасположены к более быстрому прогрессированию когнитивных и эмоционально-поведенческих расстройств [11–14].
Целью нашего исследования была оценка влияния мер социальной изоляции, введенных в связи с пандемией COVID-19, на психическое здоровье и качество жизни пожилых людей, страдающих деменцией, а также лиц, осуществляющих уход за ними.
МАТЕРИАЛ И МЕТОДЫ
Нами был проведен систематический поиск в базе PubMed по следующим ключевым словам: COVID-19, коронавирус, SARS-CoV-2; деменция, болезнь Альцгеймера, когнитивные нарушения и поведенческие нарушения. Для поиска литературы не было установлено временных ограничений. В итоге в исследование были включены статьи, опубликованные до 10 января 2021 г. (последний день поиска). Ограничений относительно типа статей также не было. Исключались работы, посвященные изучению пациентов детского или молодого возраста, исследования медицинского персонала, материалы, освещающие патогенез и терапию COVID-19, исследования, направленные на оценку непосредственного воздействия вируса на нервную систему.
РЕЗУЛЬТАТЫ
В соответствии с выбранными критериями в PubMed было найдено 1640 статей. Из них только 19 статей отражали интересующую нас проблему, и лишь 6 статей соответствовали всем критериям поиска.
Исследования пациентов с деменцией, проживающих дома
В Аргентине было проведено исследование пациентов с деменцией, проживающих во время действия ограничительных мер дома. Изучение поведенческих и когнитивных нарушений выполнялось путем анкетирования пациента. К участию в опросе были приглашены члены семей пациентов аргентинского центра старения и памяти. Выборка состояла из семей, ухаживающих за пациентами с болезнью Альцгеймера. Всего в исследовании участвовало 119 семей [15].
Выраженность когнитивных нарушений по клинической рейтинговой шкале деменции (Clinical Dementia Rating Scale) [16] была следующей: 34% выборки имели легкую деменцию, 32% – умеренную и 34% – тяжелую [15].
Анкетирование состояло из двух разделов: первый включал демографические данные членов семьи, осуществляющих уход, и лиц, страдающих деменцией; второй содержал вопросы относительно проблем ухода, с которыми пациенты и их родственники столкнулись в течение первых 8 нед карантина, связанного с коронавирусом [15].
Наиболее часто члены семьи сообщали о возникновении или обострении ранее существовавших поведенческих симптомов у опекаемых ими пациентов (у 60,5% больных с деменцией). Симптомы тревожного спектра, признаки депрессии и нарушения сна были зарегистрированы у 33; 12,8 и 14,7% выборки соответственно. Поведенческие симптомы чаще отмечались и были более выраженными у более пожилых пациентов, а также у больных, имевших расстройства тревожного спектра еще до пандемии [15]. Следует напомнить, что поведенческие и психотические симптомы становятся основной причиной ухудшения качества жизни пациентов с деменцией и лиц, осуществляющих уход за ними.
Как видно из приведенных выше данных, наиболее частым поведенческим симптомом у исследуемых больных выступала тревога. В большей степени она была распространена среди лиц с легкой формой деменции. Авторы связывают это с тем, что во время карантина данная группа пациентов была лучше осведомлена об эпидемии и рисках заболевания, и, вероятно, именно эти знания вызывали беспокойство. Заметим, что тревожное расстройство крайне негативно влияет на повседневную деятельность пациента [17].
Также у изучаемых больных оказались достаточно распространены признаки депрессии, что было ассоциировано с ухудшением качества жизни не только самих пациентов, но и лиц, осуществляющих уход.
Нарушения сна во время действия ограничительных мер у пациентов с деменцией, вероятно, были обусловлены уменьшением их активности вследствие самоизоляции, коморбидной тревогой и депрессией, а также лекарственными препаратами. Расстройства сна мешают не только самим пациентам, но и тем, кто осуществляет уход за ними [18].
Стратегии улучшения качества сна включают соблюдение гигиены сна, а также физическую активность и соблюдение структурированного распорядка дня. К сожалению, все эти стратегии были скомпрометированы в течение периода самоизоляции, что приводило к очевидным трудностям коррекции диссомнических расстройств. [15, 18].
Об ухудшении ходьбы в период самоизоляции сообщалось в 40% случаев. Нарушение походки часто встречается у пациентов с когнитивными расстройствами, особенно у ослабленных пожилых людей с выраженной деменцией, и напрямую связаны с риском падений и качеством жизни. Выполнение повседневных дел непосредственно зависит от способности пациента передвигаться. Ухудшение ходьбы во время карантина, вероятно, связано со многими факторами, включая такие, как прекращение физической и когнитивной реабилитации, маломобильность из-за постоянного пребывания дома и более широкое использование психотропных средств [15].
В цитируемой работе сообщалось об общем увеличении приема психотропных препаратов во время эпидемии со следующим распределением: на 20% возросло применение антипсихотиков, на 15% – бензодиазепинов, на 6% – снотворных средств, на 10% – антидепрессантов [15]. Побочные эффекты этих лекарственных средств могут приводить к дальнейшему снижению когнитивных функций и увеличивать риск падений и дезориентации. Такое увеличение использования потенциально неподходящих для пожилых людей лекарств может в будущем оказать пагубное влияние на состояние здоровья пациентов с когнитивными нарушениями [15, 19].
Ранее сообщалось, что когнитивный тренинг и реабилитация могут улучшить когнитивные функции и уменьшить поведенческие симптомы [20]. Недавний обзор литературы показал, что когнитивные упражнения улучшают повседневную деятельность пациентов с деменцией [21]. Однако во время пандемии большинство когнитивных тренировок и других реабилитационных мероприятий было приостановлено [15]. Занятия на дому в большинстве случаев были отменены в связи с невозможностью посещения пациента медицинским работником в условиях ограничительных мер. Реабилитация в амбулаторных условиях отменялась по тем же причинам [15].
Исследования пациентов, живущих в домах престарелых
Чтобы справиться с пандемией COVID-19 и ограничить распространение вируса среди пациентов в домах престарелых, во Франции был запрещен физический контакт между пациентами, семьями и друзьями, а в некоторых случаях даже между пациентами внутри домов престарелых или между больными и опекунами. В работе El Haj M. et al. в 2020 г. было проведено исследование влияния этих карантинных мер на психическое здоровье пациентов с болезнью Альцгеймера [22].
В исследовании участвовали 58 пациентов с клиническим диагнозом «болезнь Альцгеймера», проживающих в домах престарелых. Отбор исследуемых происходил с помощью персонала (14 психологов, врачей или медсестер) домов престарелых [22]. Критериями включения пациентов служили:
- согласие участников на проведение исследования;
- диагноз деменции, установленный неврологом или гериатром в соответствии с клиническими критериями;
- результат оценки с помощью шкалы MMSE (Mini Mental State Exam) 21/30 баллов или выше за 3 мес до начала исследования.
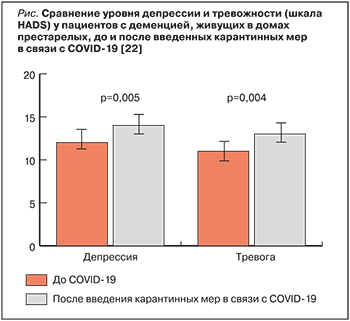 Результаты исследования свидетельствовали о нарастании депрессии и тревоги у пациентов во время ограничительных мер (рис.) [22]. Исследователи связали этот факт со значительными изменениями в их повседневной жизни. Вынужденные меры, введенные с целью предотвращения распространения инфекции в домах престарелых, ухудшили качество жизни пациентов с болезнью Альцгеймера, что потенциально может негативно сказаться на дальнейшем течении этого заболевания [22, 23].
Результаты исследования свидетельствовали о нарастании депрессии и тревоги у пациентов во время ограничительных мер (рис.) [22]. Исследователи связали этот факт со значительными изменениями в их повседневной жизни. Вынужденные меры, введенные с целью предотвращения распространения инфекции в домах престарелых, ухудшили качество жизни пациентов с болезнью Альцгеймера, что потенциально может негативно сказаться на дальнейшем течении этого заболевания [22, 23].
Исследования лиц, ухаживающих за пациентами с деменцией
Изоляция в связи с пандемией COVID-19 повлияла не только на самих пациентов с деменцией, но и на лиц, осуществляющих уход за ними [24]. Оказание помощи пожилым людям с когнитивными расстройствами уже само по себе является стрессом, который может отрицательно сказаться на психологическом благополучии опекуна [25]. Около 34% лиц, осуществляющих уход, сообщают о депрессивной симптоматике, а 43,6% – о высоком уровне тревожности [24, 26]. Следует учитывать, что уровень дистресса у лиц, осуществляющих уход, зависит не только от объективной ситуации, но и индивидуального уровня психологической устойчивости – способности противостоять физическим и психологическим проблемам или адаптироваться к ним [24, 27].
В работе Altieri M. et al., опубликованной в январе 2021 г., было исследовано 84 человека, осуществляющих уход за пациентами с деменцией. Они заполняли онлайн-анкеты, в которых оценивали депрессивную симптоматику и тревогу до и во время изоляции, а также уровень психологической устойчивости [24]. Результаты исследования показали, что пандемия COVID-19 и изоляция привели к серьезным психологическим последствиям для лиц, ухаживающих за инвалидами: у них было зафиксировано достоверное увеличение выраженности депрессивной симптоматики. Высокая «психологическая устойчивость» препятствовала нарастанию тревоги, но не влияла на депрессивную симптоматику во время изоляции. Негативное влияние оказывало снижение уровня нагрузки на лиц, осуществляющих уход. Поэтому всем лицам, опекающим больных с деменцией, даже тем, кто имеет высокий уровень психологической устойчивости, авторы рекомендуют психологическую помощь [24].
Телемедицинские технологии для преодоления последствий изоляции пациентов с деменцией
Телездравоохранение – потенциально важный инструмент для оказания повседневной медицинской помощи в условиях пандемии [28]. В работе Д.М. Гудман-Казановой с соавт. [29] были изучены эффекты телевизионной интегрированной вспомогательной технологии TV-AssistDem (интегрированная ассистивная услуга на базе TeleVision для поддержки взрослых европейцев, живущих с легкой деменцией или легкими когнитивными нарушениями). Меры, которые были приняты для преодоления негативных последствий изоляции, включали:
- информирование пациентов о происходящей ситуации, доступ к медицинским и социальным услугам;
- способы поддержки, которые предотвращали риск заражения COVID-19 и гарантировали поставку продуктов питания и предметов медицинского назначения;
- поддержание распорядка дня с сохранением привычек сна и активного отдыха;
- поддержку физической и умственной активности с помощью упражнений на когнитивную стимуляцию и обеспечение социальной связи с помощью технологий.
Телевизоры были предпочтительными технологическими устройствами для доступа к информации о COVID-19. Телевидение использовалось как для развлекательных мероприятий, так и выполнения упражнений на память и другие когнитивные функции [30].
Телевизионная поддержка с использованием TV-AssistDem продемонстрировала высокий потенциал когнитивной стимуляции [29]. Результаты исследования показали, что во время изоляции, связанной с COVID-19, физическое, психическое здоровье и благополучие были удовлетворительными для большинства пациентов, подключенных к этой телевизионной технологии.
Телекоммуникация и виртуальное общение с семьями и друзьями благоприятно сказывается на психическом здоровье пациентов с когнитивными расстройствами [31]. Также есть сообщения об эффективности домашних веб-программ для когнитивного тренинга и заочного медико-психологического консультирования [32].
Телемедицина на государственном уровне, направленная на консультирование пожилых пациентов с деменцией, может значительно помочь в период непредсказуемого течения пандемии COVID-19 [33]. В то же время некоторые эксперты высказали ряд опасений насчет телемедицины, которые необходимо решить, прежде чем эта технология станет повсеместной [31]. Так, неврологическое обследование пациентов обычно невозможно без его очного контакта с врачом. Помимо этого, во многих странах нет беспроводной инфраструктуры для полноценного внедрения телемедицинских технологий [34]. Социальная вовлеченность в очный контакт с другими людьми является критически важной потребностью для пожилых пациентов с деменцией, которым обычно трудно адаптироваться к современным технологиям [31].
ОБСУЖДЕНИЕ
Проведенные исследования демонстрируют повышение уровня тревоги, депрессии и нарушений сна в условиях ограничительных мер, связанных с пандемией COVID-19, у пациентов с деменцией, их родственников и лиц, осуществляющих уход. Для нивелирования этих неблагоприятных последствий целесообразно использовать в первую очередь немедикаментозные методики. В идеале психотерапевтические и иные методы лечения (например, когнитивная и поведенческая терапия, медитация для снижения стресса) должны быть предложены пациентам во время ограничительных мер и по их завершении с целью их адаптации и улучшения качества жизни. Для решения указанных выше задач, а также для обучения ухаживающего персонала весьма перспективно развитие телемедицинских технологий. Следует подчеркнуть, что будущие программы обучения и образования для лиц, осуществляющих уход и наблюдение за пациентами, должны строиться с учетом знаний, полученных во время пандемии COVID-19.
ЗАКЛЮЧЕНИЕ
Таким образом, результаты проведенных исследований свидетельствуют, что карантинные меры, введенные для сдерживания распространения COVID-19, неблагоприятно влияют на эмоционально-поведенческую сферу пациентов с деменцией. Лица с когнитивными расстройствами особенно уязвимы в период самоизоляции. Их потребность в уходе, медицинской и социальной реабилитации не могут быть удовлетворены в надлежащей степени. Последствия введенных карантинных мер для этой группы пациентов еще предстоит проанализировать и изучить, но уже сейчас можно сделать вывод о необходимости активной реабилитации больных с деменцией после выхода из кризиса COVID-19.