Несмотря на достижения современной медицины, сердечно-сосудистая патология по-прежнему занимает ведущее место в структуре общей заболеваемости трудоспособного населения развитых и развивающихся стран мира [1]. По данным европейских ученых, экономическое бремя кардиоваскулярных заболеваний составляет в странах Евросоюза приблизительно 169 млрд евро ежегодно, причем 62% этих расходов непосредственно связаны с системой здравоохранения. На 1000 человек теряются 2,4 рабочих года по причине смертности и 591 день по причине заболеваемости. При этом потери, которые связаны с уходом за больными, осуществляемым их родственниками и друзьями, оцениваются на уровне 29 млрд евро ежегодно [2].
Поскольку патогенетической основой сердечно-сосудистых заболеваний (ССЗ) во многих случаях выступает атеросклероз, коррекция липидного обмена является одной из важнейших задач в рамках профилактических мероприятий. Несмотря на известные и регулярно пересматриваемые ведущими профессиональными сообществами рекомендованные цели медикаментозной коррекции обмена липидов у пациентов с целью профилактики ССЗ, существует значительная часть пациентов, которые таких целей не достигают [3, 4]. Так, по данным крупнейших международных исследований, 72,4% обследованных пациентов в России, нуждающихся во вторичной профилактике ССЗ, не достигали целевых уровней холестерина липопротеидов низкой плотности (EUROASPIRE V) [5]; среди общей популяции европейцев с дислипидемией только 74,4% получали лечение, при этом лишь 41,2% пациентов достигали целевых уровней общего холестерина и ХС ЛПНП (EURIKA) [6].
Установлено, что к потенциальным причинам неэффективности гиполипидемической терапии могут относиться как факторы, связанные с компетенциями медицинских работников, так и особенности пациента (приверженность). Недостаточная приверженность к лечению лекарственными препаратами с доказанной эффективностью, по данным мировой литературы, связана с избыточной заболеваемостью и смертностью [7, 8]. Огромный арсенал возможностей воздействия на липидный обмен [9–12] в реальной клинической практике используется лишь в небольшом объеме [13].
Целью нашего исследования стало изучение факторов эффективности гиполипидемической терапии, связанных с уровнем оказывающих помощь специалистов здравоохранения и приверженностью пациентов к такой терапии, на основании анализа анкетирования врачей.
МАТЕРИАЛ И МЕТОДЫ
Для оценки факторов, оказывающих влияние на достижение целевых уровней ХС ЛПНП, была разработана уникальная анкета для опроса врачей, наблюдавших по роду своей клинической деятельности пациентов с нарушением липидного обмена. Она содержала вопросы, ответы на которые характеризовали, насколько практикующие врачи в своей практике придерживаются клинических рекомендаций, насколько большим арсеналом лекарственных препаратов и их дозировок пользуются, а также какие факторы, влияющие на приверженность пациентов к терапии, они считают актуальными. Вопросы предполагали выбор единственного ответа по умолчанию или же множественный выбор с явным указанием на такую возможность.
Вопрос с предложением провести ранжирование факторов подразумевал нумерацию ответов, начиная от единицы, в порядке уменьшения значимости, т.е. ответ 1 (единица) предполагал самый весомый фактор, по мнению конкретного врача, а 2 и последующие – все менее и менее существенные в данный момент. Допускалось установление одинакового ранга для нескольких факторов. Также возможен был пропуск ответа на любой из вопросов, кроме вопросов о специальности и стаже работы врача.
 В анкетировании приняли участие врачи, посетившие тематические конференции в июне 2019 г. в следующих городах: Астрахань (31 врач/29,52% всех опрошенных), Краснодар (13/12,38%), Москва (13/12,38%), Ростов-на-Дону (31/29,52%), Самара (17/16,19%). В анализ включались анкеты, в которых респонденты указывали, что имеют как минимум одну из нижеперечисленных специальностей: кардиолог, терапевт, врач общей практики, невролог.
В анкетировании приняли участие врачи, посетившие тематические конференции в июне 2019 г. в следующих городах: Астрахань (31 врач/29,52% всех опрошенных), Краснодар (13/12,38%), Москва (13/12,38%), Ростов-на-Дону (31/29,52%), Самара (17/16,19%). В анализ включались анкеты, в которых респонденты указывали, что имеют как минимум одну из нижеперечисленных специальностей: кардиолог, терапевт, врач общей практики, невролог.
Из анализа исключались анкеты, где не были указаны специальности и/или стаж работы врачей. Кроме них, не брались в расчет анкеты с пропущенными ответами на все вопросы, кроме вопросов о специальности и/или стаже работы. Всего в анализ вошли 105 анкет различных специалистов (рис.).
В исследовании также применялись статистические методики. Качественные параметры сопоставлялись с использованием критерия χ2. Различия считались достоверными при значении χ2 <0,05.
РЕЗУЛЬТАТЫ И ОБСУЖДЕНИЕ
Согласно рекомендациям Европейского общества кардиологов (ESC) и Российского кардиологического общества (РКО), назначение статинов показано всем пациентам с ишемической болезнью сердца (ИБС) независимо от уровней ХС ЛПНП. Данные, полученные нами в результате анализа ответов на вопрос о частоте назначения статинов больным с абсолютными показаниями к их применению, свидетельствуют, что большинство опрошенных врачей прописывает такое лечение всем или большинству пациентов (табл. 1).
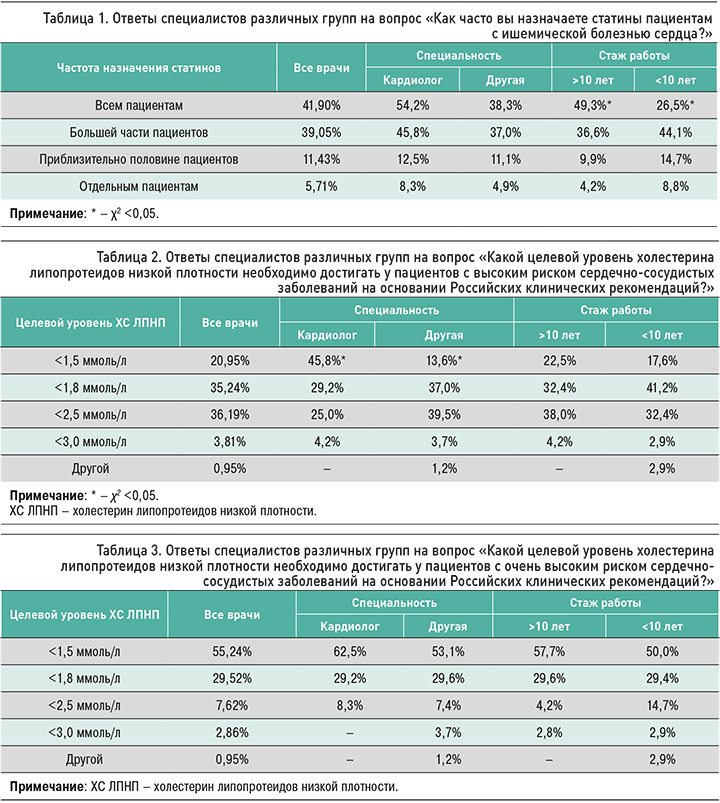
Среди врачей-респондентов всего лишь около трети (36,19%) правильно ответили на вопрос о целевых уровнях ХС ЛПНП для пациентов с высоким риском ССЗ. Однако подавляющее большинство всех ответов на данный вопрос указывало на целевые концентрации, находящиеся в приемлемом диапазоне менее 2,5 ммоль/л. Так, суммарное количество ответивших на первые 3 варианта ответов (целевые уровни ХС ЛПНП <1,5, <1,8 и <2,5 ммоль/л соответственно) составило 92,38% (n=97; табл. 2).
Большая часть респондентов правильно ответила на вопрос о целевой концентрации ХС ЛПНП, рекомендованной РКО для пациентов с очень высоким сердечно-сосудистым риском. Часть врачей в ответе на этот вопрос привела целевую концентрацию, рекомендованную ESC в 2016 г. Суммарное количество принимавших участие в анкетировании врачей указало корректные целевые уровни ХС ЛПНП по обоим вышеуказанным рекомендациям и продемонстрировало хорошие знания целей гиполипидемической терапии (табл. 3).
На вопрос относительно влияния на основную цель гиполипидемической терапии (целевой уровень ХС ЛПНП) распространенных в быту факторов, таких как употребление алкоголя и легкоусвояемых углеводов, только незначительная часть врачей дала корректный ответ, совпадающий с данными, опубликованными ведущими профессиональными сообществами (табл. 4).
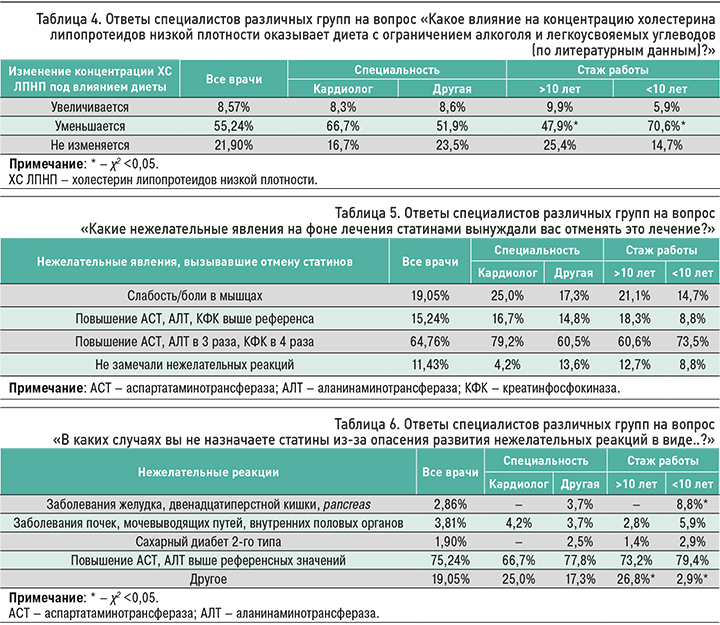
Отвечая на вопрос о развитии нежелательных реакций, которые требовали прекращения лечения статинами, часть врачей указала, что в своей практике отменяла такую терапию по неактуальным причинам, т.е. даже при незначительном повышении аспартатаминотрансферазы (АСТ), аланинаминотрансферазы (АЛТ), креатинфосфокиназы (КФК) выше референсных значений, а не при рекомендованном для уменьшения и/или отмены статинов уровне этих маркеров.
Согласно литературе, наиболее часто встречаемым побочным эффектом статинотерапии являются симптомы, связанные с мышцами: слабость и боль; по данным большинства исследователей, их встречаемость составляет около 5% [14]. В нашем исследовании лишь 19,05% врачей сталкивались с такими явлениями. Также установлено, что чаще всего (64,76%) врачи прекращали лечение статинами при повышении АСТ, АЛТ и КФК до уровней, рассматриваемых в клинических рекомендациях как критерий для отмены этой группы препаратов (табл. 5). При этом стоит отметить, что, по литературным данным, частота даже умеренного повышения АЛТ и АСТ на фоне статинотерапии составляет не более 0,5–2,0%.
С целью оценки основных факторов, препятствующих эффективному проведению гиполипидемической терапии, был задан вопрос о возможных препятствиях к назначению статинов. Ни один из предложенных респондентам ответов, согласно рекомендациям ведущих профессиональных сообществ, не должен был служить таким препятствием. Полученные результаты свидетельствуют о том, что во врачебном сообществе существует осторожное отношение к лечению статинами; при принятии решения об их назначении специалистами учитывается большое количество клинических состояний, которые уже имеются или только могут развиться у конкретного пациента (табл. 6).
Изучение применяемых в настоящее время статинов и их доз показало, что наиболее часто врачами, принимавшими участие в опросе, назначался аторвастатин по 10/20 мг (50,48%), розувастатин по 10/15 мг (40,00%) и розувастатин по 20 мг (53,33%; табл. 7). Поскольку в клинических рекомендациях оговорено, что статины необходимо назначать до максимально разрешенных или максимально переносимых доз, то крайне важной является возможность рутинного использования конкретным специалистом высоких дозировок препаратов для оптимального подбора лечения. Кроме этого, в контексте достижения целевых уровней ХС ЛПНП существенным фактором представляется возможность назначения тем же врачом различных видов статинов при высокоинтенсивной гиполипидемической терапии.
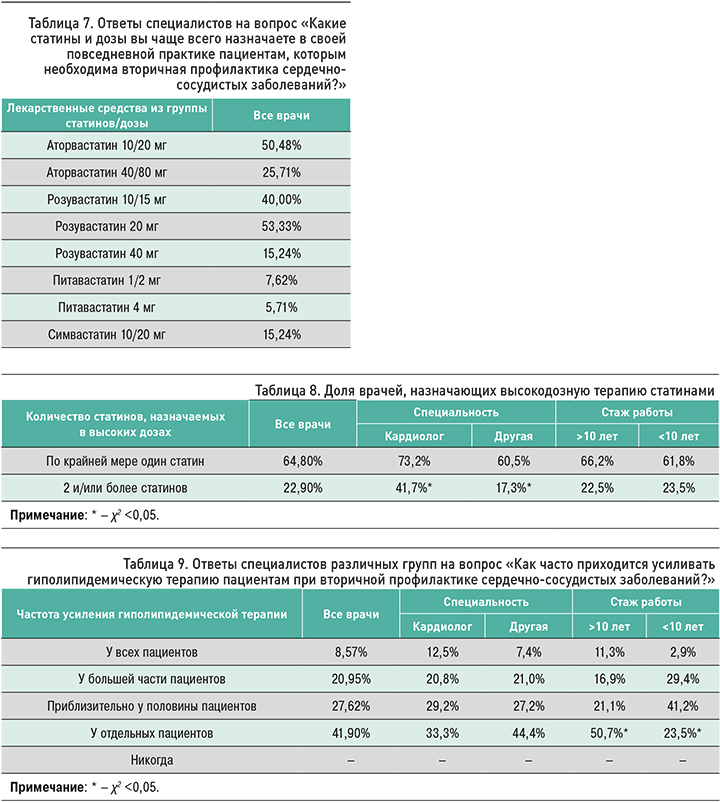
Поскольку гиполипидемическая терапия у пациентов, нуждающихся во вторичной профилактике ССЗ, предполагает назначение интенсивного лечения, дополнительно был проведен анализ количества врачей, использующих высокодозную терапию. В нашем исследовании 64,8% (n=68) врачей назначали хотя бы 1 статин в высокой дозировке. Среди прошедших анкетирование 22,9% (n=24) специалистов применяли два и более статина в рамках интенсивного лечения (табл. 8).
Недостаточная эффективность медикаментозного лечения, направленного на коррекцию липидного обмена, – общемировая проблема, поэтому усиление гиполипидемической терапии является актуальной необходимостью для ряда пациентов. Учитывая большое количество верных ответов о целевом уровне ХС ЛПНП для пациентов очень высокого сердечно-сосудистого риска, респондентам был задан вопрос о том, как часто им приходится усиливать гиполипидемическую терапию таким пациентам. Большинство ответов на этот вопрос свидетельствовало о том, что усиление терапии требуется только отдельным пациентам (41,90%; табл. 9).
Следующие вопросы были посвящены изучению факторов, способных оказать существенное влияние на приверженность пациентов к лекарственной терапии или к медицинскому сопровождению. Анализ ответов на вопрос, считают ли врачи различных специальностей обязательным убеждать пациентов в необходимости приема статинов, показал практически единодушную их позицию: почти все дали утвердительный ответ. Это косвенно свидетельствует о том, насколько важным для опрошенных специалистов видится соблюдение больным рекомендаций по лечению. С учетом большого количества врачей, верно ответивших на вопрос о целевых уровнях ХС ЛПНП, крайне актуальным является воплощение убеждающих усилий врачей, направленных на повышение эффективности гиполипидемической терапии.
Убеждение пациента в необходимости приема статинов может осуществляться по-разному, поэтому анкетируемым был задан вопрос насчет того, какие именно способы они для этого используют. Большинство указало, что предпочитает объяснить больному, почему необходим прием (87,62%) статинов, и/или сослаться на мировую практику и клинические рекомендации (26,67%; табл. 10).
Согласно результатам опроса, в 59% случаев специалисты считают, что рекомендациям по лекарственной терапии привержено большинство их пациентов. В то же время достаточно часто (22,86%) встречался ответ, что лекарственным назначениям врача привержены лишь около половины больных (табл. 11).
Приверженность к медицинскому сопровождению, так же как и к лекарственной терапии, относится к значимым факторам, способным повлиять на эффективность терапии. Изучение ответов на соответствующий вопрос показало: значительная доля опрошенных врачей (50,48%) считает, что большая часть пациентов соблюдает рекомендации по обследованию и повторным консультациям. При этом ответ, указывающий, что рекомендации по медицинскому сопровождению соблюдает лишь приблизительно половина больных, как и в случае с приверженности к фармакотерапии, встречался достаточно часто – в 25,71% (табл. 12).
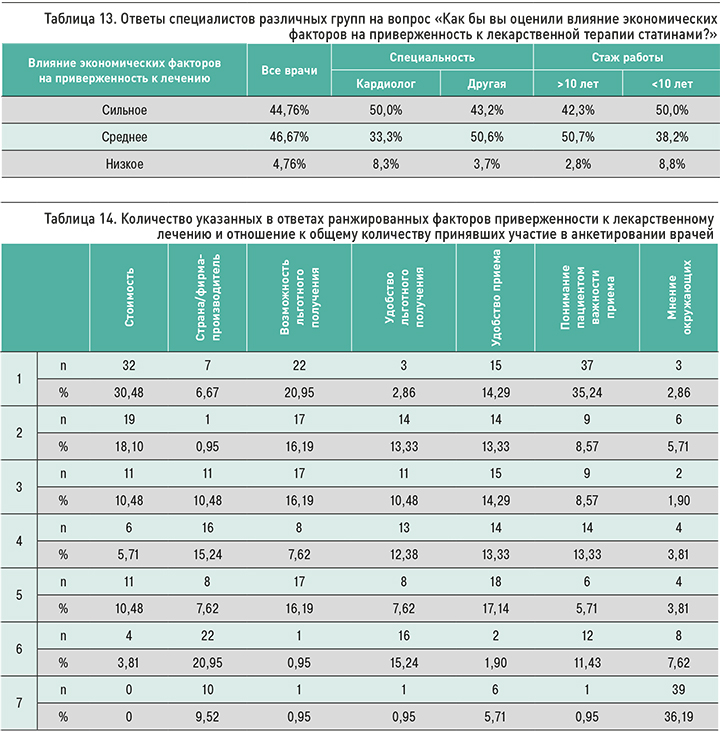
Еще один вопрос, включенный в анкету, касался того, насколько сильно, по мнению врачей, сказываются экономические факторы на соблюдении пациентами рекомендаций по лечению. Приблизительно одинаковое количество опрошенных считает, что такие факторы имеют сильное (44,76%) и среднее (46,67%) влияние на приверженность к лечению. О низком влиянии сообщило очень небольшое количество специалистов (табл. 13).
Для более детального изучения факторов, которые, с точки зрения врачей, могут оказывать влияние на приверженность лекарственной терапии, мы попросили распределить их в порядке значимости. Далее осуществлялся подсчет количества ответов с указанием определенного ранга для определенного фактора, после чего было рассчитано их отношение к общему числу врачей.
На первом месте среди факторов приверженности к фармакотерапии большинство врачей указали понимание пациентом важности приема (35,24%) и стоимость лекарственных препаратов (30,48%). Немалая доля респондентов отнесла к значимым моментам стоимость (18,10%) и возможность льготного получения (16,19%) медикаментов (табл. 14).
ЗАКЛЮЧЕНИЕ
В проведенном исследовании выявлено, что специалисты-терапевты и кардиологи первичного звена, в практике которых часто встречаются пациенты, нуждающиеся в активном воздействии на липидный обмен, в недостаточной мере информированы об основных особенностях гиполипидемической терапии. Будучи хорошо ориентированными в целевых значениях ХС ЛПНП в зависимости от сердечно-сосудистого риска, они, однако, подчас чрезмерно опасаются достигать эти уровни из-за потенциальных побочных эффектов препаратов.
Также установлено, что, по мнению врачей, главными факторами, влияющим на приверженность к лекарственной терапии, являются понимание пациентом важности приема медикаментов и их стоимость. Следовательно, недостаточную приверженность пациентов к лечению, с одной стороны, можно объяснить ограниченным временем приема у врача, осложняющим подробное объяснение больному необходимости приема назначенных лекарственных средств определенным курсом и в определенных дозировках. С другой стороны, восприятие специалистами стоимости препаратов как важного фактора приверженности к лечению может уменьшать назначение ими дополнительных, более дорогих и эффективных дополнительных методов коррекции липидного обмена.
Таким образом, доведение до пациентов причин, определяющих необходимость применения ими назначенной терапии, является одним из ведущих факторов приверженности к лечению, на который может повлиять практикующий врач. Поэтому при оказании медицинской помощи следует стремиться к созданию условий, облегчающих проведение разъяснительной работы (увеличение времени приема, демонстрация наглядных моделей, выдача обучающих материалов, размещение информационных материалов на стенах и др.). Также не вызывает сомнений, что значительным позитивным эффектом может обладать софинансирование гиполипидемической терапии со стороны государственных структур и облегчение административных процедур по получению лечения льготными категориями граждан.



