Распространенность хронической сердечной недостаточности (ХСН) в России составляет 7–10% [1]. Основным патогенетическим фактором при формировании сердечной недостаточности признана ишемическая болезнь сердца (ИБС), в 8 раз повышающая риск ее возникновения [2].
Оценка фракции выброса (ФВ) левого желудочка (ЛЖ) служит основой для классификации больных с сердечной недостаточностью: при ФВ ЛЖ >50% определяют ХСН с сохраненной (ХСНсФВ), а при ФВ ЛЖ <40% – со сниженной ФВ (ХСНнФВ). В 2016 г. для пациентов с умеренно сниженной ФВ (40–49%) введен термин «сердечная недостаточность с промежуточной фракцией выброса» (ХСНпрФВ) [3]. Исследования показали, что доля пациентов, попадающих в категорию ХСНпрФВ, составляет от 13 до 24% [3, 4].
Наличие сопутствующей патологии связано с более тяжелым течением ХСН, ухудшением качества жизни и прогноза больных [5–7]. По данным Фремингемского исследования, ХСН повышает риск фибрилляции предсердий в 8,5 раза у мужчин и в 14 раз у женщин. Как уже отмечалось, традиционно фактором риска развития ХСН считается ИБС. Недавние исследования подчеркнули, что метаболический синдром существенно ухудшает течение ХСН [8].
Отметим, что проведенные исследования лекарственных препаратов, эффективных у больных ХСНнФВ, показали их нейтральные эффекты в случае ХСНсФВ. При этом ретроспективный анализ продемонстрировал результативность применения таких лекарств у пациентов с ХСНпрФВ.
Цель исследования – выявить особенности структурно-функционального ремоделирования миокарда у больных ХСНпрФВ ишемического генеза и методы их коррекции на основе длительной (12 мес) фармакотерапии.
МАТЕРИАЛ И МЕТОДЫ
Проведено исследование с участием 86 больных ХСНпрФВ (ФВ ЛЖ 40–49%) ишемического генеза II функционального класса (ФК) по NYHA, средний возраст – 59,3±4,7 лет. В зависимости от коморбидной патологии пациенты были разделены на 2 группы:
- • 1 группа (n=32) – без коморбидной патологии;
- • 2 группа (n=54) – при наличии таковой (26 пациентов с фибрилляцией предсердий, 28 – с метаболическим синдромом).
Критериями включения больных в исследование были:
1) ХСН с ФВ ЛЖ 40–49% (по Симпсону);
2) II ФК ХСН по NYHA;
3) стабильная стенокардия II ФК;
4) перенесенный острый инфаркт миокарда более 12 мес назад;
5) постоянная форма фибрилляции предсердий;
6) метаболический синдром;
7) подписанное информированное согласие.
Критериями невключения служили острые воспалительные, инфекционные болезни, хронические заболевания в стадии обострения, врожденные пороки сердца, кардиомиопатии.
Эхокардиографию (ЭхоКГ) проводили на сканере Vivid-7 (GE). Оценивались конечный диастоличеcкий (КДР, мм), конечный систолический размер (КСР, мм) ЛЖ, размеры левого предсердия (ЛП), толщину задней стенки ЛЖ (ТЗС) и межжелудочковой перегородки (ТМЖП), ФВ ЛЖ (по Симпсону), индекс массы миокарда (ИММ ЛЖ, г/м2). Гипертрофию ЛЖ диагностировали при значениях ИММЛЖ ≥110 г/м2 (муж.) и 95 г/ м2 (жен.). Определялись относительная толщина стенок ЛЖ (ОТСЛЖ) и индекс сферичности ЛЖ (ИСЛЖ) в систолу.
Оценка функции правого желудочка (ПЖ) выполнялась в соответствии с рекомендациями ASE [9]. Здесь измерялись такие параметры, как TAPSE – амплитуда смещения фиброзного кольца трикуспидального клапана (ФКТК) в систолу (мм), FAC (фракция укорочения площади ПЖ, %), максимальная скорость систолического смещения ФКТК (RV S’, см/с). Дисфункция ПЖ регистрировалась при изменении FAC <35% или RV S’<9,5 см/с, TAPSE <16 мм [10]. Также для ПЖ вычислялся индекс Tei, отражающий его общую производительность.
В течение 12 мес больные получали фармакотерапию в соответствии с клиническими рекомендациями Общества специалистов по сердечной недостаточности, Российского кардиологического общества и Российского научного медицинского общества терапевтов [1]. Было назначено лечение бета-адреноблокаторами (Конкор), средние дозы небиволола через 12 мес терапии составили 8,55±1,75 мг, бисопролола – 8,45±1,65 мг. Средняя доза антагониста минералокортикоидных рецепторов (АМКР) эплеренона (Инспра) была равна 48,25±2,25 мг.
Количественные значения выражали как медиану (Ме) и 25–75% интерквартильный размах (Q25%; Q75%). Сравнение количественных переменных проводили с помощью t-критерия Стьюдента, достоверными считали различия при р <0,05.
РЕЗУЛЬТАТЫ И ОБСУЖДЕНИЕ
Ремоделирование сердца – это структурно-геометрические изменения, включающие процессы гипертрофии миокарда и дилатации сердца и приводящие к нарушению систолической и диастолической функции. Нами изучены особенности ремоделирования миокарда у больных ХСНпрФВ ишемического генеза в зависимости от наличия коморбидной патологии. Результаты ЭхоКГ в изучаемых группах исследования представлены в таблице 1.
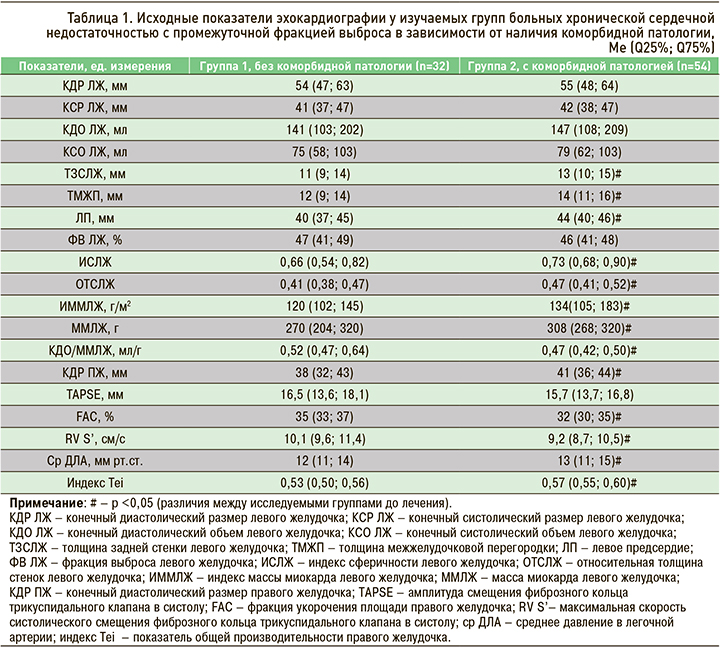
У изучаемых групп больных ХСНпрФВ ишемического генеза в зависимости от наличия коморбидной патологии не обнаружено достоверных различий по КДР ЛЖ, КДО ЛЖ, КСР ЛЖ, КСО ЛЖ. В группе пациентов с коморбидной патологией (КП+) выявлено достоверное увеличение ЛП на 9% (р <0,05), утолщение МЖП на 14% (р <0,05) и задней стенки ЛЖ на 15% (р <0,05) по сравнению с группой без коморбидной патологии (КП-). ОТСЛЖ в группе КП- была на 13% (р <0,05) меньше по сравнению с КП+. Значение ИСЛЖ в норме составляет <0,60; в группе КП- было отмечено незначительное увеличение этого параметра (р <0,01), в КП+ – умеренное увеличение по сравнению с нормой; межгрупповое различие составило 10% (р <0,05).
Нами продемонстрировано достоверное (10%; р <0,05) увеличение ММЛЖ в группе КП+ относительно КП-. Был проанализирован индекс объем/масса ЛЖ (ИОМ), определяемый как отношение КДО к ММЛЖ (мл/г). Соотношение 0,75–1,1 мл/г является нормальным, <0,75 мл/г свидетельствует о гипертрофическом типе ремоделирования ЛЖ, >1,1 мл/г – о преобладании дилатации ЛЖ. В группе КП+ ИОМ был на 10% (р <0,05) ниже, чем в КП-, что свидетельствует о нарастании гипертрофии ЛЖ при коморбидной патологии у больных ХСНпрФВ ишемического генеза.
Подводя итог проведенному исследованию, можно сделать вывод, что у больных ХСНпрФВ ишемического генеза с коморбидной патологии нарастает степень гипертрофии ЛЖ (от незначительной до умеренной), увеличивается ОТСЛЖ, ИОМ ЛЖ. Это свидетельствует о концентрическом ремоделировании ЛЖ у этой категории больных.
Принято считать, что структурно-функциональные и геометрические изменения правых отделов сердца могут определять тяжесть проявлений ХСН у больных ИБС и ухудшать прогноз. В недавних работах показано, что патологией ПЖ страдают до 48% больных ХСН, в том числе и с постинфарктным кардиосклерозом [11]. Ассоциация с ухудшением прогноза при наличии легочной гипертензии как при ХСНсФВ, так и при ХСНнФВ остается спорной [12]. Поэтому представляет интерес, насколько коморбидная патология сказывается на сократительной функции ПЖ, особенно при ХСНпрФВ. Подобные работы в доступной литературе отсутствуют, что послужило основанием для проведения нами дальнейшего изучения сократительной функции ПЖ у больных ХСНпрФВ ишемического генеза в зависимости от наличия коморбидной патологии.
В ходе исследования было выявлено (см. табл. 1) достоверное увеличение размерных параметров ПЖ в группе КП+ по сравнению с КП- на 7% (р <0,05). По показателю TAPSE достоверной разницы найдено не было (р=0,12). При сравнении по показателям FAC и RV S’ установлено снижение по обоим параметрам у больных группы КП+ на 9% (р <0,05) относительно КП-. При оценке общей производительности ПЖ (индекс Tei), обнаружено его достоверное увеличение на 7% (р <0,05) в группе КП+ по сравнению с КП-. Таким образом, на основании результатов ЭхоКГ нами выявлена дисфункция ПЖ, наиболее выраженная у больных с коморбидной патологией.
Известно, что при ИБС отмечается возрастание давления в легочной артерии (ДЛА) и сосудистого сопротивления в малом круге за счет повышения жесткости артерий [13]. В нашем исследовании данных в пользу легочной гипертензии у обследованных больных не было, однако можно отметить, что среднее ДЛА в группе КП+ оказалось на 8% выше, чем у КП- (р <0,05).
К препаратам, снижающим смертность при лечении ХСНнФВ, относят бета-адреноблокаторы, ингибиторы АПФ, антагонисты рецепторов ангиотензина II и АМКР, которые улучшают выживаемость, уменьшают заболеваемость и количество госпитализаций [4, 14]. В исследованиях по лечению больных ХСН с ФВЛЖ >40% до сих пор существует неопределенность, являются ли эти методы эффективными при ХСНсФВ, и полностью отсутствуют доказательства в отношении больных ХСНпрФВ. Практика показывает, что применение тех же классов препаратов, что и для терапии ХСНнФВ, часто приводит к уменьшению выраженности симптоматики ХСН других категорий. Нами изучены особенности ремоделирования миокарда у пациентов ХСНпрФВ ишемического генеза на фоне различных схем терапии в зависимости от коморбидной патологии.
Динамика показателей ЭхоКГ у больных ХСНпрФВ, в зависимости от коморбидной патологии и различных схем фармакотерапии, представлена в таблице 2.
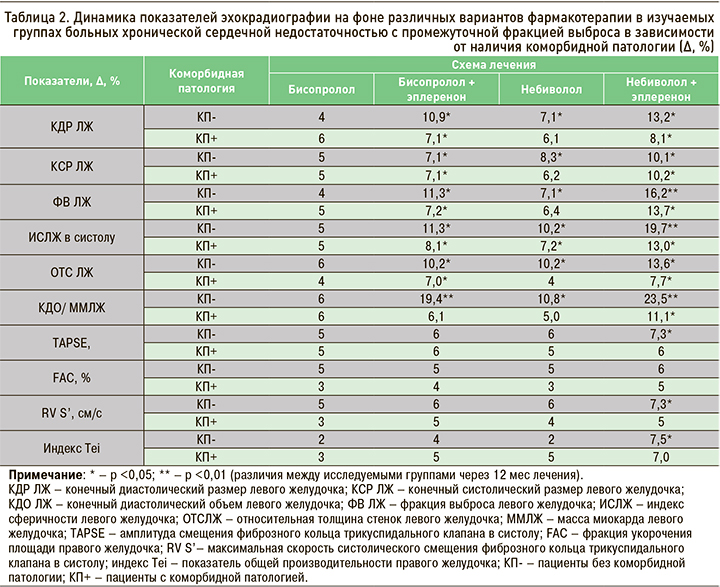
Достоверное уменьшение КДР ЛЖ было получено у больных в группе КП- при приеме небиволола, бисопролола + эплеренона (Б+Э), небиволола + эплеренона (Н+Э); в группе КП+ эффективной оказалась комбинированная терапия Н+Э.
В группе больных без КП отмечено максимальное увеличение ФВ ЛЖ до 56 (52; 58)% (∆16,2%; р <0,01) в подгруппе Н+Э, все больные перешли в категорию ХСНсФВ.
В группе КП- отмечено максимальное увеличение ФВ ЛЖ до 56 (52; 58)% (∆16,2%; р <0,01) в подгруппе Н+Э, все больные перешли в категорию ХСНсФВ. Достоверное увеличение ФВ ЛЖ до 53 (49; 55)% (∆11,3%; р<0,05) выявлено на фоне комбинации Б+Э. В подгруппе небиволола разница ФВ ЛЖ с исходными значениями составила 7,1% (р <0,05). В процессе лечения отмечалось структурное ремоделирование ЛЖ за счет снижения ОТСЛЖ: в подгруппе Н+Э на 13,6%, в подгруппах небиволола и Б+Э – на 10,2% от исходного (р <0,05). Изначально умеренно увеличенный ИСЛЖ уменьшился до нормального соотношения при приеме Н+Э (∆19,7%; р <0,01). В подгруппах Б+Э и небиволола этот показатель уменьшился на 11,3% (р <0,05), и 10,2% (р <0,05) соответственно. Максимальное увеличение ИОМ через 12 мес терапии (∆23,5%; р <0,01) наблюдалось в подгруппе Н+Э. В подгруппе небиволола аналогичное увеличение составило ∆10,8% (р <0,05), Б+Э – ∆19,4% (р <0,05).
Уменьшение КСР ЛЖ было получено при применении Б+Э, небиволола, Н+Э, при этом комбинация Н+Э позволила снизить КСР ЛЖ в группе КП+ столь же эффективно, как и в КП-. Достоверное увеличение ФВ ЛЖ при приеме небиволола, Б+Э, Н+Э было получено как в группе КП-, так и КП+, при этом наиболее эффективной оказалась терапия Н+Э. Уменьшение ИСЛЖ свидетельствовало об улучшении геометрических параметров ЛЖ у больных ХСНпрФВ, при этом наиболее эффективной была опять же комбинация Н+Э. Достоверное уменьшение ОТСЛЖ при приеме Н+Э отмечалось и в группе КП-, и в группе КП+. Данные изменения свидетельствуют, что на фоне применения Н+Э происходит адаптивное ремоделирование ЛЖ у больных ХСНпрФВ как без коморбидной патологии, так и при ее наличии.
Через 12 мес фармакотерапии больных без коморбидной патологии в подгруппах небиволола, Б+Э, Н+Э по показатели КДР ЛЖ, КСР ЛЖ и ФВ ЛЖ достигли значений, характерных для здоровых лиц. Показатели ИСЛЖ и ОТСЛЖ, соответствующие норме, в группе КП- были достигнуты на фармакотерапии Н+Э. Достоверных изменений размеров ЛП выявлено не было (р=0,064).
Хотя физиологические механизмы действия β-адреноблокаторов хорошо описаны, их влияние на функцию ПЖ не изучалось. Нарушение функции ПЖ рассматривается как предиктор неблагоприятного исхода при ХСНнФВ. Бисопролол задерживает прогрессирование правосторонней сердечной недостаточности при экспериментальной легочной гипертензии, однако его влияние на недостаточность ПЖ у больных ХСНпрФВ до сих пор не исследовалось. При недостаточности ПЖ переносимая дозировка бисопролола не приводила ни к улучшению его функции, ни к снижению симпатической активности [15].
Известно также, что АМКР снижают смертность и заболеваемость среди пациентов с тяжелой левосторонней сердечной недостаточностью, однако вклад альдостерона в патофизиологию ПЖ сердечной недостаточности до конца не установлен. В литературе нам встретилась только одна работа об отсутствии влияния эплеренона на ремоделирование ПЖ [16]. В связи с этим нами была оценена динамика изменения сократительной функции ПЖ при ХСНпрФВ. Достоверные изменения ПЖ были обнаружены у больных группы КП- по показателям TAPSE (на 7,3%; р <0,05) и RVS’ (на 7,3%; р <0,05). Особый интерес представляет уменьшение индекса Tei на 7,5% (р <0,05) у больных группы КП- на фармакотерапии Н+Э, что свидетельствует об улучшении сократительной способности ПЖ.
В группе пациентов КП-, получавших бисопролол, достоверных различий до и через 12 мес лечения получено не было.
В группе КП+ нами выявлено максимальное сокращение размеров ЛЖ в подгруппе лечения Н+Э: КДР – на 8,1%, КСР – на 10,2% (р <0,05). При приеме комбинации Б+Э аналогичное уменьшение составило 7,1% для обоих параметров (р <0,05). При терапии небивололом достоверного снижения КДР и КСР ЛЖ не наблюдалось (р >0,05). Изменения размеров ЛП не достигали достоверности (р=0,058).
Максимальное увеличение ФВ ЛЖ (∆13,7%; р <0,05) получено в подгруппе Н+Э, при этом только часть больных (44%) перешла в категорию ХСНсФВ. Достоверное увеличение ФВ произошло и в подгруппе комбинации Б+Э (∆7,2%; р <0,05). В процессе лечения отмечалось структурное ремоделирование миокарда ЛЖ, о чем свидетельствовало снижение ОТСЛЖ, которая в подгруппе Н+Э снизилась на 7,7%, небиволола – на 5% (р >0,05), Б+Э – на 7,0% (р <0,05).
Изначально умеренно увеличенный ИСЛЖ через 12 мес лечения уменьшился до нормального соотношения на фоне лечения Н+Э (∆13,0%; р <0,01). В подгруппах небиволола и Б+Э разница составила ∆7,2 и ∆8,1% соответственно (р <0,05).
Максимальное увеличение ИОМ через 12 мес терапии (∆11,1%; р <0,01) наблюдалось в подгруппе Н+Э. В подгруппе небиволола увеличение достигло ∆5,0% (р >0,05), Б+Э – ∆6,1% (р>0,05).
Уменьшение дисфункции ПЖ (∆7%; р <0,05) установлено нами только при приеме Н+Э. Влияния на остальные ЭхоКГ-показатели ПЖ проводимая терапия не оказала.
ЗАКЛЮЧЕНИЕ
Таким образом, нами установлено, что через 12 мес терапии у больных ХСНпрФВ ишемического генеза без коморбидной патологии наблюдалось улучшение изучаемых структурно-функциональных показателей. Добавление к терапии эплеренона способствовало более выраженному достоверному снижению размеров ЛЖ, ИСЛЖ и ИОМ ЛЖ. Улучшение диастолической функции ПЖ в этой группе отмечено только на фоне комбинированной терапии Н+Э.
В группе больных ХСНпрФВ ишемического генеза с коморбидной патологии выявлена менее выраженная, достоверная динамика изучаемых показателей (ИСЛЖ, ОТСЛЖ, ИОМ) на фоне лечения комбинацией Н+Э. Однако только в группе больных без коморбидной патологии, принимавших комбинацию Н+Э, отмечен переход всех пациентов в класс ХСНсФВ.