АКТУАЛЬНОСТЬ
Эндокринные заболевания являются важной медико-социальной проблемой современности, поскольку могут вызывать длительную нетрудоспособность, осложнения, значимо ухудшающие качество и прогноз жизни пациентов. Доля больных с патологией эндокринной системы постоянно увеличивается во всех экономически развитых странах мира [1]. При эндокринных заболеваниях довольно часто отмечается сопутствующее поражение кожи и придатков кожи [2, 3], которые могут быть первым поводом, вынуждающим пациента обратиться за медицинской помощью. Продолжая традиции русской терапевтической школы, созданной трудами М.Я. Мудрова, Г.А. Захарьина, С.П. Боткина, традиционные методы исследования пациентов и в настоящее время сохраняют свое значение в диагностике большинства заболеваний. Хотелось бы еще раз подчеркнуть роль общего осмотра, который в современной практической работе не используется в достаточной мере. Между тем с помощью осмотра можно выявить важные симптомы, имеющие основополагающее значение в постановке диагноза, в частности, на доклинической или манифестной стадии заболевания, оптимизировать лечебно-диагностический процесс и избежать возможных ошибок.
Цель настоящего обзора – повысить осведомленность врачей первичного звена (терапевтов и врачей общей практики), а также дерматологов и косметологов в вопросе кожных проявлений эндокринных заболеваний, выявляемых методом осмотра. Статья основана на изучении материалов зарубежных и отечественных исследований. Использованы данные преимущественно за последние 5–7 лет.
ИЗМЕНЕНИЕ И ПОРАЖЕНИЕ КОЖИ ПРИ САХАРНОМ ДИАБЕТЕ
Сахарный диабет (СД) занимает ведущее место в структуре всех эндокринных заболеваний. По данным Международной федерации диабета (IDF), в 2015 г. численность больных СД в мире превысила 415 млн человек. В России также отмечаются высокие темпы роста заболеваемости диабетом. По данным российского Госрегистра больных СД, в начале 2015 г. по обращаемости в лечебные учреждения насчитывалось около 4,1 млн человек: 340 тыс. больных СД 1-го типа и 3,7 млн человек с СД 2-го типа. Результаты контрольно-эпидемиологических исследований показали, что истинная численность пациентов с диабетом приблизительно в 3–4 раза больше зарегистрированной официально, т.е. составляет не менее 7% населения России (9–10 млн человек) [4]. При этом у больных с недиагностированным СД могут развиваться системные сосудистые осложнения, такие как нефропатия, ретинопатия, энцефалопатия, поражение сосудов сердца и головного мозга, периферических артерий, которые являются причиной инвалидизации и смерти больных.
Кожные проявления СД встречаются достаточно часто и свидетельствуют о плохой компенсации заболевания. Они могут оказывать негативное влияние не только на физическое, но и на психоэмоциональное и социальное благополучие этих пациентов. При общем осмотре больных с СД можно выявить широкий спектр кожных изменений.
Аcanthosis Nigricans (черный акантоз) – наиболее частое кожное проявление СД. Он присутствует у 74% страдающих ожирением взрослых пациентов и может быть прогностическим признаком гиперинсулинемии.
Ксероз, или ксеродерма (сухая кожа), – второе наиболее распространенное кожное проявление СД (26,4% случаев).
Диабетический рубеоз представляет собой гиперемию лица, что приводит к его общему красноватому цвету и чаще всего ассоциируется с плохим контролем гликемии [5, 6]. Рубеоз является относительно распространенным микроангиопатическим осложнением, связанным с СД. На фоне диабета наблюдается повышенная частота грибковых и бактериальных инфекций, возбудителями которых чаще всего выступают грибы рода Candida и дерматофиты, а также полимикробных инфекций, вызванных золотистым стафилококком, стрептококками, грамотрицательными аэробными бактериями и анаэробами. Наиболее распространены интертриго (с поражением подмышечной, паховой областей, межпальцевых промежутков), вульвовагинит, баланит, паронихия, глоссит и ангулярный хейлит [7].
Диабетическая склередема чаще наблюдается при длительно текущем СД в сочетании с ожирением и проявляется диффузными симметричными индуративными изменениями кожи преимущественно в области шеи и верхней трети спины по типу апельсиновой корки. По данным разных авторов, частота ее возникновения у больных СД составляет 2,5–14% [8].
Выраженный СД выявляется у 19% пациентов с красным плоским лишаем, у части которых имеет место значительное изменение глюкозотолерантного теста [9]. Часто поражение слизистой оболочки полости рта при красном плоском лишае сочетается с СД и артериальной гипертензией (синдром Потекаева–Гриншпана), причем высыпания на слизистой оболочке, как правило, носят эрозивно-язвенный характер и при длительном течении могут малигнизироваться [10, 11].
В ходе крупномасштабного исследования было установлено, что женщины, страдающие псориазом, на 63% больше предрасположены к развитию СД, по сравнению с пациентками, не имеющими этого дерматоза. На фоне СД псориаз, как правило, протекает тяжелее, при этом наблюдаются такие его формы, как экссудативный псориаз, псориатический полиартрит, псориаз крупных складок [12–14].
Диабетическая дермопатия – еще одно из кожных поражений, возникающих при метаболических нарушениях. Она начинается с папулезных высыпаний на передней поверхности голени, которые затем переходят в округлые, атрофические, красновато-коричневые пятна диаметром до 1 см [15].
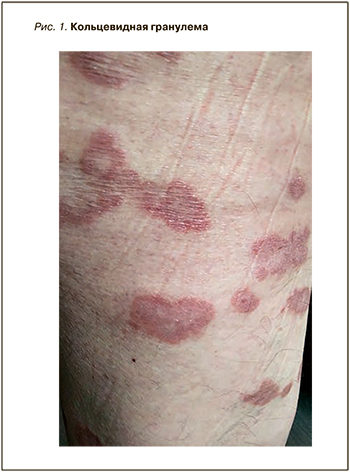
Проявлением кольцевидной гранулемы выступают расположенные кольцом или полукольцом мелкие множественные папулы (рис. 1). Они могут быть красновато-розовыми или не отличаться по цвету от окружающей кожи, имея в диаметре 1–5 см.
Диабетические пузыри (буллы) образуются спонтанно и являются следствием трофических нарушений вследствие автономной периферической полинейропатии. В этом случае характерно появление интраэпидермальных пузырей на пальцах стоп, рук, реже – на коже нижних конечностей выше стоп. Их развитие провоцируется трением обуви или одежды. Диабетические пузыри могут служить входными воротами вторичной инфекции [16].
Липоидный некробиоз – редкое некротизирующее заболевание кожи, характеризующееся дегенерацией коллагена, утолщением кровеносных сосудов и гранулематозным воспалительным процессом [17]. Как самостоятельное заболевание оно встречается только у 10% больных. Не исключается аутоиммунная этиология липоидного некробиоза. В 66% случаях он развивается на фоне СД, причем чаще СД 1; для 24% больных с этим кожным заболеванием типичны нарушение толерантности к глюкозе и отягощенная по СД наследственность [18].
Aкрохордоны – нитевидные бородавки, обычно локализующиеся в области шеи, подмышечной области, на веках и в паховой области. Они состоят из гиперпластических мягких разрастаний дермы и эпидермиса и имеют цвет обычной кожи или коричневатый цвет. Aкрохордоны – довольно распространенное явление, которое встречается примерно у 25–46% взрослого населения [19].
Витилиго характеризуется наличием хорошо очерченных, депигментированных участков кожи и волос и имеет аутоиммунное происхождение. Витилиго встречается примерно у 2–10% пациентов, страдающих СД 1-го типа [20].
Приобретенный перфорирующий дерматоз – состояние, ассоциированное с СД, хронической болезнью почек и гемодиализом (часто вызывается диабетической нефропатией). Приобретенный перфорирующий дерматоз специфически связан как с СД 1-го, так и 2-го типа. Патогенез этого заболевания изучен недостаточно, поражение кожи протекает хронически. Клинически приобретенный перфорирующий дерматоз проявляется сильным зудом, наличием куполообразных папул и узелков с центральным углублением, в котором определяется участок гиперкератоза. Поражения, как правило, развиваются на разгибательных поверхностях конечностей и туловища и реже в области головы [21, 22].
Околоногтевая телеангиэктазия представляет собой изменение кожи красноватого цвета у проксимального ногтевого валика, которое имеет место при СД. Ониходистрофия у пациентов с диабетом часто становится следствием плохого периферического кровообращения и диабетической нефропатии [23, 24]. При неконтролируемом СД также описаны случаи желтого окрашивания ладоней и подошв [25].
Папулы Хантли представляют собой гиперкератотические папулы цвета кожи, сгруппированные в виде «камешков» на разгибательной стороне пальцев при СД 2-го типа, и иногда предшествуют склеротическим изменениям пальцев [26].
Таким образом, при СД методом осмотра можно выявить ряд изменений кожи и придатков, некоторые из которых специфичны для данного заболевания и могут способствовать выявлению диабета или свидетельствовать о недостаточной его компенсации.
НАРУШЕНИЯ ФУНКЦИИ ЩИТОВИДНОЙ ЖЕЛЕЗЫ
Тиреоидная патология занимает второе место по распространенности после СД среди всех эндокринопатий и приводит к ухудшению жизненного прогноза и увеличению смертности от заболеваний сердечно-сосудистой системы [27].
Гипотиреоз – состояние, обусловленное дефицитом гормонов щитовидной железы. Признаки и симптомы, указывающие на дисфункцию щитовидной железы, неспецифичны, особенно на ранних стадиях заболевания. Наиболее частыми симптомами гипотиреоза у взрослых являются усталость, вялость, непереносимость холода, увеличение веса, запоры, изменение голоса и сухость кожи, снижение когнитивных функций. Чаще это заболевание встречается у женщин и пациентов старшего возраста. Симптомы варьируют от минимальных до опасных для жизни (микседематозная кома).
Субклинический гипотиреоз связан с повышенным риском ишемической болезни сердца, сердечной недостаточности и цереброваскулярных заболеваний [28, 29].
При выраженном гипотиреозе больные имеют характерный внешний вид: бледное, одутловатое, маскообразное лицо с узкими глазными щелями, грубые, крупные, утолщенные черты лица. Характерны отеки лица, особенно периорбитальные, век и конечностей, особенно кистей и стоп. Кожа при этом бледная, с восковидным или мраморным оттенком из-за замедления периферического кровотока и частой сопутствующей анемии. Иногда наблюдается яркий румянец щек. Возможна и желтушность кожных покровов, особенно на ладонях, вследствие избытка бета-каротина. Кожа у больных гипотиреозом холодная, температура тела снижена. Эти нарушения связаны со снижением интенсивности энергетического обмена и задержкой жидкости в организме. Кроме того, кожа у рассматриваемых больных сухая, шелушащаяся, с участками ороговения. В связи с накоплением гликозамингликанов она становится плотной, тугоподвижной, не собирается в складки.
У пациентов с гипотиреозом при осмотре может выявляться симптом Бэра – чрезмерное ороговение и утолщение эпидермиса на коленях и локтях (симптом грязных колен и локтей), иногда на тыле стоп и внутренних лодыжках. В свою очередь, синдром Вилановы–Каньяделя представляет собой гипотиреоидную дермопатию, которая проявляется сухой кожей с легким шелушением и фолликулярным гиперкератозом преимущественно на наружной поверхности плеч и бедер, на спине, а также незначительной общей гиперпигментация.
Типичным сопутствующим признаком гипотиреоза выступает и микседематозный (слизистый) отек подкожной клетчатки (а в тяжелых случаях и других органов и тканей), развивающийся вследствие внеклеточного накопления мукополисахаридов, повышающих гидрофильность тканей. При этом на отечных тканях не остается ямки от надавливания. Конечности утолщены, пальцы рук толстые и производят впечатление коротких. Волосы на голове сухие, ломкие, редкие. Отмечается выпадение ресниц, волос в области наружной трети бровей (симптом Хертога–Ротшильда), в подмышечных впадинах, на лобке. Ногти при этом ломкие, исчерченные, медленно растут [30, 31].
Диффузный токсический зоб (болезнь Грейвса) – наиболее частая причина тиреотоксикоза (80% всех случаев). Тиреотоксикоз может быть причиной фибрилляции предсердий, которая, в свою очередь, служит независимым предиктором сердечной недостаточности. Среди проявлений «тиреотоксического сердца» можно назвать также легочную гипертензию, диастолическую дисфункцию, дилатацию полостей сердца и гипертрофию миокарда левого желудочка [32].

При осмотре больных с гипертиреозом можно отметить ряд характерных изменений: эластичная, горячая на ощупь кожа, влажная за счет общего гипергидроза, эритема ладоней (рис. 2), мягкие, истонченные, слоящиеся ногтевые пластины, склонные к повышенной ломкости [33]. При этой форме дисфункции щитовидной железы возможны дисхромия кожи (гиперпигментация век – симптом Елинека; рис. 3), меланодермия типа болезни Аддисона вследствие ускоренного метаболизма глюкокортикостероидных гормонов и их относительной недостаточности, витилиго с гиперпигментацией по периферии очагов, припухлость и менискообразное свисание век, дистрофия ногтей [34]. При гипертиреозе также формируются пальцы в виде «барабанных палочек» и ногти в виде «часовых стекол» (тиреоидная акропахия). Для заболевания характерна претибиальная микседема, которая может наблюдаться в начальной стадии тиреотоксикоза или при эутиреоидном зобе и тиреоидите Хашимото (рис. 4). Обычно она локализуется на передней и боковой поверхностях обеих большеберцовых костей и может быть представлена диффузной, опухолевой, бляшкообразной или слоновой формами [35].

Пораженная кожа при гипертиреозе отечна, уплотнена, не собирается в складку, при надавливании на нее ямка не образуется. Кожа может быть инфильтрирована за счет узелковых полушаровидных или подушкообразных плоских элементов, образующих сливной, обширный, бляшкообразный очаг восковидно-желтоватого цвета (в начальной стадии цвет кожи нормальный или слабо-розовый) с характерным признаком «апельсиновой корки», обусловленным расширением отверстий волосяных фолликулов. Подобное поражение кожи может отмечаться в зоне предплечий (прерадиальная микседема). У некоторых больных отмечаются и другие изменения кожи: участки гиперпигментации, витилиго, телеангиэктазии на коже лица, уртикарии, дистрофические изменения ногтей и волос [36, 37].
БОЛЕЗНЬ (СИНДРОМ) ИЦЕНКО–КУШИНГА
Болезнь Иценко–Кушинга (БИК) считается редким заболеванием, характеризующимся гиперсекрецией адренокортикотропного гормона из-за аденомы гипофиза, которая в конечном итоге вызывает эндогенный гиперкортизолизм за счет стимуляции надпочечников. Признаки и симптомы гиперкортизолизма обычно неспецифичны: ожирение, артериальная гипертензия, разной степени выраженности гирсутизм, остеопороз, респираторные расстройства.
При общем осмотре больных можно выявить характерные черты: центрипитальное распределение подкожной жировой клетчатки (отложение жира в области живота и верхней части тела при худых конечностях – кушингоидный тип ожирения), отложение жира в надключичных областях, в области шейных позвонков, щек и живота. Лицо становится круглым, лунообразным, щеки – багрово-красного цвета (матронизм). Истончение нижних и верхних конечностей объясняется значительно выраженной атрофией поперечнополосатой мускулатуры за счет катаболизма белка [38].
При осмотре кожи выявляются такие дерматологические проявления, как атрофия кожи, фиолетовые полосы растяжения на коже (стрии), угри, полнокровие лица, гипертрихоз, гирсутизм, черный акантоз, гиперпигментация, алопеция, пурпура [39].
Эндогенный гиперкортизолизм связан с повышенным риском сердечно-сосудистых и метаболических проявлений, именно поэтому важно диагностировать БИК как можно раньше и реализовать план лечения, позволяющий минимизировать осложнения и улучшить прогноз [40].
БОЛЕЗНЬ (СИНДРОМ) АДДИСОНА
Болезнь (синдром) Аддисона обусловлена абсолютной или относительной недостаточностью гормонов коры надпочечников (глюко-и минералокортикостероидов), развивающейся в результате следующих патологических процессов: аутоиммунного воспаления (адреналита), туберкулеза, грибковой инфекции, отложения амилоидного белка, накопления солей железа при гемохроматозе, метастазов опухоли из кишечника, молочной железы или легочной ткани, вирусных болезнях (доказана роль цитомегаловируса и ВИЧ) [41, 42].
Бронзовый оттенок кожи – наиболее известный и типичный симптом болезни Аддисона. Кожа у пациента вся грязно-коричневого оттенка, цвета загара, но при этом открытые воздействию солнца участки, кожные складки выглядят темнее. При болезни Аддисона отложения мелатонина, помимо зон кожных складок и ладонных линий, особенно четко заметны вокруг сосков, в аногенитальной области и на рубцах. Отмечается также пигментация участков тела, испытывающих трение и давление (локти, колени, суставы пальцев и копчик), и слизистых оболочек (серо-коричневая пигментация; рис. 5). Участки гиперпигментации на коже могут чередоваться с участками депигментации по типу витилиго. У ряда больных волосы приобретают более темную окраску.

Помимо кожных проявлений, надпочечниковой недостаточности сопутствует ряд симптомов, определяющих опасность данного заболевания: снижение массы тела, выраженная мышечная слабостью, гипотония, судороги в икроножных мышцах и передней брюшной стенке [43, 44]. При различных стрессовых ситуациях, сопровождающихся повышением потребности в глюкокортикостероидных (стрессовых) гормонах, заболевание может осложниться адреналовым кризом и иметь неблагоприятный исход. Именно поэтому крайне важны своевременная диагностика болезни Аддисона и адекватная заместительная гормонотерапия [45].
ПОРАЖЕНИЯ КОЖИ ПРИ ДРУГИХ ЭНДОКРИНОПАТОЛОГИЯХ
Первичный гиперальдостеронизм (болезнь Конна) является причиной 5% всех случаев артериальной гипертонии и 20% случаев заболевания, резистентных к лекарственной терапии [46]. Специфических кожных изменений при этой патологии нет, однако нередко у больных имеет место багрово-цианотичная окраска лица и шеи. При гистологическом исследовании отмечаются явления гиперкератоза [47, 48].
Акромегалия – синдром, обусловленный гиперпродукцией соматотропного гормона. Кожные изменения в этом случае связаны с избыточной экспрессией гормона роста и инсулиноподобного фактора роста-1 на клетках кожи и ее придатках. Накопление кожных гликозаминогликанов вызывает отек кожи, наиболее заметный на лице, руках и ногах. Типичны жирная кожа с расширенными порами, гипертрихоз и повышенное потоотделение, а также пигментные пятна на коже, черный акантоз и псориаз [49, 50].
Гипопитуитаризм характеризуется частичным или полным дефицитом секреции гормонов гипофиза, что приводит к различным сочетаниям клинических картин надпочечниковой недостаточности, гипотиреоза, гипогонадизма, дефицита гормона роста и реже несахарного диабета. Классическим признаком гипопитуитаризма является бледная, с желтоватым оттенком кожа в области ладоней, подошв и носогубных складок (каротинемия). Кожа у больных истончается, что приводит к появлению мелких морщинок вокруг глаз и рта. Из-за недостатка меланостимулирующего гормона может произойти потеря пигментации. Кроме того, возможны выпадение волос на теле, онихолизис, появление продольных гребней и коричневатого цвета на ногтях [51].
Первичный гиперпаратиреоз (ПГПТ) сопровождается избыточной секрецией паратиреоидного гормона, приводящей к гиперкальциемии. В 80–85% случаев он обусловлен солитарной аденомой околощитовидной железы. В зависимости от спектра поражения систем и органов выделяют костную, висцеральную и смешанную формы заболевания. ПГПТ иногда сопровождается кожным зудом и хронической крапивницей. Для него характерно образование кальцинатов в мягких тканях [52].
Хронический гипопаратиреоз – редкое клиническое состояние, характеризующееся дефицитом секреции паратиреоидного гормона (в большинстве случаев вследствие ятрогенного повреждения паращитовидных желез), которое может произойти во время операции на щитовидной железе. Вторая по распространенности форма гипопаратиреоза, обусловленная иммуноопосредованным разрушением клеток околощитовидных желез, – аутоиммунный гипопаратиреоз. Он может быть изолированным заболеванием, однако значительно чаще встречается в рамках наследственного аутоиммунного полиэндокринного (полигландулярного) синдрома (АПС) 1-го типа, также известного как кандидо-эктодермальная дистрофия. Заболевание дебютирует, как правило, в детском возрасте, и в подавляющем большинстве случаев начальным его проявлением становится слизисто-кожный кандидоз, развивающийся в первые 10 лет жизни, чаще в возрасте около 2 лет. На фоне слизисто-кожного кандидоза у 84% пациентов появляется гипопаратиреоз, при этом в 88% случаев он дебютирует в возрасте до 10 лет. К другим компонентам синдрома относятся хроническая надпочечниковая недостаточность (третий классический компонент триады АПС 1-го типа, наряду со слизисто-кожным кандидозом и гипопаратиреозом), СД 1-го типа, тиреоидит Хашимото, целиакия, витилиго, аутоиммунный гепатит, гипогонадизм и др. [53].
Основные клинические проявления гипопаратиреоза обусловлены гипокальциемией и гиперфосфатемией, приводящими к увеличению нервно-мышечной возбудимости и общей вегетативной реактивности, и включают парестезии в акральных областях, фибриллярные подергивания, тонические судороги, ларинго- и бронхоспазм, неврозы [54]. При гипопаратиреозе кожа становится сухой, шелушащейся и пастозной, ногти ломкими, с поперечными бороздками, наблюдается лейконихия. Волосы грубые и редкие. Псевдогипопаратиреоз может иметь особый соматический фенотип, известный как остеодистрофия Олбрайта: он состоит из низкого роста, короткой шеи, брахидактилии и подкожных кальцификатов [55, 56].
АПС 2-го типа – наиболее распространенный вариант АПС, определяемый как сочетание надпочечниковой недостаточности с аутоиммунным тиреоидитом и/или СД 1-го типа при отсутствии гипопаратиреоза и хронического грибкового поражения кожи и слизистых оболочек, характерных для АПС-1 [57].
Аутоиммунный полиэндокринный синдром 3-го типа – сочетание патологии островкового аппарата поджелудочной железы (СД 1-го типа) и щитовидной железы. Классическая картина болезни может включать патологию других органов и систем: синдром мальабсорбции, гипогонадизм, витилиго, алопецию, реже хронический активный гепатит, пернициозную анемию и др. В отдельный подтип выделяет вариант АПС 3-го типа, при котором, кроме эндокринных нарушений, имеются два или более других аутоиммунных неэндокринных системных заболевания (ревматоидный артрит, красная волчанка и др.) [58].
Синдром поликистозных яичников (СПКЯ) – одно из наиболее распространенных женских эндокринных заболеваний, которым страдают 5–10% женщин репродуктивного возраста. Осмотр кожи позволяет выявить дерматологические проявления гиперандрогении – гирсутизм, обыкновенные угри, андрогенную алопецию и признаки вирилизации, черный акантоз. Все они относятся к числу кардинальных проявлений СПКЯ [59].
Чрезмерный рост терминальных волос у женщин по мужскому типу оказывает значительное негативное влияние на самооценку и качество жизни женщины. Гирсутизм является наиболее часто используемым клиническим диагностическим критерием гиперандрогении, и большинство случаев гирсутизма связано с избытком андрогенов. Более 80% женщин с гирсутизмом имеют СПКЯ. Кроме того, гирсутизм может иметь место при синдроме Кушинга, акромегалии, дисфункции щитовидной железы, гиперпролактинемии, а также при применении некоторых лекарственных средств, например андрогенов, анаболических стероидов и др. [60].
Ожирение – серьезная проблема общественного здравоохранения во всем мире, распространенность которой в последние десятилетия неуклонно растет. Поражение кожи при ожирении и связанном с ним метаболическом синдроме может проявляться черным акантозом, ксантоматозом, акрохордоном, целлюлитом, акне и гирсутизмом, растяжками и подошвенным гиперкератозом [61]. Обратим особое внимание на то, что акантоз присутствует у 74% страдающих ожирением взрослых пациентов и может быть прогностическим признаком гиперинсулинемии. Более того, ожирение связано с учащением бактериальных и кандидозных кожных инфекций, а также онихомикозов, воспалительных кожных заболеваний и хронических дерматозов, таких как гнойный гидраденит, псориаз и розацеа. Также оно сопровождается преждевременным поседением волос [62].
ЗАКЛЮЧЕНИЕ
Таким образом, проведенный нами анализ отечественных и зарубежных литературных данных свидетельствует о достаточно широком спектре специфических кожных проявлений при патологии эндокринной системы, которые можно выявить методом осмотра. Эти изменения могут появляться задолго до манифестации клиники заболеваний эндокринной системы. Повышение осведомленности и настороженности в данном вопросе терапевтов и врачей общей практики, наряду с дерматологами и эндокринологами, а также их плодотворное междисциплинарное сотрудничество будет способствовать более ранней диагностике и успешному лечению эндокринных заболеваний, минимизации риска развития осложнений и улучшению прогноза.