Пандемия коронавирусной болезни (COVID- 19), вызванная высококонтагиозным коронавирусом SARS-CoV-2, продолжает быть актуальной проблемой здравоохранения в мире, унося тысячи человеческих жизней каждую неделю. К сожалению, несмотря на многочисленные попытки поиска патогенетической лекарственной терапии, текущая выживаемость пациентов с COVID-19, особенно с тяжелыми формами болезни, зависит от их возможности поддерживать дыхательную функцию и газообмен [1].
Существующие в настоящее время клинические рекомендации по ведению тяжелых случаев COVID-19 в основном руководствуются принципами терапии вирусных пневмоний и сепсиса [2–5]. Однако COVID-19, по-видимому, имеет другую патофизиологию, чем привычные вирусные пневмонии и сепсис. В контексте сказанного возникает множество клинических вопросов уместности и необходимости респираторной поддержки в форме неотложной оксигенотерапии (НОТ) и неинвазивной искусственной вентиляции легких (НИВЛ) на разных этапах течения COVID-19. Цель настоящего обзора – анализ эффективной респираторной поддержки пациентов COVID-19 доступными методами реальной клинической практики.
1. ОСОБЕННОСТИ ПАТОФИЗИОЛОГИИ И ГИСТОПАТОЛОГИИ COVID-19
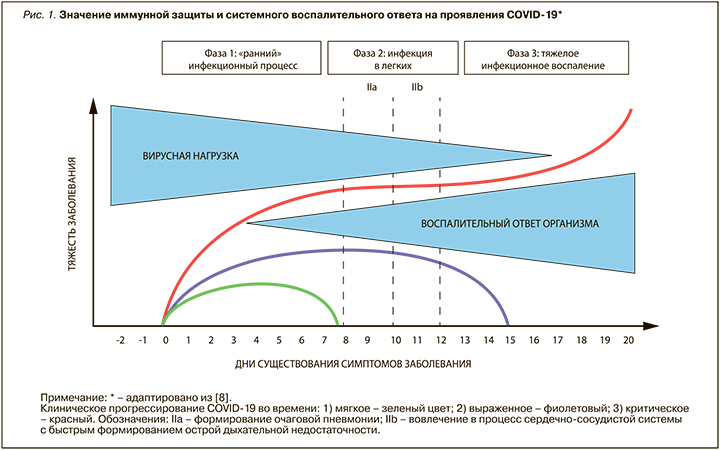
Подобно коронавирусу тяжелого острого респираторного синдрома (SARS), вирус SARS-CoV-2 поступает в клетку, используя рецептор ангиотензинпревращающего фермента-2 (АПФ-2), который присутствует в большинстве тканей человека: сосудистый эндотелий (включая сосуды легких), слизистую оболочку (полость рта и носоглотки), легочную ткань (пневмоциты II типа) [6]. Признается, что COVID-19 имеет 3 фазы, которые могут быть описаны следующим образом: «ранний» инфекционный процесс (чаще катаральный), легочная инфекция («матовое стекло»), общее тяжелое инфекционное воспаление (пневмония, сепсис) [7, 8] (рис. 1). Во время «ранней фазы» инфекции вирус инфильтрирует легочную паренхиму и начинается его репликация. Это триггирует воспалительную реакцию с вовлечением местной вазодилатации, усилением проницаемости эндотелия, рекрутирует в зону воспаления лейкоциты [9]. Фактически это говорит об вирусной «очаговой пневмонии» с формированием тяжелой гипоксемии и сердечно-сосудистой реакции на стресс.
У большинства пациентов с COVID-19 наличие микротромбов, повышенные D-димеры в плазме, были связаны с плохим прогнозом, а периферический легочный тромбоз и эмболия являлись обычным явлением при тяжелой форме COVID-19 с острой дыхательной недостаточностью (ОДН) [10]. С точки зрения патофизиологии ОДН она характеризуется как гипоксическая. Однако в ряде случаев у больных COVID-19 значительно увеличивается уровень PaCO2 (гиперкапния). Более того, у пациентов, интубированных и вентилируемых на этой фазе заболевания, существенно увеличивается альвеолярно-артериальный кислородный градиент (A-аО2) (с учетом высокой фракции кислорода (FiO2> 50%) и дыхательным коэффициентом 0,85) и присутствует существенная разница уровня CO2 артериального и конца выдоха. Это свидетельствует в пользу особого вида «пневмонии» с острым повреждением легких (ОПЛ), существенно отличающейся от бактериальной пневмонии или пневмонии при септическом шоке, часто вызывающих респираторный дистресс-синдром взрослых (РДСВ) [11].
Клинические наблюдения убедительно показывают, что привычная схема проведения искусственной вентиляции легких (ИВЛ), показавшая свою эффективность при РДВС, не эффективна среди пациентов с COVID-19 в 30,5–84,5% случаев [12]. Причиной тому служат несвоевременность и отсутствие четких алгоритмов проведения ИВЛ для пациентов COVID-19, с одной стороны, и высокая травматичность и тяжелые последствия вентилятор-ассоциированной пневмонии ‒ с другой. Именно поэтому особое клиническое значение в поддержании газообменной функции пациентов приобретают неинвазивные методы респираторной поддержки, назначаемые пациентам на ранних стадиях заболевания [13].
2. ОСОБЕННОСТИ РЕСПИРАТОРНОЙ ПОДДЕРЖКИ ПАЦИЕНТОВ COVID-19
Понимание особенностей патофизиологии и гистопатологии COVID-19 принципиально важно для установления типа и времени начала респираторной поддержки, преследующей цель поддерживать постоянство газообмена у таких пациентов (жизнесберегающая терапия). Такая респираторная поддержка объединяет методы НИВЛ через маски или шлемы, а также варианты кислородотерапии:
- неотложная оксигенотерапия (НОТ) (через назальные канюли и/или маски Вентури с потоком 5 –15 л/мин);
- высокопоточная назальная оксигенотерапия (ВНОТ) (через специальные назальные канюли с FiO2 >30%);
- длительная оксигенотерапия (ДОТ) (через назальные канюли потоком 1,5–2,0 л/мин);
- ингаляционная терапия теплой гелий-кислородной смесью (термический гелий) (t-He/ O2) (через специальный аппаратный комплекс «Гелиокс») [3].
Метод механической инвазивной (интубационной или трахеостомической) вентиляции легких (ИВЛ) относят к вентиляционной поддержке, и далее он рассматриваться нами не будет, поскольку достаточно конкретно и четко изложен в методических рекомендациях «Анестезиолого-реанимационное обеспечение пациентов с новой коронавирусной инфекцией COVID-19» Общероссийской общественной организации «Федерация анестезиологов и реаниматологов» (2020) [5].
2.1. Инфекционный контроль при респираторной поддержке
Вирусный агент SARS-CoV-2 имеет диаметр 60–140 нм, а основным путем его передачи признается аэрогенный (воздушно-капельный). Риск воздействия выдыхаемого инфицированным человеком аэрозоля на медицинского работника является реальной проблемой терапии пациентов с COVID-19. Критически важно соблюдать санитарные нормы и персональную защиту специалистов в области респираторной медицины. Каждого пациента с COVID-19 при проведении респираторной поддержки следует изолировать:
- в помещении с отрицательным давлением с 12-кратным воздухообменом в час;
- в помещениях с естественной вентиляцией не менее 160 л/с на пациента.
Медицинский персонал должен использовать максимум средств индивидуальной защиты (СИЗ) с фильтрующими респираторами/масками FFP3 N-95 и средствами защиты глаз (защитный щиток или очки защитные). Гигиена рук водой с мылом или дезинфицирующими средствами на спиртовой основе, надевание двух пар перчаток является чрезвычайно важным и должно быть стандартной практикой во всех медицинских учреждениях. Другие стратегии инфекционного контроля включают сведение к минимуму числа необходимых контактов между респираторными специалистами и больными COVID-19 с прекращением контактов для лиц, непосредственно не участвующих в уходе за пациентом [14, 15].
2.2. Особенности проведения кислородотерапии
Оксигенотерапия в различных ее формах рекомендована в качестве терапии «первой линии» для лечения респираторного дистресса и гипоксии, вызванных COVID-19. Целью оксигенотерапии служит устойчивое поддержание SpO2 >90%. В случае беременных пациенток с COVID-19 необходимый показатель SpO2 составляет 93–95% [3–5].
2.2.1. Носовая канюля. Оксигенотерапия, проводимая посредством носовой канюли, позволяет создать поток кислорода уровнем 5–6 л/мин, что увеличивает фракцию O2 в газовой смеси (FiO2) лишь до 45%. С этой целью удобно использовать современные кислородные концентраторы. Фактическое FiO2 может существенно изменяться в зависимости от скорости пикового потока вдоха больного. Важным является адекватное увлажнение подаваемого кислорода, необходимое для поддержания мукоцилиарного клиренса [16]. Доставка кислорода может вызывать значительное рассеивание выдыхаемого пациентом «облака» с максимальным расстоянием рассеивания частиц на 30 см при скорости потока в 1 л/мин и на 40 см при скорости в 5 л/мин [17].
2.2.2. Носовая маска. Кислородные маски позволяют создать поток кислорода уровнем 5–10 л/ мин, что увеличивает фракцию O2 в газовой смеси (FiO2) лишь до 55%. Такая доставка вызывает рассеивания частиц на 40 см при скорости потока 10 л/мин [17].
2.2.3. Маска «Вентури». Обеспечивают доставку кислорода уровнем 24–60% посредством специальных «трубок Вентури», что позволяет точно дозировать FiO2. При этом скорость потока кислорода варьируется от 2 до 15 л/мин. Такая доставка вызывает рассеивания частиц на 33 см при FiO2=40% и на 40 см при FiO2=24% [17].
2.2.3. Маска без обратного захвата углекислоты (ребризинговая маска). Ребризинговые кислородные маски (РКМ) обеспечивают самый безопасный способ обеспечения кислородом пациентов с COVID-19, практически исключая возможность рассеивания частиц. Они позволяют создать FiO2=90% при потоках кислорода в 15 л/мин. Для предотвращения возможной гиперкапнии специальный «мешок выдоха» должен быть всегда раздутым, для чего требуется поток не менее 10 л/мин. Такая доставка вызывает рассеивания частиц на минимальное расстояние (менее 10 см) при скорости потока в 10 л/мин [17].
2.3. Особенности проведения ингаляционной терапии термической гелий-кислородной смесью
Проведение t-He/O2 через специальные аппаратные комплексы (Гелиокс Экстрим) обеспечивает эффективную и безопасную доставку кислорода больным COVID-19 с FiO2=30–70%. Более того, аппарат позволяет создавать однородную гелий-кислородную смесь, многократно изменять и мониторировать процентное содержание гелия и кислорода, температуру ингалируемой газовой смеси во время одной процедуры с целью определения наиболее эффективного режима для каждого пациента, обеспечивать во время процедуры соответствие фактического состава гелия, кислорода и температуры заданным параметрам, мониторировать во время процедуры необходимые параметры (дыхательный объем, частоту дыхания, сатурацию), формировать равномерный ламинарный поток газовой смеси, подавать необходимые лекарственные средства через небулайзер, встроенный в дыхательный контур. Такая доставка вызывает рассеивания частиц на 30 см при FiO2=30% и на 40 см при FiO2=70% [3, 5].
2.4. Особенности проведения высокопоточной назальной оксигенотерапии
Высокопоточная назальная оксигенотерапия (ВНОТ) проводится посредством носовой канюли с высоким расходом кислорода и высокоскоростной инсуффляцией газовой смеси. Аппаратные комплексы ВНОТ обеспечивают нагревание, 100% увлажнение обогащенной газовой смеси с FiO2=30–90% с регулировкой скорости потока от 40 до 60 л/мин. Особый механизм действия ВНОТ связан с уменьшением мертвого пространства, низкого уровня PEEP, снижением частоты и работы дыхания. Такая доставка вызывает рассеивания частиц на 17 см при FiO2=60% и скорости потока в 60 л/мин [18].
2.5. Неинвазивная искусственная вентиляция легких. Проведение НИВЛ у пациентов с COVID- 19 возможно выполнить в режиме постоянного положительного давления в дыхательных путях (англ. continuous positive airway pressure – CPAP) или двухуровневого положительного давления в дыхательных путях (англ. bi-level positive airway pressure – BiPAP), обеспечивающих поддержание газообменной функции пациентов на всех этапах дыхательного цикла. При этом пациенту необходима способность самостоятельного дыхания и преодоления положительного давления на выдохе. Такие аппаратные вентиляционные комплексы способны обеспечить FiO2=100% в замкнутом вентиляционном контуре [19]. Риск образования и рассеивания аэрозоля у CPAP/BiPAP систем варьирует от управляемых параметров вентиляции, характеристик назальных масок, использования вирусных фильтров. Уровень рассеивания частиц составляет:
- для СРАР-терапии через назальную маску – 40 см при давлении EPAP=10 мбар;
- для BiPAP-терапии через назальную маску – 64 см при давлении IPAP/EPAP=10/5 мбар;
- для BiPAP-терапии через назальную маску – 95 см при давлении IPAP/EPAP=18/7 мбар [20].
Использование вместо маски гарнитуры ШЛЕМ уменьшает рассеивание частиц от границы раздела шлем–шея до 2,7 см при сохранении требуемых параметров вентиляции CPAP/BiPAP [21]. Выбор лицевой гарнитуры для выполнения НИВЛ у пациентов COVID-19 можно разделить по степени контаминации окружающей среды [4]:
- 1-й выбор – невентилируемая полная лицевая маска с вирусным фильтром на выдохе;
- 2-й выбор – шлем с воздушной подушкой для CPAP/ BiPAP;
- 3-й выбор – шлем без воздушной подушки для CPAP/ BiPAP;
- 4-й выбор – стандартная маска для лица.
3. АЛГОРИТМЫ ПРОВЕДЕНИЯ РЕСПИРАТОРНОЙ ПОДДЕРЖКИ
С учетом существующих отечественных и зарубежных клинических рекомендаций [3–5] нами был выполнен анализ подходов к проведению респираторной поддержки у пациентов с COVID- 19. Нам удалось стандартизировать основные этапы оказания респираторного пособия, практически идентичные по времени и объему во всех указанных рекомендациях. Ниже нами будет описан ступенчатый алгоритм действий (рис. 2).
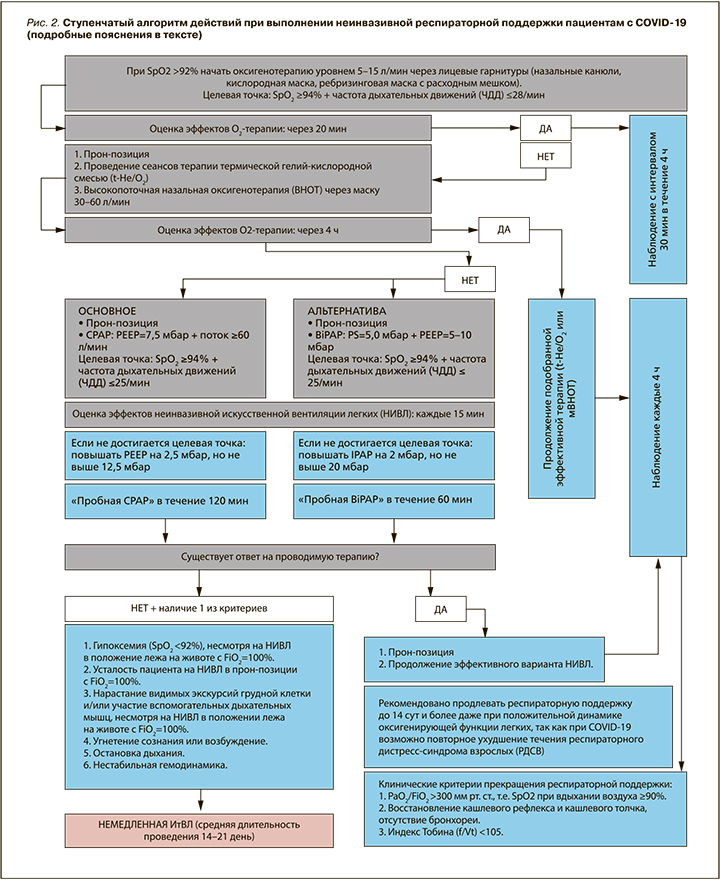
1-я ступень: при определении у пациента SpO2 <92% необходимо незамедлительно начать оксигенотерапию через лицевую маску, назальные канюли, ребризинговую маску со скоростью потока от 5 до 15 л/мин для достижения целевых значений SpO2 ≥94% и частоты дыхательных движений (ЧДД) ≤28/мин (оптимальные значения SpO2=96–98% и ЧДД=24/мин); у коморбидных пациентов (например, с хронической обструктивной болезнью легких, хронической сердечной недостаточностью, сахарным диабетом 2 типа) следует сразу приступить ко второй ступени лечения. Оценку эффективности проводимой терапии необходимо выполнить через 20 мин. При отсутствии достижения целевых уровней SpO2 и ЧДД – немедленно перейти ко 2-й ступени лечения. В случае достижения целевых значений SpO2 и ЧДД осуществляется длительный 4-часовой мониторинг жизненных показателей каждые 30 мин. У пациентов, устойчиво поддерживающие газообменную функцию в течение 4 ч, кислородотерапия может быть прекращена.
2-я ступень: кислородотерапия, не достигающая целевых значений SpO2 и ЧДД, потребует усиления респираторной поддержки. Во-первых, необходимо обеспечить пациенту «прон-позицию» (позиция, лежа на животе), в которой он должен находиться не менее 16 ч/сут. Во-вторых, рекомендуется проведение сеансов t-He/O2 с не менее чем 4 ингаляциями в сутки и индивидуальным подбором уровня FiO2, не допускающим развития гиперкапнии. В-третьих, при невозможности выполнения сеансов t-He/O2 следует приступить к ВНОТ через «защитную маску» (специализированная гарнитура для высокопоточной оксигенотерапии) уровнем 30–60 л/мин. В случае достижения целевых значений SpO2 ≥94% и ЧДД ≤25/мин подобранный индивидуально способ респираторной поддержки проводится базисно до 14 сут даже при сохранении положительной динамики оксигенирующей функции легких. Мониторинг жизненных показателей требуется выполнять каждые 4 ч. Прекращение респираторной поддержки возможно только при достижении устойчивых (не менее 5 последовательных дней) клинических критериев:
- PaO2/FiO2 >300 мм рт.ст., т.е. SpO2 при вдыхании воздуха ≥90%;
- восстановление кашлевого рефлекса и кашлевого толчка, отсутствие бронхореи;
- индекс Тобина (f/Vt) <105.
В отсутствие достижения целевых уровней SpO2 и ЧДД в течении 4 ч необходимо немедленно приступить третьей ступени.
3-я ступень: респираторная поддержка, не достигающая целевых значений SpO2 ≥94% и ЧДД ≤25/ мин через 4 ч, потребует выполнения НИВЛ в режиме CPAP-терапии уровнем PEEP=7,5 мбар + поток O2 ≥60 л/мин при сохранении пациента в «прон-позиции» (лежа на животе). В случаях плохой переносимости пациентом СРАР-терапии альтернативой выступает BiPAP-терапия, проводимая уровнем PS=5,0 мбар + PEEP = 5–0 мбар. Оценку первых эффектов НИВЛ проводят через 15 мин, ориентируясь на уровень SpO2 ≥94% и ЧДД ≤25/ мин. При необходимости проводят титрацию уровня респираторной поддержки:
- для СРАР-терапии ступенчато повышают PEEP на 2,5 мбар, но не выше 12,5 мбар;
- для BiPAP-терапии ступенчато повышают IPAP на 2 мбар, но не выше 20 мбар.
При достижении желаемого эффекта НИВЛ длительность «пробной» СРАР-терапии должна быть не менее 120 мин, а BiPAP-терапии – не менее 60 мин. Через указанное ранее время проводится повторная оценка ответа на проводимую терапию. При отсутствии ответа на НИВЛ и наличии хотя бы одного «критического признака» требуется немедленная ИтВЛ (ИВЛ) по жизненным показаниям. К таким «критическим признакам» относятся:
- гипоксемия (SpO2 <92%), несмотря на НИВЛ в положении лежа на животе с FiO2=100%;
- усталость пациента на НИВЛ в прон-позиции с FiO2=100%;
- нарастание видимых экскурсий грудной клетки и/или участие вспомогательных дыхательных мышц, несмотря на НИВЛ в положении лежа на животе с FiO2=100%;
- угнетение сознания или возбуждение;
- остановка дыхания;
- нестабильная гемодинамика.
При тяжелом течении COVID-19 средняя длительность ИтВЛ составила 14–21 день [3–5]. В случае хорошего ответа на НИВЛ рекомендуется продлевать респираторную поддержку до 14 сут и более даже при положительной динамике оксигенирующей функции легких, так как при COVID-19 возможно повторное ухудшение течения РДВС. Прекращение респираторной поддержки возможно только при достижении устойчивых (не менее 5 последовательных дней) клинических критериев, описанных ранее для второй ступени.
НИВЛ не рекомендуется пациентам с COVID-19 в следующих ситуациях [3–5]:
- отсутствие самостоятельного дыхания (апноэ);
- нестабильная гемодинамика (гипотензия, ишемия или инфаркт миокарда, жизнеугрожающая аритмия, неконтролируемая артериальная гипертензия);
- невозможность обеспечить защиту дыхательных путей (нарушение кашля и глотания) и высокий риск аспирации;
- избыточная бронхиальная секреция;
- признаки нарушения сознания (возбуждение или угнетение сознания), неспособность пациента к сотрудничеству;
- травмы или ожоги лица, анатомические дефекты, препятствующие установке маски;
- неспособность пациента убрать маску с лица в случае рвоты;
- активное кровотечение из ЖКТ;
- обструкция верхних дыхательных путей;
- дискомфорт от маски.
4. ЗАКЛЮЧЕНИЕ
Пандемия COVID-19 требует расширенного и всестороннего анализа рисков и пользы проведения неинвазивной респираторной поддержки таким пациентам. Выполнение респираторной поддержки современными вариантами кислородотерапии и НИВЛ потребует тщательной оценки рисков заражения медицинских работников, внутрибольничного распространения инфекции, наличия ресурсов здравоохранения и клинического спектра заболеваний у коморбидных пациентов с COVID-19 [3–5].


