ВВЕДЕНИЕ
Несмотря на активное внедрение активных профилактических стратегий, число пациентов, перенесших сердечно-сосудистые катастрофы, остается высоким [1]. Широкое использование инвазивной коронароангиографии (ИКАГ) с транслюминальной балонной ангиопластикой (ТЛБАП) и инновационных медикаментозных подходов с ранних минут развития острого коронарного синдрома (ОКС) и при дальнейшем наблюдении за пациентами позволило снизить показатели смертности от инфаркта миокарда (ИМ) [2]. Тем не менее лица, перенесшие ИМ, вносят значительный вклад в когорту пациентов с хронической ишемической болезнью сердца (ИБС) и хронической сердечной недостаточностью (ХСН), смертность от которых удерживает лидирующие позиции среди всех причин у взрослого населения [3].
В период с 1998 по 2017 г. в России отмечено удвоение пациентов с сердечной недостаточностью (СН) – с 4,9 до 10,2%. Учитывая, что такой прирост произошел преимущественно за счет пациентов с тяжелой СН III–IV функционального класса (ФК) по NYHA, среднегодовой уровень смертности пациентов с ХСН в нашей стране составляет 6% [4]. Более ранний дебют заболеваний, связанных с атеросклерозом, и их более агрессивное течение с развитием ХСН наблюдается у лиц с сахарным диабетом (СД), распространенность которого приобретает характер пандемии [5]. Только за последние 15 лет опубликовано более 11 000 научных статей, посвященных патогенезу и лечению ХСН у больных с СД, а также течению диабета при ХСН. В России, по данным регистра СД, к началу 2022 г. на диспансерном учете состояло 4,5 млн пациентов с СД 2-го типа и около 374 тыс. пациентов с другими типами диабета (СД 1-го типа, гестационный диабет и др.) [6, 7]. Данные исследований по развитию микро- и макрососудистых осложнений при СД свидетельствуют об эндотелиальной дисфункции как раннем маркере развития атеросклероза еще на этапе предиабета за несколько лет до установления диагноза СД [8]. Развитие диабетического континуума от предиабета до клинической манифестации СД демонстрирует появление ретинопатии, ангиопатии различных локализаций, макрососудистых осложнений уже по прошествии 5 и более лет с момента фиксации изменений углеводого обмена [9].
Полученные в исследованиях DAPA-HF и EMPEROR-Reduced неоспоримые доказательства тесного взаимодействия сердечно-сосудистых событий и СД позволили активно внедрить в терапию ХСН с низкой фракцией выброса препараты из класса ингибиторов натрий-глюкозного котранспортера 2-го типа (иНГЛТ-2), которые могут применяться в этом случае независимо от наличия СД. Более того, активно обсуждается вопрос о возможности их использования в терапии ХСН с промежуточной и сохранной фракцией выброса также независимо от наличия СД [10].
Проведя предварительный анализ существующих данных, мы поставили целью нашего исследования оценку состояния функции левого желудочка (ЛЖ) и уровня предшественника мозгового натрийуретического пептида (NTproBNP) у пациентов с диагнозом ОКС в первые сутки госпитализации в стационар и через 6 мес наблюдения в зависимости от наличия СД и вариантов используемой терапии.
МАТЕРИАЛ И МЕТОДЫ
В исследование было включено 100 пациентов, госпитализированных в РСЦ Владивостокской клинической больницы № 1, с диагнозом ОКС в возрасте от 35 до 65 лет. Основными критериями включения в исследование были впервые установленный диагноз инфаркта миокарда с подъемом сегмента ST (ИМпST / инфаркт миокарда без подъема сегмента ST (ИМбпST) / нестабильная стенокардия (НС) с наличием СД 2-го типа менее 5 лет или без него.
Критериями исключения из исследования служили длительность СД 2-го типа более 5 лет, СД 1-го типа, наличие в анамнезе ранее перенесенного ОКС и/или острого нарушения мозгового кровообращения (ОНМК) и/или вмешательства на коронарных артериях, документированная хроническая болезнь почек IV стадии и более, поражение периферических артерий, онкологические заболевания различной давности и тяжелые заболевания печени.
Все участники исследования подписали информированное согласие, разрешающее использование анонимно собранных данных. Исследование было одобрено решением этического комитета ФГБОУ ВО «Тихоокеанский государственный медицинский университет» Минздрава России (протокол от 15 марта 2021 г. № 17).
Всем пациентам были выполнены лабораторно-инструментальные методы диагностики ОКС, включающие электрокардиографию (ЭКГ), эхокардиографию (ЭхоКГ), ИКАГ, а также определение в первые часы поступления в стационар маркера повреждения миокарда (TрI) и N-терминального фрагмента мозгового натрийуретического пептида (NT-proBNP) в качестве показателя увеличения давления в ЛЖ и/или его сократительного потенциала. При повторном визите пациентов через 6 мес были проведены ЭхоКГ и оценка содержание NT-proBNP в сыворотке крови.
Статистическая обработка данных осуществлялась с помощью программы StatTech v. 2.7.1. Категориальные данные описывались с применением абсолютных значений и процентных долей, количественные показатели – посредством медианы (Me) и нижнего и верхнего квартилей [Q1; Q3]. Сравнение двух групп по количественному показателю выполнялось с использованием критерия U Манна–Уитни. Направление и теснота корреляции между двумя количественными показателями оценивались через коэффициент ранговой корреляции Спирмена (ρ). Критическое значение уровня статистически значимых различий (p) принимали равным 0,05.
РЕЗУЛЬТАТЫ
В результате обследования пациентов при поступлении в стационар было установлено, что пациенты с СД 2-го типа были старше, чем пациенты без него, и среди них преобладали женщины (p <0,001; табл. 1). Пациенты с ОКС вне зависимости от наличия или отсутствия СД 2-го типа имели более высокие значения систолического (САД) и диастолического (ДАД) артериального давления в сравнении со здоровыми добровольцами, которые, однако, не выходили за пределы рекомендованных показателей.

Анализ состояния фракции выброса (ФВ) ЛЖ при госпитализации пациентов в зависимости от вариантов ОКС показал статистически значимые различия между ними (рис. 1). Так, медиана (Ме) значений исходной ФВ ЛЖ в группе ИМпST была наиболее низкой и составила 47%, что оказалось статистически значимо ниже, чем у пациентов с ИМбпST и НС, где этот параметр был равен 52 и 55% соответственно (p=0,002).

При разделении всех пациентов в зависимости от наличия СД у участников исследования с этим заболеванием была выявлена более низкая ФВ ЛЖ по сравнению с больными без СД – 48 против 56% (p <0,001). Результаты более детального анализа ФВ ЛЖ в зависимости от клинического варианта ОКС, наличия СД и содержания NTproBNP в сыворотке крови при поступлении пациентов в стационар и через 6 мес наблюдения представлен в таблице 2.
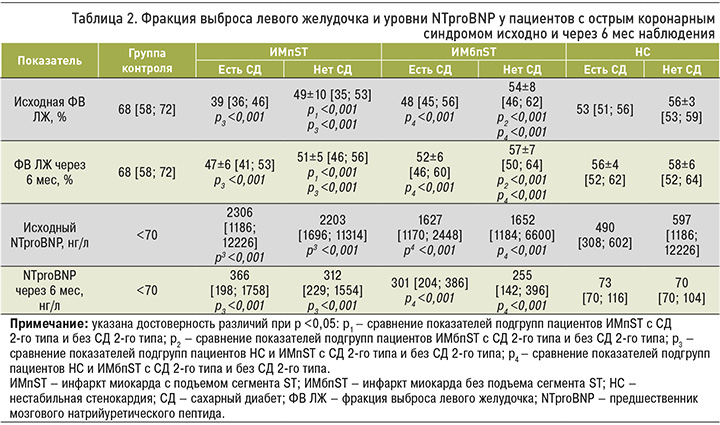
Как и ожидалось, наиболее низкие значения ФВ ЛЖ при поступлении в стационар наблюдались у пациентов с ИМпST в сочетании с СД. При анализе этого параметра у пациентов с ИМбпST его значения в группе лиц с СД также оказались ниже, чем у больных без СД – 48 против 54±8% (р <0,001). Пациенты с нестабильной стенокардией не имели значимых различий в величине ФВ ЛЖ в зависимости от наличия/отсутствия СД, и в целом по группе ее значения были близки к уровню сохранной ФВ ЛЖ, т.е. попадали в диапазон более 50%.
При анализе содержания NTproBNP при госпитализации (см. табл. 2) было выявлено его превышение относительно нормативных значений (>125 нг/л) во всех группах обследованных, включая пациентов с нестабильной стенокардией. Однако максимальное повышение уровня NTproBNP, как и ожидалось, наблюдалось у пациентов с ИМ, с наибольшими значениями в подгруппе ИМпST. В отличие от ФВ ЛЖ различий по этому показателю в подгруппах лиц с различными клиническими вариантами ОКС в зависимости от наличия СД обнаружено не было (p=0,94).
Нами была сделана попытка проанализировать наличие взаимосвязей между показателями ФВ ЛЖ и уровнем NTproBNP в период госпитализации пациентов, т.е. в первые сутки развития ОКС. Несмотря на изменение показателей ФВЛЖ и повышение содержания NTproBNP, статистически значимых взаимосвязей выявлено не было (ρ=0,2, р=0,020). Очевидно, в ранний период развития сердечно-сосудистого события на повышение уровня NTproBNP влияют и другие факторы, в частности неустойчивые показатели гемодинамики, повышение содержания соединений, связанных с активацией ренин-ангиотензин-альдостероновой системы (РААС), активацией системы эндотелина, избыточным синтезом ряда провоспалительных цитокинов и др., которые невозможно учесть при построении прямой линейной зависимости [11].
Нами установлено увеличение ФВ ЛЖ у лиц, перенесших ИМ, спустя 6 мес наблюдения по сравнению с исходными значениями, однако в группе лиц с нестабильной стенокардией статистически значимых различий по этому параметру обнаружено не было (рис. 2).
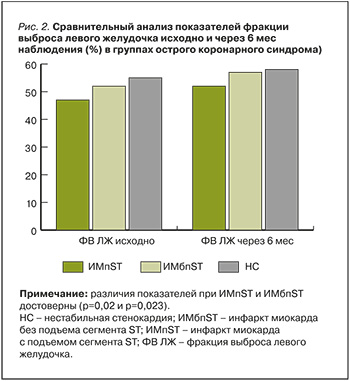
При детальном анализе было определено, что у всех пациентов через 6 мес ФВ ЛЖ превышала 40% (см. табл. 2). При сравнении ФВ ЛЖ между подгруппами пациентов, перенесших различные варианты ОКС, установлено статистически значимое снижение этого показателя у лиц с СД после ИМпST относительно других подгрупп, который достиг уровня 47±6% (р <0,001).
При повторном определении NTproBNP через 6 мес наблюдения было выявлено значительное его снижение во всех подгруппах пациентов по сравнению с исходными показателями (см. табл. 2). Уровень этого маркера достиг рекомендованных значений у пациентов, перенесших нестабильную стенокардию, в то время как у лиц после ИМпST и ИМбпST он оставался повышенным, без различий в подгруппах в зависимости от наличия СД (p=0,196).
В отличие от периода госпитализации, нами прослежена тесная обратная связь между ФВ ЛЖ и NTproBNP через 6 мес наблюдения. В соответствии с полученными результатами (рис. 3) можно прогнозировать снижение уровня NTproBNP на 45,9 нг/л при увеличении ФВ ЛЖ на 1% спустя 6 мес после развития ОКС (ρ=0,4; р=0,002).

Исходя из целей исследования, были проанализированы показатели ФВ ЛЖ и NTproBNP в зависимости от вариантов используемой терапии. Группа пациентов с нестабильной стенокардией была исключена из анализа в силу наличия сохранной ФВ ЛЖ в период госпитализации и отсутствия ее статистически значимого увеличения спустя 6 мес наблюдения. Также в этой группе отмечались наименьшее содержание NTproBNP в первые часы болезни и полная нормализация показателей к 6-му месяцу наблюдения, которое в большинстве случаев достигло рекомендованных значений при выписке. Всем больным с нестабильной стенокардией при выписке была рекомендована терапия, включающая дезагрегантную и гиполипидемическую терапию, а также ингибиторы АПФ, бета-блокаторы. Кроме того, при наличии СД назначались иНГЛТ-2.
Кроме того, были изучены показатели ФВ ЛЖ и NTproBNP у пациентов, перенесших ИМ. Всем больным из когорты с низкой ФВ ЛЖ (<40%) (n=20), которая состояла из лиц с ИМпST и ИМбпST, при выписке, помимо дезагрегантной и гиполипидемической терапии, была рекомендована квадротерапия ХСН, включающая иНГЛТ-2, бета-блокаторы, антагонисты минералокортикоидных рецепторов и РААС. В этой группе исходная ФВ ЛЖ составила 38% [32; 39], через 6 мес ее показатели достигли 45% [38; 47]; ΔФВ ЛЖ равнялась 7% (р=0,003). Исходный уровень NTproBNP в этой же группе составил 9431 нг/л [1708; 28 000], спустя 6 мес было обнаружено его снижение до 1623 нг/л [251; 6700]; ΔNTproBNP была равна 7808 нг/мл (р <0,001). Иными словами, все пациенты, перенесшие ИМпST и имевшие сниженную ФВ ЛЖ на фоне рекомендованной терапии через 6 мес, имели промежуточную ФВ ЛЖ и значительное уменьшению уровня NTproBNP.
Пациентам с ИМ, имевшим ФВ ≥40%, в случае СД (n=16) при выписке, кроме дезагрегантной и гиполипидемической терапии, назначалась терапия бета-блокаторами, ингибиторами РААС и иНГЛТ-2. В подгруппе пациентов с ИМ и без СД, имевших ФВЛЖ >40% (n=30), иНГЛТ-2 в протоколах лечения отсутствовали.
При детальном рассмотрении двух указанных групп была установлена следующая динамика изучаемых показателей. Лица с СД имели исходный уровень ФВ ЛЖ в диапазоне 49,78% [43; 60], спустя 6 мес – 54,3% [47; 62], ΔФВЛЖ составила 4,5% (р=0,0019). Исходный уровень NTproBNP в этой же группе был 5716,6 нг/л [600; 22711], через 6 мес – 803,8 нг/л [182; 3124], ΔNTproBNP достиг 4912,8 нг/мл (р <0,001). 5 пациентов из этой группы с промежуточной ФВЛЖ [44; 48] перешли в группу с сохранной ФВ ЛЖ [50; 54]. Лица, перенесшие ИМ, в отсутствие СД имели исходную ФВ ЛЖ 51,1% [42; 59], через 6 мес – 53,9% [48; 60], ΔФВЛЖ – 2,8% (р <0,001). В этой же группе исходный уровень NTproBNP составил 3817,5 нг/л [708; 12000], через 6 мес – 433,6 нг/л [70; 2299], ΔNTproBNP – 3383,9 нг/мл (р <0,001). Также в этой группе 5 пациентов с промежуточной ФВ ЛЖ [45; 49] перешли в категорию с сохранной ФВ ЛЖ [50; 54].
Мы провели сравнение прироста ФВ ЛЖ во всех 3 подгруппах с различными вариантами терапии: статистически значимых различий по величине этого показателя обнаружено не было (р=0,368). Такая же картина наблюдалась и в отношении снижения NTproBNP: статистически значимых различий в 3 подгруппах не наблюдалось (р=0,368). Таким образом, соблюдение рекомендованной терапии способствует повышению ФВ ЛЖ у всех пациентов, перенесших ИМ. При этом спустя 6 мес отсутствуют пациенты со сниженной ФВ ЛЖ, и увеличивается число лиц с промежуточной и с сохранной ФВ ЛЖ.
ОБСУЖДЕНИЕ
СД имеет большое значение в развитии атеросклероза, при этом особый интерес вызывают лица с недавним анамнезом СД, у которых острые сосудистые катастрофы могут быть дебютом как самого диабета, так и следствием развития макроангиопатий [12]. В наше исследование вошли пациенты с впервые возникшими сердечно-сосудистыми катастрофами в виде ИМпST, ИМбпST и нестабильной стенокардией, половина из которых имела СД с продолжительностью заболевания менее 5 лет. Установлено, что у лиц с ИМ и СД было статистически значимое снижение ФВ ЛЖ, они исходно имели более низкие значения этого показателя и более высокий уровень NTproBNP. Полученные различия можно объяснить наличием микро- и макроангиопатий, которые не были документированы при предшествующем наблюдении, а также, возможно, вкладом предиабета в риск сосудистых повреждений при развитии диабетического континуума продолжительностью от 5 до 10 лет [13, 14]. В отличие от пациентов с ИМ, при сравнении показателей ФВ ЛЖ и уровня NTproBNP у больных с нестабильной стенокардией значимых различий этих параметров в зависимости от наличия СД обнаружено не было. Очевидно, эта группа лиц нуждается в тщательном наблюдении с целью дальнейшей профилактики развития более тяжелых сосудистых катастроф.
Всем пациентам в нашем исследовании в зависимости о наличия СД и показателя ФВ ЛЖ была назначена терапия в соответствии с существующими клиническими рекомендациями и зарегистрированными показаниями к применению лекарственных средств. При этом у пациентов с ФВ ЛЖ <40% вне зависимости от наличия СД применялась квадротерапия, в том числе с использованием препаратов класса иНГЛТ-2. При промежуточной и сохранной ФВ ЛЖ у лиц с СД эти препараты также включались в комплексное лечение.
В течение 6 мес у исследуемых оценивалось соблюдение рекомендованной терапии (приверженность лечению), пациенты наблюдались у врача-кардиолога. По прошествии 6 мес во всех подгруппах было зарегистрировано увеличение ФВ ЛЖ у пациентов с ИМпST и СД, с ИМбпST и СД, также у больных с ИМбпST без СД. При этом ФВ ЛЖ превышала 40%.
Исходя из полученных данных, можно констатировать, что рекомендованная терапия способствует увеличению ФВ ЛЖ у всех групп пациентов, перенесших ОКС, способствует исчезновению низкой ФВ ЛЖ, а также увеличению лиц с промежуточной и сохранной ФВ ЛЖ.
Не было получено статистически значимых различий во всех 3 исследованных подгруппах в показателях ΔФВЛЖ и ΔNTproBNP, несмотря на кажущиеся различия.
ЗАКЛЮЧЕНИЕ
У пациентов с ИМ и небольшим анамнезом СД (до 5 лет) наблюдается статистически более значимое снижение ФВ ЛЖ и повышение уровня NTproBNP по сравнению с лицами без СД.
Использованная терапия в лечении пациентов, перенесших ОКС, соответствующая клиническим рекомендациям в зависимости от ФВ ЛЖ и наличия СД, способствовала статистически значимому повышению ФВ и снижению NTproBNP спустя 6 мес наблюдения. Более того, через 6 мес приема рекомендованной терапии в нашем исследовании отсутствовали пациенты с низкой ФВ ЛЖ на фоне значительного увеличения количества пациентов с промежуточной и сохранной ФВ ЛЖ.
Ограничения исследования. К ограничениям выполненного исследования можно отнести небольшую выборку пациентов и отсутствием более длительного (>6 мес) наблюдения за ними, что будет учтено на последующем этапе нашей работы.



