Медико-социальное значение язвенного колита (ЯК) и болезни Крона (БК), объединенных в группу воспалительных заболеваний кишечника (ВЗК), определяется неуклонным ростом частоты и распространенности этих болезней в структуре гастроэнтерологической патологии [1]. В последние годы в группу ВЗК включен микроскопический колит [2]. Нередко ВЗК дебютируют патологией опорно-двигательного аппарата [3], которая может быть как связана [4, 5], так и не связана с активностью основного заболевания [6] либо становиться следствием метаболических нарушений [7]. Несвоевременная верификация кишечного воспаления, отсроченная базисная терапия, развитие осложнений, инвалидизация определяют ВЗК как проблему не только медицинскую, но и социальную [8].
К патологии опорно-двигательного аппарата, связанной с активностью ВЗК, относят анкилозирующий спондилит (АС) и периферические артропатии I типа [9].
Остеопенический синдром при ВЗК чаще рассматривают как следствие метаболических нарушений, реже в связи с системным воспалением [10, 11]. Одним из критериев активности иммунного воспаления при ВЗК служит количественная плотность колоноцитов эпителия и собственной пластинки слизистой оболочки толстой кишки (СОТК), иммунопозитивных к CD3 [12]. Сведения о связи количественных маркеров иммунного кишечного воспаления и патологии опорно-двигательного аппарата при ВЗК единичны [13].
Цель исследования – изучить частоту, клинические, биохимические и рентгенологические особенности осевой (анкилозирующий спондилит) и периферической артропатии I типа при БК и ЯК, биохимические маркеры нарушений костного метаболизма и показатели минеральной плотности костной ткани (МПКТ) в сопоставлении с фенотипом, клиническими особенностями и морфометрическими характеристиками колоноцитов, иммунопозитивных к CD3.
МАТЕРИАЛ И МЕТОДЫ
Исследование выполнено в дизайне простого открытого одномоментного нерандомизированного исследования. В исследование были включены 194 пациента с ВЗК (157 пациентов с ЯК и 37 с БК), находившихся на обследовании и лечении в гастроэнтерологическом отделении Саратовской городской клинической больницы № 5 и терапевтическом отделении Саратовской городской клинической больницы № 32 им. В.И. Разумовского в 2016–2019 гг. (клиническая база кафедры терапии, гастроэнтерологии и пульмонологии). Критерии включения: пациенты с ВЗК в возрасте от 18 до 65 лет; наличие внекишечных проявлений ВЗК (анкилозирующий спондилит, периферические артропатии I типа, остеопенический синдром); подписанное информированное согласие пациента на участие в исследовании.
Критерии исключения: сопутствующие заболевания органов сердечно-сосудистой, дыхательной, эндокринной, мочевыделительной системы в фазе обострения; беременность; дивертикулярная болезнь кишечника; микроскопический колит; острые и хронические кишечные инфекции и паразитарные инвазии ЖКТ; неоплазия любой локализации; прием лекарственных средств, влияющих на костный метаболизм, за исключением препаратов базисной терапии.
Протокол исследования был одобрен этическим комитетом Саратовского государственного медицинского университета им. В.И. Разумовского (протокол от 05.06.2018 № 10).
Средний возраст пациентов с ЯК (n=157) составил 44 {33; 60} года, пациентов с БК (n=37) – 47,76±15,12 лет. В группу сравнения вошли 30 пациентов с ВЗК без внекишечных проявлений (15 мужчин, 15 женщин) в возрасте 43,3±10,6 лет. Группу контроля составили 30 практически здоровых лиц (15 мужчин, 15 женщин) в возрасте 41,3±11,3 лет.
Верификация ВЗК соответствовала клиническим рекомендациям Российской гастроэнтерологической ассоциации и Ассоциации колопроктологов России [14, 15]. Анкилозирующий спондилит и периферические артропатии I типа были диагностированы совместно с ревматологами в соответствии с клиническими рекомендациями Ассоциации ревматологов России от 2016 г. [16, 17]. Проводилась количественная оценка общего состояния здоровья с использованием опросника BASDAI [18], характеризующего клиническое состояние пациентов (наличие боли, припухлости и скованности в суставах) с помощью аналоговых шкал. Значение комбинированного индекса ASDASСРБ отражало активность анкилозирующего спондилита [19]. Оценка функциональной активности пациентов проводилась с использованием индекса DFI [20]. Структурные изменения костно-суставного аппарата выявлялись при рентгенологическом исследовании крестцово-подвздошного сочленения, позвоночника и крупных суставов (Philips, США, 2012).
Для оценки биохимических маркеров МПКТ в сыворотке крови определяли концентрации тартрат-резистентной кислой и щелочной фосфатазы, ионизированного кальция. Инструментальная оценка МПКТ включала денситометрию с определением показателя T-score методом двухэнергетического сканирования (Calscan, Швеция, 2008) [21].
Оценка клинико-эндоскопической и морфологической активности ВЗК выполнялась на основании клинических, эндоскопических, морфологических критериев [22, 23]. Всем пациентам делали колоноскопию (фиброколоноскоп Pentax FC-38LV, Япония, 2016) со взятием колонобиоптатов из ректосигмоидного отдела толстой кишки, а также из визуально измененных участков СОТК. Общеморфологическое исследование осуществляли с помощью светового микроскопа с увеличением ×200 [24]. Выполняли иммуногистохимическое исследование колонобиоптатов и морфометрический анализ количественной плотности колоноцитов, иммунопозитивных к CD3 (Clone 4B12, DAKO). Морфометрию CD3-иммунопозитивных клеток проводили путем подсчета количества иммунопозитивных клеток в эпителии и СОТК во всем препарате (в 5 полях зрения), исключая зоны лимфоидных фолликулов, с расчетом среднего значения количества CD3-иммунопозитивных клеток в одном поле зрения. Для оценки и клинической интерпретации полученные результаты умножали на 5, получая таким образом среднее значение количественной плотности CD3-иммунопозитивных колоноцитов на 1 мм2 СОТК. За нормальное значение принят показатель от 7 до 9 CD3-иммунопозитивных колоноцитов на 1 мм2 площади слизистой оболочки толстой кишки [25]. Морфологические и морфометрические исследования проводились в НИИ акушерства, гинекологии и репродуктологии им. Д.О. Отта при участии ассистента кафедры патологической анатомии с патологоанатомическим отделением НИИ акушерства, гинекологии и репродуктологии им. Д.О. Отта к.м.н. Ю.С. Крыловой.
Статистическую обработку полученных данных осуществляли с помощью программ Microsoft Office Excel 2016 и R-Studio Version 1.1.383. Использовались критерии Колмогорова–Смирнова, Шапиро–Уилка. Сравнение групп независимых данных проводилось посредством t-критерия Стьюдента и критериев Вилкоксона, χ-квадрата Пирсона с поправкой Йетса (χ2). Критерии Пирсона и Спирмена применялись для корреляционного анализа (критический уровень значимости установлен в p <0,05).
РЕЗУЛЬТАТЫ
Для целенаправленного выявления патологии опорно-двигательного аппарата у пациентов был использован опросник Д.И. Абдулганиевой с соавт. (2018) [26]. С учетом результатов опроса после консультации ревматолога внекишечные проявления со стороны опорно-двигательного аппарата были выявлены у 48,6% пациентов с БК и у 14% с ЯК. Больные с патологией опорно-двигательного аппарата были разделены на следующие группы:
- • ЯК + периферические артропатии I типа (n=13);
- • БК + анкилозирующий спондилит (n=5);
- • БК + периферические артропатии I типа (n=6).
К периферическим артропатиям I типа относили серонегативные артриты тазобедренных (1,3% пациентов с ЯК и 5,4% с БК), коленных (5,1% пациентов с ЯК и 8,1% с БК), локтевых (1,9% пациентов с ЯК и 2,7% с БК) суставов.
Средний возраст пациентов с ЯК и периферическими артропатиями I типа (n=13) составил 57,5±13,3 лет, с БК и периферическими артропатиями I типа (n=6) – 48,3±11,9 лет, с БК и АС (n=5) – 54±6,7 лет. При этом больные из группы с ЯК + периферические артропатии I типа значимо старше пациентов группы БК + периферические артропатии I типа (r=0,42; р=0,036).
Особенности анамнеза пациентов с ВЗК и патологией опорно-двигательного аппарата представлены в таблице 1.
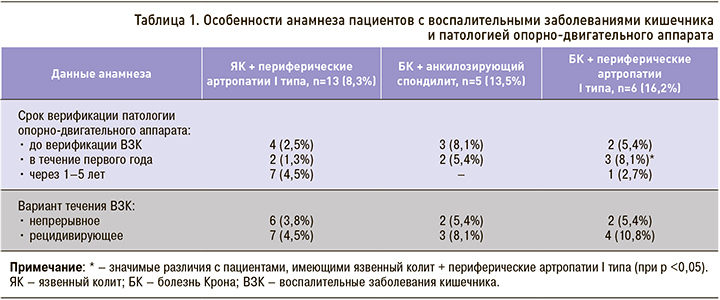
У 2,5% пациентов с ЯК и у 13,5% с БК заболевание кишечника дебютировало артропатией. После верификации ВЗК в течение первого года периферические артропатии I типа значимо чаще развивались при БК, чем ЯК (р=0,044).
При периферических артропатиях I типа боли в тазобедренных суставах отмечали 1,3% пациентов с ЯК и 5,4% с БК. Для болей в коленных суставах аналогичные показатели составили 5,1 и 8,1% соответственно, для болей и припухлости локтевых суставов – 1,9 и 2,7% соответственно. При этом 4,5% пациентов с ЯК и 13,5% пациентов с БК связывали усиление суставного синдрома с атакой ВЗК. Анкилозирующий спондилит был выявлен только у пациентов с БК, характеризовался болями в позвоночнике и крестцово-подвздошном сочленении, утренней скованностью в суставах и позвоночнике длительностью более 30 мин.
При рентгенологическом исследовании крупных суставов больных с ВЗК и периферическими артропатиями I типа были обнаружены изменения в виде околосуставного остеосклероза крестцово-подвздошных сочленений без признаков (15,4% пациентов с ЯК ) и с признаками сужения суставной щели (16,6% пациентов с БК), сужение суставной щели коленных суставов с незначительным склерозом субхондральной кости (30,8% пациентов с ЯК, 33,2% с БК), сужение суставной щели тазобедренных суставов (7,7% пациентов с ЯК, 38,5% с БК), сужение суставной щели локтевых суставов (15,4% пациентов с ЯК). Выявленные нами изменения совпадают с описанными в литературе [27].
У пациентов с анкилозирующим спондилитом при БК индекс BASDAI составил 5,3±0,8, индекс ASDASСРБ – 2,6±0,2; это отражало высокую активность заболевания позвоночника. При рентгенологическом исследовании крестцово-подвздошного сочленения были обнаружены 2-я (8,1%) и 3-я (5,4%) стадии сакроилеита. При рентгенографии позвоночника диагностированы квадратизация поясничных и нижнегрудных позвонков (10,6%), околосуставной остеосклероз (13,5%). При анкилозирующем спондилите на фоне БК оценка функциональной активности установила ограничение непрофессиональной деятельности (II функциональный класс) у 5,4% пациентов и частично профессиональной деятельности (III функциональный класс) – у 8,1%.
Особенности анамнеза пациентов с остеопеническим синдромом при ВЗК представлены в таблице 2.
После верификации заболевания кишечника остеопения при БК чаще развивалась в течение первого года. При ЯК остеопения чаще выявлялась через 3–4 года после верификации кишечной патологии. При анализе остеопении с учетом локализации БК было установлено, что у 4 из 5 пациентов с БК имелся терминальный илеит. Остеопению у этих больных можно объяснить нарушением процессов активного и пассивного транспорта кальция в кишечнике [28]. Изменение концентрации ионизированного кальция в крови как маркера остеопении при рецидивирующем течении ВЗК, вероятно, связано с повторными курсами стероидов [14, 15]. Нами выявлены корреляции средней силы между содержанием ионизированного кальция и рецидивирующим течением заболевания (r1=0,47, р1=0,038 для ЯК; r2=0,44, р2=0,043 для БК). Также определены корреляционные связи этого показателя со стероидозависимостью (r1=0,47, р1=0,038 для ЯК; r2=0,44, р2=0,043 для БК).
Результаты денситометрии с определением показателя T-score методом двухэнергетического сканирования при ВЗК представлены в таблице 3.
У пациентов с внекишечными проявлениями ВЗК выявлены значимые изменения показателя T-score. Обращает на себя внимание, что денситометрические признаки снижения МПКТ при БК встречались чаще, чем при ЯК, однако эти различия не имели статистической значимости.
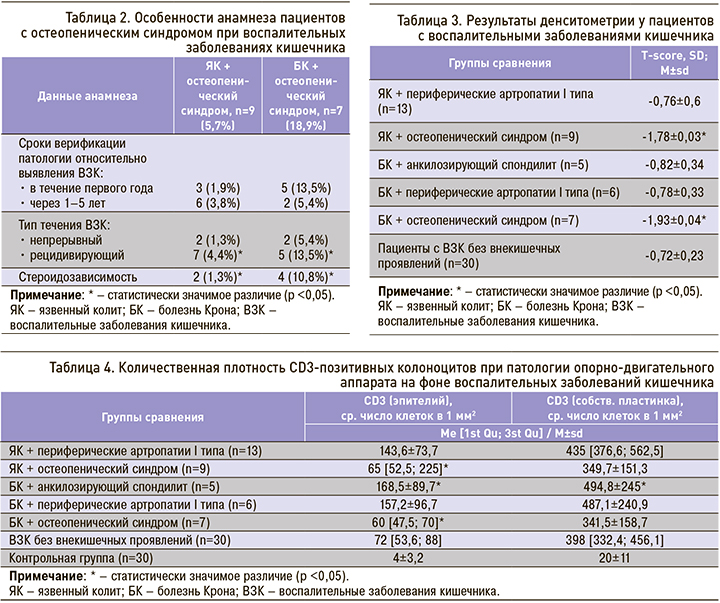
Одной из универсальных причин развития воспалительных и метаболических изменений при ВЗК могут быть иммунологические нарушения [29]. Для уточнения вклада степени иммунного воспаления в кишечнике в развитие патологии опорно-двигательного аппарата определялись морфометрические показатели CD3-позитивных колоноцитов эпителия и собственной пластинки СОТК (табл. 4).
У пациентов с анкилозирующим спондилитом на фоне БК количественная плотность CD3-позитивных колоноцитов эпителия и собственной пластинки толстой кишки значимо превышала значения в остальных анализируемых группах (r=0,44, р=0,036). Анкилозирующий спондилит при БК ассоциирован с повышением количественных показателей иммунного кишечного воспаления [30]. В нашем исследовании при артропатиях I типа у пациентов с ВЗК наблюдалось повышение количественной плотности колоноцитов эпителия и собственной пластинки толстой кишки, иммунопозитивных к CD3.
При остеопении на фоне ВЗК показатели количественной плотности CD3-позитивных колоноцитов эпителия толстой кишки были значимо меньше по сравнению с соответствующими значениями в других группах, однако выше, чем в группе контроля. Повышение количественной плотности CD3-позитивных колоноцитов эпителия и собственной пластинки толстой кишки при анкилозирующем спондилите на фоне БК можно объяснить антигенной общностью синовиальной оболочки и эпитопами измененного при ВЗК кишечного микробиома [31, 32].
ЗАКЛЮЧЕНИЕ
Патология опорно-двигательного аппарата выявлена у значительного числа пациентов с БК (48,6%) и у 14% больных с ЯК. У 2,5% пациентов с ЯК и 13,5% пациентов с БК заболевание кишечника манифестировало артропатией. Для периферических артропатий I типа у пациентов с ВЗК характерны неэрозивные изменения суставных поверхностей без деформации суставов, а также установленная связь с повышенным маркером иммунного кишечного воспаления – количественной плотностью CD3-позитивных колоноцитов. Максимальное повышение количественной плотности CD3-позитивных колоноцитов в эпителии и в собственной пластинке СОТК выявлено при анкилозирующем спондилите на фоне БК.
Остеопения была обнаружена у 5,7% пациентов с ЯК и 18,9% с БК. Факторами риска остеопении у пациентов с ЯК стали рецидивирующее течение заболевания с длительностью анамнеза 3–5 лет, стероидозависимость. При БК факторами риска остеопенического синдрома выступали терминальный илеит с длительностью анамнеза до одного года, рецидивирующее течение, стероидозависимость. При остеопеническом синдроме у пациентов с ВЗК отмечались повышенные значения показателей CD3-позитивных колоноцитов, что подтверждает роль иммунного воспаления в снижении МПКТ.