СОСТАВ РАБОЧЕЙ ГРУППЫ ПО РАЗРАБОТКЕ И ПЕРЕСМОТРУ КЛИНИЧЕСКИХ РЕКОМЕНДАЦИЙ:
Лазебник Л.Б. (ФГБОУ ВО «Московский государственный медицинский стоматологический университет им. А.И. Евдокимова» Минздрава России), Туркина С.В. (ФГБОУ ВО «Волгоградский государственный медицинский университет» Минздрава России), Ардатская М.Д. (ФГБУ ДПО «Центральная государственная медицинская академия» Управления делами Президента Российской Федерации, г. Москва), Остроумова О.Д. (ОСП «Российский геронтологический научно-клинический центр», ФГБОУ ВО «Российский национальный исследовательский медицинский университет им. Н.И. Пирогова» Минздрава России, г. Москва; ООО «Российская ассоциация геронтологов и гериатров», г. Москва), Голованова Е.В. (ФГБОУ ВО «Московский государственный медицинский стоматологический университет им. А.И. Евдокимова» Минздрава России), Комиссаренко И.А. (ФГБОУ ВО «Московский государственный медицинский стоматологический университет им. А.И. Евдокимова» Минздрава России), Корочанская Н.В. (ФГБОУ ВО «Кубанский государственный медицинский университет» Минздрава России, г. Краснодар), Козлова И.В. (ФГБОУ ВО «Саратовский государственный медицинский университет им. В. И. Разумовского» Минздрава России), Успенский Ю.П. (ФГБОУ ВО «Санкт-Петербургский государственный педиатрический медицинский университет (СПбГПМУ)» Минздрава России), Фоминых Ю.А. (ФГБОУ ВО «Первый Санкт-Петербургский государственный медицинский университет им. акад. И.П. Павлова» Минздрава России), Левченко С.В. (ФГБОУ ВО «Московский государственный медицинский стоматологический университет им. А.И. Евдокимова» Минздрава России), Лоранская И.Д. (ФГБОУ ВО «Первый Санкт-Петербургский государственный медицинский университет им. акад. И.П. Павлова» Минздрава России), Ткаченко Е.И. (ФГБОУ ВО «Северо-Западный государственный медицинский университет им. И.И. Мечникова» Минздрава России, г. Санкт-Петербург), Ситкин С.И. (ФГБОУ ВО «Северо-Западный государственный медицинский университет им. И.И. Мечникова» Минздрава России, г. Санкт-Петербург), Бакулин И.Г. (ФГБОУ ВО «Северо-Западный государственный медицинский университет им. И.И. Мечникова» Минздрава России, г. Санкт-Петербург), Бакулина Н.В. (ФГБОУ ВО «Северо-Западный государственный медицинский университет им. И.И. Мечникова» Минздрава России, г. Санкт-Петербург), Шемеровский К.А. (ФГБНУ «Институт экспериментальной медицины», г. Санкт-Петербург)
СПИСОК СОКРАЩЕНИЙ:
- ЖКТ – желудочно-кишечный тракт
- ПЭГ – полиэтиленгликоль
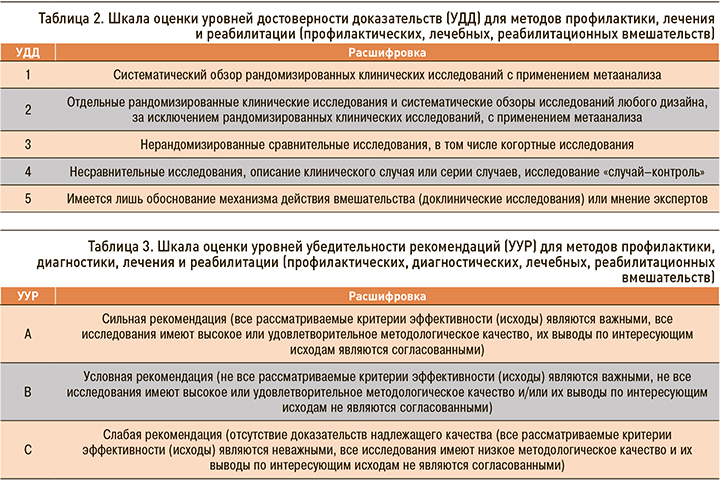
- УДД – уровень достоверности доказательств
- УУР – уровень убедительности рекомендаций
- ХЗ – хронический запор
1. ТЕРМИНЫ И ОПРЕДЕЛЕНИЯ
Термин «запор», или «констипация», происходит от латинского constipatio (синоним – obstipatio), что дословно означает «скопление».
Хронический запор (ХЗ) – это одна из актуальных проблем человека, по поводу которой пациенты обращаются к врачам всех специальностей: общей практики, терапевтам, гастроэнтерологам, кардиологам, эндокринологам, хирургам, гериатрам и др.
Согласно Римским критериям запора (Римский консенсус IV, 2016) по проблемам функциональных заболеваний желудочно-кишечного тракта (ЖКТ), запоры характеризуются следующими симптомами:
- менее 3 дефекациямй в неделю;
- отделением кала большой плотности;
- отсутствием ощущения полного опорожнения кишечника после дефекации;
- наличием чувства «блокировки» содержимого в прямой кишке при потугах;
- необходимостью в сильных потугах;
- необходимостью пальцевого удаления содержимого из прямой кишки, поддержки пальцами тазового дна и др. [1].
Для ХЗ характерны постоянные нарушения акта дефекации продолжительностью не менее 3 мес.
2. КРАТКАЯ ИНФОРМАЦИЯ
2.1. Национальное определение
Запор – это удлинение интервалов между актами произвольной дефекации до 72 ч и более, сопровождающееся, как правило, комплексом симптомов в виде изменения формы и консистенции каловых масс (твердый, фрагментированный кал – 1-й и 2-й типы по Бристольской шкале; рис. 1), ощущением неполного опорожнения кишки, необходимостью избыточного, нередко бесполезного, натуживания, а также приобретающего характер зависимости приема слабительных препаратов или проведения манипуляций, облегчающих достижение акта дефекации (клизмы, трансанальное или трансвагинальное ручное пособие и т.п.).

Условиями развития запора являются невозможность (ситуационная), нежелание (подавление позывов) или неспособность (физиологическая) осуществления акта произвольной дефекации.
2.2. Этиология и патогенез хронических запоров
Запор – полиэтиологическое заболевание. В зависимости от непосредственных причин и способствующих факторов запоры разделяют на первичные, вторичные и идиопатические [2].
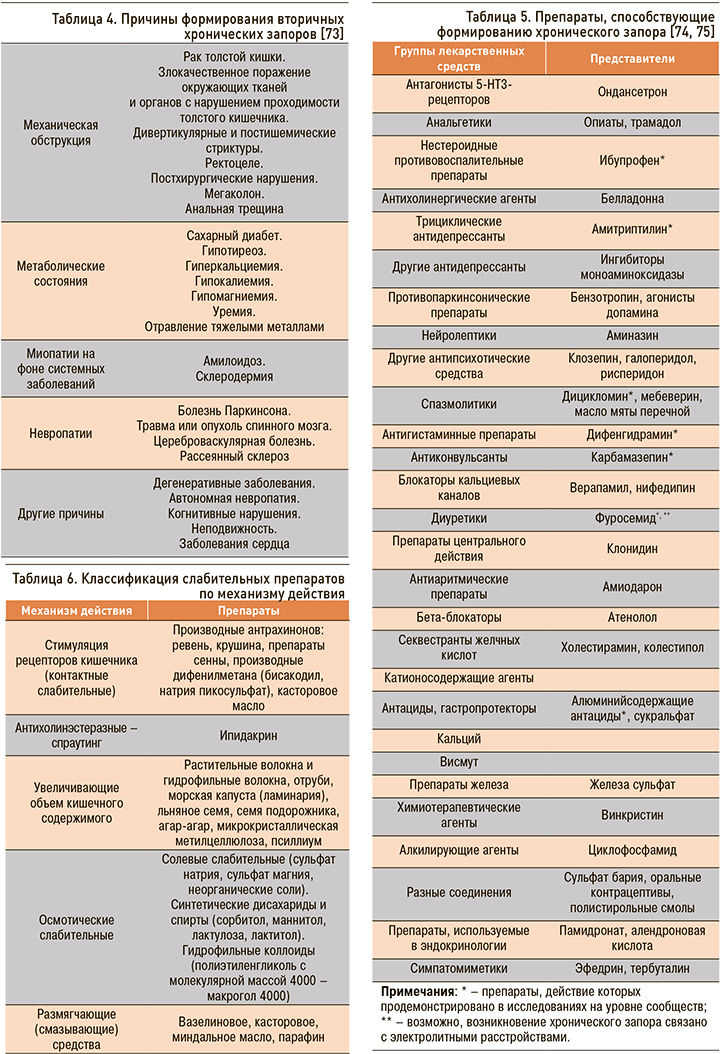
К первичным запорам относятся аномалии и пороки развития толстой кишки и ее иннервации (долихосигма, долихоколон, мегаколон, синдром Пайра, синдром Хилайдити, болезнь Гиршспрунга), а также синдром раздраженного кишечника. Вторичные запоры развиваются как проявление заболеваний и повреждений толстой кишки (ректоцеле, анальная трещина, осложненный геморрой, выпадение прямой кишки, дивертикулит, ишемический колит и др.), метаболических, эндокринных расстройств, неврологических заболеваний (Приложение 2, табл. 4), могут быть опосредованы приемом лекарственных препаратов (Приложение 2, табл. 5), что связано с изменением физиологических функций толстого кишечника и физиологических основ акта дефекации под воздействием этих этиологических факторов.
В основе ХЗ при этом могут лежать различные механизмы, обусловленные соматическим заболеванием и способствующие формированию нарушений функции толстой кишки и/или таза/аноректальной функции (запор, обусловленный замедлением транзита; запор с нормальным транзитом; запор, вызванный нарушением акта дефекации) [3]. Нередко встречается сочетание или «перекрест» клинических форм, например сочетание запора с замедлением транзита и расстройств дефекации; сочетание запора с нормальным транзитом и заболеваниями толстого кишечника и т.д.
Физиологические основы функций толстого кишечника и патогенетические особенности формирования ХЗ как проявлений различных заболеваний представлены в Приложении 2.
Снижение объема потребляемой пищи и воды, уменьшение в рационе пищевых волокон, избыточное потреблении белков животного происхождения, сознательное подавлении акта дефекации, гиподинамия относят к алиментарно-поведенческим этиологическим причинам ХЗ. Дополнительными факторами риска вторичного ХЗ служат пожилой возраст и связанные с ним снижение двигательной активности кишечника, недостаток физической активности, трудности при жевании, возникающие у пожилых пациентов в связи с утратой зубов, неадекватным протезированием и т.д. [4–6].
2.3. Эпидемиология
Жалобы на хронические затруднения дефекации, снижение частоты опорожнения кишечника встречаются у 14–35% взрослых пациентов и учащаются с возрастом [7–8].
По данным исследований, ХЗ чаще встречаются у женщин, а тяжелый запор заметно чаще наблюдается у пожилых женщин по сравнению с мужчинами.
Эпидемиологические данные, полученные в 2010 г. (популяционное исследование «МУЗА»), [9] свидетельствуют о том, что в московской популяции утвердительно на прямой вопрос о запоре положительно ответили 34,3% респондентов, Римским критериям ХЗ соответствовали 16,5% взрослого населения Москвы. Причем два и более симптома запора достоверно чаще встречались у женщин – в 29,8% случаев (vs 14,3% у мужчин). Частота встречаемости ХЗ увеличивалась с возрастом (до 32,8% у лиц старше 65 лет). Были выявлены факторы, ассоциированные с ХЗ: факт родов (у женщин моложе 55 лет), низкий уровень потребления пищевых волокон и жидкости, пониженная физическая активность (у мужчин моложе 55 лет с повышенным индексом массы тела).
2.4. Кодирование по МКБ-10
На территории Российской Федерации диагноз выставляется по ведущему клиническому заболеванию, синдрому и/или симптому, соответствующему МКБ-10: К59.0 Запор.
2.5. Классификация хронических вторичных запоров
- Вторичный ХЗ, развившийся как следствие заболеваний и повреждения толстой кишки (ректоцеле, анальная трещина, осложненный геморрой, выпадение прямой кишки, дивертикулит, ишемический колит и др.).
- Вторичный ХЗ как следствие метаболических, эндокринных расстройств, неврологических нарушений, системных заболеваний.
- Вторичный ХЗ, опосредованный приемом лекарственных препаратов.
- Гестационный запор при беременности.
- Алиментарно-поведенческие запоры.
- Механический запор, развивающийся в результате сужения кишки спаечным, опухолевым, воспалительным процессом [2].
С учетом оценки времени транзита содержимого по кишечнику, а также состояния мышц тазового дна могут быть выделены группы больных ХЗ с преимущественно следующими механизмами его формирования:
- запором, обусловленным замедлением транзита;
- запором, вызванным нарушением акта дефекации (диссинергичная дефекация);
- запором с нормальным транзитом [10].
2.6. Клиническая картина хронического запора
При обычном, смешанном питании самым физиологичным ритмом опорожнения кишечника является ежедневный утренний стул без каких-либо затруднений (одномоментно, быстро и полностью), приносящий ощущение полноценного освобождения толстой кишки от содержимого [11].
Клиническая картина ХЗ складывается из симптомов урежения стула (частота дефекаций менее 3 раз в неделю), наличия чувства неполного опорожнения кишечника, затруднений при дефекации со скудным выделением, как правило, твердого и фрагментированного по типу «овечьего» содержимого кишечника. Более половины пациентов с ХЗ могут испытывать необходимость в интенсивном и длительном, а иногда и безрезультатном натуживании, ощущать неприятные, а подчас и болевые ощущения при дефекации. При этом именно жалобы на необходимость длительного натуживания и малорезультативная дефекация являются наиболее показательными и достоверными признаками запора (чувствительность 94%). Наряду с этим больные ХЗ могут также жаловаться на чувство вздутия кишечника, явления дискомфорта в области живота, чаще в нижней его части.
3. ДИАГНОСТИКА ХРОНИЧЕСКОГО ЗАПОРА
• Сбор жалоб и анамнеза – основной, необходимый и в большинстве случаев достаточный метод установления диагноза ХЗ.
Уровень убедительности рекомендаций A (уровень достоверности доказательств 2).
Комментарий: при опросе пациента уточняются:
- количество актов дефекации в течение недели;
- консистенция кала (наличие комков и/или твердый кал);
- наличие примесей (кровь, слизь, непереваренные фрагменты пищи) в кале;
- качество дефекации (ощущение препятствия или затруднения при ее совершении);
- необходимость в чрезмерном натуживании при дефекации;
- неудовлетворенность дефекацией (чувство неполного опорожнения кишечника);
- необходимость специфических манипуляций для облегчения дефекации.
Выявление клинических особенностей у каждого конкретного пациента имеет прямое значение для выбора дальнейшей лечебной тактики: например, пациенты с наличием эвакуаторных расстройств, как правило, практически не реагируют на применение стандартных программ лечения, и неспособность распознать этот компонент становится частой причиной неудачи последующей терапии.
• Цель сбора жалоб и анамнеза, физикального обследования – выявление приема пациентом лекарственных препаратов, сопутствующей патологии (сердечно-сосудистой, эндокринной, неврологической), акушерского анамнеза у женщин и т.д.
Уровень убедительности рекомендаций A (уровень достоверности доказательств 2).
Комментарий: прием лекарственных препаратов может сопровождаться формированием ХЗ [2, 12–13]. Поэтому в беседе с пациентом опросу о сопроводительной терапии других заболеваний должно уделяться большое внимание.
Следует отметить, что из эндокринологических заболеваний самыми частыми причинами ХЗ являются сахарный диабет и гипотиреоз, а из неврологических – болезнь Паркинсона и рассеянный склероз [14, 15].
• Сбор жалоб и анамнеза, проведение физикального обследования у пациента с ХЗ должны быть направлены на выявление тревожных признаков и симптомов.
Уровень убедительности рекомендаций A (уровень достоверности доказательств 2).
Комментарий: при сообщении пациентом о наличии крови в кале уже на этапе сбора жалоб и анамнеза у можно заподозрить колоректальный рак, дивертикулярную болезнь, воспалительные заболевания кишечника. Потеря веса более чем 4,5 кг и возникновение запоров в пожилом возрасте должны насторожить врача в отношении дальнейшего скрининга колоректального рака.
• При выявлении симптомов «тревоги» (гематохезия, железодефицитная анемия неясной этиологии, мелена при отсутствии патологии при эндоскопическом исследовании верхних отделов ЖКТ) пациенту должно быть проведено эндоскопическое исследование вне зависимости от возраста.
Уровень убедительности рекомендаций A (уровень достоверности доказательств 2).
Комментарий: колоноскопия позволяет исключить не только органическую патологию (опухолевое поражение, воспалительные заболевания). С помощью эндоскопического исследования можно диагностировать меланоз толстой кишки, являющийся результатом длительного применения слабительных препаратов антрахинонового ряда.
Залогом хорошей диагностики и успешного лечения патологии толстого кишечника является строгое следование правилам подготовки пациента к исследованиям (см. Приложение 2).
• Регулярное использование анализов крови, рентгенографии или эндоскопии у пациентов с запором, у которых нет симптомов тревоги, не рекомендуется.
Уровень убедительности рекомендаций A (уровень достоверности доказательств 2).
• При подозрении на наличие у пациента метаболических заболеваний, способствующих формированию ХЗ, рекомендуется проведение лабораторных тестов определения уровня глюкозы, тиреотропного гормона, кальция.
Уровень убедительности рекомендаций A (уровень достоверности доказательств 2).
• Исследование кала на скрытую кровь иммунохимическим методом у пациентов с ХЗ рекомендовано при подозрении на опухолевые заболевания толстого кишечника.
Уровень убедительности рекомендаций A (уровень достоверности доказательств 2).
• Проведение пальцевого ректального исследования с оценкой двигательной активности мышц тазового дна должно проводиться всем пациентам.
Уровень убедительности рекомендаций A (уровень достоверности доказательств 2).
Комментарий: при проведении ректального исследования возможна оценка прежде всего состояния кожи и слизистой перианальной области, выявление эскориаций, анальных трещин, геморроя. Пальцевое исследование прямой кишки служит ценным методом по оценке состояния тканей анального канала и замыкательной функции сфинктера заднего прохода, состояния окружающих прямую кишку органов и тканей, выявления ректоцеле.
Если это возможно, прием лекарственных препаратов, которые могут вызвать запор, следует прекратить перед дальнейшим мануальным обследованием (уровень убедительности рекомендаций A, уровень достоверности доказательств 3) [2]. Клиническая значимость этого исследования крайне важна: отсутствие анального рефлекса может свидетельствовать о патологии сакрального нерва, отсутствие реакции мышц тазового дна – о дисфункции мышц тазового дна, «утечка» каловых масс при проведении пальцевого исследования характерна для ректального пролапса, зияния ануса; боль, возникающая в момент проведения пальцевого исследования, часто связана с наличием анальной трещины [16, 17].
• При отсутствии эффекта от приема слабительных препаратов рекомендуется проведение аноректальной манометрии и теста изгнания ректального баллона.
Уровень убедительности рекомендаций B (уровень достоверности доказательств 2).
Комментарий: проведение аноректальной манометрии измеряет давление мышц анальных сфинктеров, чувствительность прямой кишки, исследуется нейрорефлекторная деятельность мышц заднего прохода, управляющая дефекацией, что позволяет получить информации о тонусе аноректального мышечного комплекса и скоординированности сокращений прямой кишки и сфинктеров ануса. Стандарты медицинской помощи, утвержденные Минздравсоцразвития России, определяют необходимость выполнения аноректальной манометрии у 100% пациентов, страдающих болезнью Гиршпрунга, мегаколоном [18–20].
Тест изгнания баллона рекомендуют для выявления нарушения синхронной деятельности мышц аноректальной зоны, участвующих в акте дефекации (диссинергия мышц тазового дна).
При получении неубедительных данных, свидетельствующих о наличии дефекационных расстройств у пациента с хроническим запором, обследование следует продолжить и провести дефекографическое исследование или рассмотреть возможность оценки транзита содержимого о толстой кишке (уровень убедительности рекомендаций B, уровень достоверности доказательств 2).
• Рентгенологический метод определения времени транзита содержимого по толстой кишке (метод рентгеноконтрастных маркеров) рекомендуют для верификации нарушений транзита по толстой кишке и тем самым определения преимущественного патофизиологического механизма развития запора.
Уровень убедительности рекомендаций B (уровень достоверности доказательств 2).
Комментарий: метод транзита рентгеноконтрастных маркеров является физиологичным и достаточно информативным методом изучения времени толстокишечного транзита, позволяющим оценить нарушение моторно-эвакуаторной функции кишечника, документировать степень и локализацию замедления транзита.
К лучевым методам диагностики относятся:
- дефекография. Позволяет диагностировать такие анатомические изменения, как ректоцеле, ректальная инвагинация, ректальный пролапс, сигмоцеле, опущение промежности [34];
- ирригоскопия с двойным контрастированием. Исследование позволяет исключить или выявить рак, полипы, дивертикулит, болезнь Крона и его осложнения, язвенный колит, ишемический и радиационный колит, болезнь Гиршпрунга. При исключении органической патологии оценивается расположение толстой кишки для исключения врожденного нарушения положения, фиксации (неполная ротация) и осложнений, которые могут быть вызваны ими: инвагинация, узлообразование, заворот. Оцениваются уровни расположения правого и левого изгибов, какие углы они образуют (деформация в виде «двустволки»). Исключаются врожденный или приобретенный долихо- и мегаколон или их сочетание [2].
При необходимости в алгоритм обследования могут быть включены компьютерная томография, динамическая магнитно-резонансная томография таза.
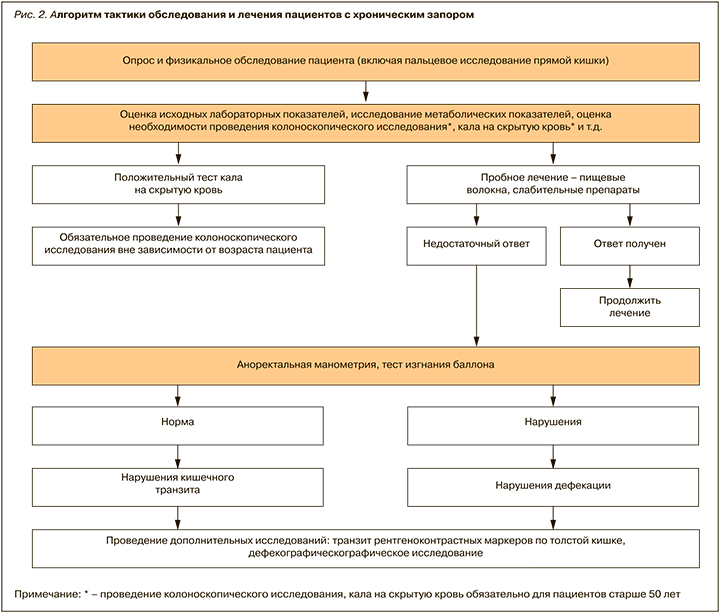
Алгоритм диагностики хронического запора представлен на рисунке 2.
4. ЛЕЧЕНИЕ ВТОРИЧНОГО ХРОНИЧЕСКОГО ЗАПОРА
• Лечение пациента с вторичным ХЗ складывается прежде всего из мероприятий по лечению заболеваний, выступающих этиологическим фактором вторичного ХЗ.
Уровень убедительности рекомендаций B (уровень достоверности доказательств 2).
• Вне зависимости от причины вторичного запора все пациенты должны осуществлять ряд мер немедикаментозного характера, включающих изменение образа жизни, диету с включением достаточного количества клетчатки (25–30 г в день), повышенное потребление жидкости (2–2,5 л в день).
Уровень убедительности рекомендаций A (уровень достоверности доказательств 2).
Комментарий: в рацион пациента должны включаться продукты, способствующие опорожнению кишечника, с минимальным употреблением продуктов, задерживающих опорожнение кишечника (Приложение 3).
Пищевые волокна, включаемые в рацион, могут быть представлены растворимыми и нерастворимыми. Нерастворимые волокна, которые содержатся в цельнозерновых продуктах, таких как пшеница, кукуруза и рис, увеличивают объем и смягчают стул, вес фекалий и уменьшают время прохождения кишечника при его нормальной функции. Растворимая клетчатка больше представлена в овсе, фруктах и овощах. Дополнительные эффекты, связанные с растворимой клетчаткой, связаны с понижением уровня холестерина глюкозы в крови. Принимая во внимание связанные с этим преимущества для здоровья, текущие рекомендации касаются 5 порций фруктов и овощей в день.
Увеличение содержания в пищевом рационе пищевых волокон, увеличивающих частоту дефекации у пациентов с запорами, может быть ограничено наличием метеоризма у пациента (уровень убедительности рекомендаций B, уровень достоверности доказательств 3).
Необходимо использовать мероприятия, направленные на усиление гастроцекального рефлекса, включающие необходимость приучить пациента пользоваться туалетом сразу же после первого приема пищи в течение дня, обычно после завтрака, если распорядок дня и характер работы позволяют осуществлять акт дефекации комфортно и без спешки.
Физические методы лечения ХЗ могут включать лечебную гимнастику (уровень убедительности рекомендаций B, уровень достоверности доказательств 3), прием минеральных сульфатных вод, массаж толстой кишки для стимуляции моторной активность кишечника в определенное время.
Метаанализ девяти рандомизированных контролируемых исследований с участием 680 участников по оценке влияния физических нагрузок показал, что физические упражнения имеют значительные преимущества как средство улучшения симптомов пациентов с запорами и могут быть возможным и эффективным вариантом лечения для пациентов с ХЗ. Однако реальный эффект этого вмешательства не может быть определен окончательно [21].
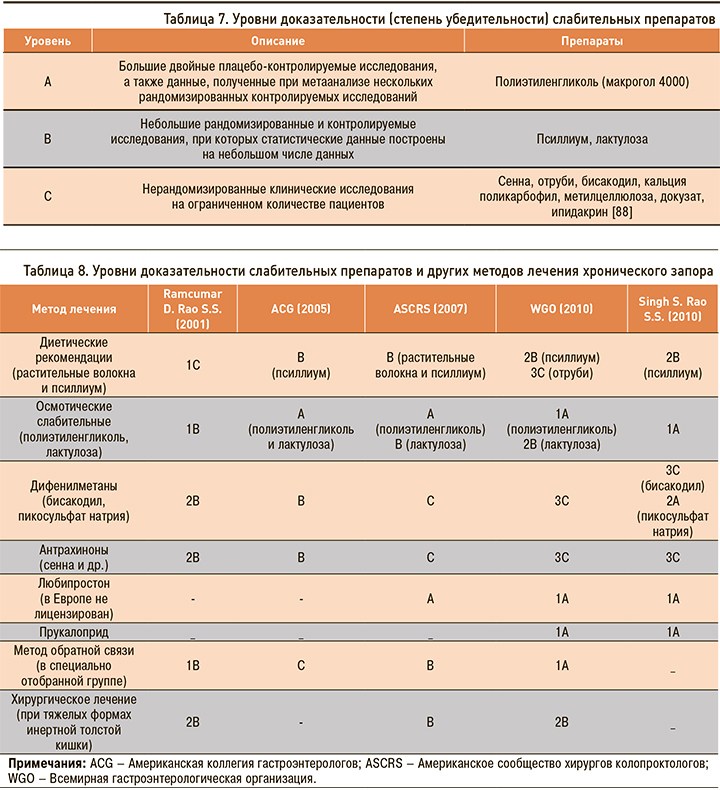
• При неэффективности немедикаментозных мероприятий рекомендуется использование осмотических слабительных, таких как макрогол 4000 (уровень убедительности рекомендаций A, уровень достоверности доказательств 1) и лактулоза (уровень убедительности рекомендаций A, уровень достоверности доказательств 2), средств, увеличивающих объем каловых масс (псиллиум, метилцеллюлоза, морская капуста, отруби, поликарбофил) (уровень убедительности рекомендаций A, уровень достоверности доказательств 2).
Комментарий: осмотические слабительные создают осмотический градиент в полости кишки и таким образом задерживают воду, поддерживая в полости кишечника изоосмотическое с плазмой давление. Задержка воды в кишечнике способствует размягчению каловых масс и улучшению их продвижения. Это средства, вызывающие увеличение объема каловых масс, не оказывающие раздражающего влияния на слизистую оболочку толстой кишки, не вызывающие привыкания.
Макрогол 4000 (полиэтиленгликоль) назначают в дозировке 10–20 г 1 раз/сут утром натощак во время или перед едой. Действие препарата начинается спустя 1–2 сут после приема. Продолжительность лечения определяется врачом. Полиэтиленгликоль (ПЭГ) предназначен не для однократного приема с целью достижения дефекации, а для планомерного и постепенного восстановления нормальной функции кишечника и его регулярного опорожнения. ПЭГ рекомендуется при ХЗ, особенно у пожилых людей, больных сахарным диабетом, артериальной гипертензией, почечной и печеночной недостаточностью, сердечно-сосудистыми заболеваниями [22].
Дозу лактулозы подбирают индивидуально. При лечении запоров взрослым обычно назначают от 15 до 45 мл препарата в первые 3 дня, потом переходят на поддерживающую дозу 10–25 мл. Препарат лучше принимать 1 раз каждый день утром во время еды.
Осмотические слабительные приемлемы для длительного использования (уровень убедительности рекомендаций A, уровень достоверности доказательств 1).
Обзор рандомизированных исследований, в которых сравнивался ПЭГ с лактулозой, показал, что ПЭГ демонстрирует лучшие результаты, касающиеся частоты и консистенции кала, и вызывает меньшее количество болей в животе [23].
Лактитол представляет собой полусинтетический дисахарид. Осмотическими свойствами обладает не само это лекарственное вещество, а продукты его метаболизма в толстой кишке с определенными видами бактерий, которые расщепляют сахара до уксусной, пропионовой и масляной кислот, вызывающих снижение внутрикишечного рН, что способствует активации пропульсивной перистальтики толстой кишки, увеличению объема кишечного содержимого и его разжижению.
Прием лактитола осуществляется во время еды 1 раз/сут, по 20 г порошка, который смешивают с различными напитками.
Доказана высокая эффективность псиллиума в лечении ХЗ, особенно у пожилых пациентов. Согласно результатам метаанализа, включавшего 31 исследование по изучению эффективности различных слабительных средств у лиц пожилого возраста, при назначении псиллиума ежедневного стула удалось добиться практически у всех больных. При этом по эффективности псиллиум не уступал ПЭГ, но значительно превосходил лактулозу [24].
Препараты подорожника, помимо увеличения объема стула в результате осмотического действия, оказывают размягчающее и смазывающее действие на содержимое кишечника за счет гельформирующей фракции, что облегчает пропульсию кишечного содержимого [25].
Принимать пищевые добавки лучше утром и на ночь с достаточным количеством воды (2–3 стакана в день дополнительно).
Все объемные агенты приемлемы для долгосрочного использования [26–29].
• Стимулирующие слабительные средства (сенна, бисакодил, производные пикосульфата натрия и антрахинона) могут быть использованы в случаях, когда использование немедикаментозных мероприятий и прием осмотических слабительных средства не принесли успеха.
Уровень убедительности рекомендаций A, уровень достоверности доказательств 2.
Комментарий: основное преимущество стимулирующих слабительных – быстрый механизм действия, при котором эвакуация кала происходит в среднем в течение 6–12 ч. Однако эти средства не лишены недостатков, главные из которых – снижение чувствительности к препарату и потеря терапевтического эффекта; стимулирующие слабительные обусловливают возникновение дегенеративных изменений клеток мейсснеровского и ауэрбаховского сплетений [30], что вызывает необходимость постоянно увеличивать дозы. Кроме того, они вызывают не нормальную дефекацию, а появление диареи со схваткообразными болями в животе и метеоризмом, часто приводят к развитию электролитных нарушений (гипокалиемия).
Следует помнить, что прием стимулирующих слабительных более двух недель не рекомендован (уровень убедительности рекомендаций A, уровень достоверности доказательств 1).
Препараты сенны назначаются внутрь натощак на ночь, по 2–4 таб.
Натрия пикосульфат применяют по 12–24 капли (5–10 мг) внутрь перед сном. Препарат перед использованием следует развести в небольшом количестве воды.
• Можно выделить следующие побочные эффекты, которые потенциально могут развиться на фоне любого слабительного препарата: диарея, дисбактериоз, дегидратация с гипокалиемией, нарушения ритма и проводимости, синдром экссудативной энтеропатии, синдром мальабсорбции, нефропатия, вторичный гиперальдостеронизм, аллергические реакции, волчаночноподобный синдром, остеопороз.
При этом существуют и побочные явления, развивающиеся при длительном применении отдельных групп слабительных препаратов. Например, известно, что бесконтрольный многолетний прием сенны в возрастающих дозах может привести к меланозу слизистой толстой кишки, для антрагликозидов и масляных слабительных характерно появление тошноты и рвоты, при применении слабительных в виде ректальных свечей пациентов часто беспокоит анальный зуд. Описано развитие аспирационной пневмонии и нарушение функции печени у пожилых лиц и у пациентов с дисфагией, находящихся на постельном режиме при приеме масляных слабительных.
Слабительные средства противопоказаны при острых воспалительных заболеваниях ЖКТ, наличии препятствий для нормального продвижения содержимого кишечника, острых лихорадочных состояниях. С осторожностью применяют их в период беременности и в старческом возрасте.
Классификация по механизму действия и определение уровней доказательности (степень убедительности) слабительных препаратов представлены в Приложении 2, таблицах 6 и 7.
• Пробиотики рекомендованы с целью восстановления кишечной микробиоты, увеличения частоты эвакуации, улучшения консистенции кала и уменьшения метеоризма.
Уровень убедительности рекомендаций B, уровень достоверности доказательств 3.
Комментарий: наиболее изученными бактериями являются Bifidobacterium lactis DN 173 010, Lactobacillus casei Shirota, VSL # 3 (смесь 8 различных штаммов) и E. coli Nissle 1917. В настоящее время, однако, отсутствуют научные доказательства, подтверждающие их пользу в лечении хронического идиопатического запора [31, 32].
Клизмы или суппозитории могут быть использованы в некоторых случаях, когда немедикаментозные мероприятия и прием слабительных были не эффективными. Использование этих методов должно быть ограничено короткими периодами, и агенты могут состоять из фосфата натрия или растительных масел.
• При недостаточной эффективности слабительных препаратов рекомендуется назначать прокинетики из группы агонистов 5-НТ4-рецепторов.
Уровень убедительности рекомендаций A, уровень достоверности доказательств 2.
Комментарий: прокинетический фармацевтический препарат прукалоприд (высокоселективный агонист рецептора 5-HT4) усиливает перистальтику и ускоряет кишечный транзит. Прукалоприд одобрен с 2009 г. в европейских странах для лечения ХЗ в тех случаях, когда слабительные средства не обеспечивают должного эффекта в устранении его симптомов (уровень убедительности рекомендаций A, уровень достоверности доказательств 1).
Препарат можно применять в дозе 2–4 мг/сут для лечения ХЗ у женщин, которые не реагируют на клетчатку и слабительные. Следует помнить, что прукалоприд противопоказан при нарушениях функции почек, требующих проведения диализа, обструкции кишечника вследствие анатомических или функциональных нарушений стенки кишечника, механической кишечной непроходимости, воспалительных заболеваниях кишечника. С осторожностью он должен назначаться пациенткам с соматической патологией: болезнями печени, легких, сердечно-сосудистыми, неврологическими, эндокринными заболеваниями, психическими расстройствами, онкологическими заболеваниями, с особой осторожностью при нарушениях сердечного ритма или ишемической болезни сердца в анамнезе [33].
• Назначение ингибиторов холинэстеразы рекомендовано в составе комбинированной терапии инертной толстой кишки вместе с осмотическими слабительными или прокинетиками.
Уровень убедительности рекомендаций B, уровень достоверности доказательств 3.
Комментарий: ипидакрин – обратимый ингибитор холинэстеразы. Он обладает двумя механизмами действия: блокирует ацетилхолинэстеразу, а также калиевые каналы мембран нейронов и мышечных клеток, что значительно удлиняет продолжительность действия ацетилхолина.
В клинической практике ипидакрин назначается коротким курсом, в течение 1–2 нед по 20 мг 2–3 раза/сут. Препарат противопоказан при эпилепсии, экстрапирамидных нарушениях с гиперкинезами, стенокардии, выраженной брадикардии, бронхиальной астме, вестибулярных нарушениях, обострениях язвы желудка или двенадцатиперстной кишки, механической непроходимости кишечника или мочевыводящих путей. С осторожностью назначают ипидакрин при язвенной болезни желудка и двенадцатиперстной кишки, тиреотоксикозе, заболеваниях сердечно-сосудистой системы, обструктивных заболеваниях дыхательной системы в анамнезе или острых заболеваниях дыхательных путей [88].
Метод биологической обратной связи (биофидбэк) используется для тренировки мускулатуры тазового дна с помощью специальных упражнений, которые способствуют расслаблению этой мускулатуры во время эвакуаторных усилий (уровень убедительности рекомендаций B, уровень достоверности доказательств 3). Для больных с замедлением транзита по ректосигмоидному отделу («обструкция выхода» или «обструктивная дефекация»), а также при наличии запоров вследствие диссинергии тазового дна основным методом лечения на сегодняшний день признана биофидбэк-терапия в двух основных разновидностях:
- биофидбэк-тренинг – мониторирование активности поперечных мышц или давления в анальном канале с обратной связью пациенту путем помещения сенсорных датчиков в анальный канал или непосредственно в области ануса;
- симулированная дефекация – тренировка дефекации с имитированным стулом.
Успех этого метода лечения в значительной мере определяется желанием больного закончить курс терапии и длительностью лечебных сессий.
Для лечения тяжелых запоров, рефрактерных к стандартной медикаментозной терапии, предлагается стимуляция крестцовых нервов – экспериментальная методика, заключающаяся в чрескожной стимуляции или даже временной имплантации электрода. Считается, что у пациентов с ответом на подобную терапию возможна длительная имплантация электродов. Методика представляется перспективной, но дальнейший опыт ее применения должен показать и оценить риски и выгоды данного лечения.
Кандидатами для хирургического лечения ХЗ являются пациенты с аномально удлиненным толстокишечным транзитом и нормальными показателями исследований тазового дна, рефрактерными к активной адекватной медикаментозной терапии [36].
5. МЕДИЦИНСКАЯ РЕАБИЛИТАЦИЯ
В качестве методов реабилитации пациентов с ХЗ могут использоваться санаторно-курортное лечение, физиотерапевтические методы лечения, прием послабляющих минеральных вод.
6. ПРОФИЛАКТИКА И ДИСПАНСЕРНОЕ НАБЛЮДЕНИЕ
Профилактика ХЗ у пациентов с системными заболеваниями предполагает мероприятия, направленные на лечение основного заболевания, рациональный режим питания с включением достаточного количества балластных веществ, прием достаточного количества жидкости, физическую активность.
7. ОРГАНИЗАЦИЯ ОКАЗАНИЯ МЕДИЦИНСКОЙ ПОМОЩИ
Организация оказания медицинской помощи проводится на основании Приказа Минздрава России от 12.11.2012 № 906н «Об утверждении порядка оказания медицинской помощи населению по профилю „Гастроэнтерология”» (зарегистрировано в Минюсте России 21 января 2013 г. № 2664).
8. КРИТЕРИИ ОЦЕНКИ КАЧЕСТВА МЕДИЦИНСКОЙ ПОМОЩИ
Медицинская помощь пациенту по профилю «Гастроэнтерология» осуществляется на основании Приказа Минздрава России от 12.11.2012 № 906н «Об утверждении Порядка оказания медицинской помощи населению по профилю „Гастроэнтерология”».
Критерии оценки качества медицинской помощи должны соответствовать Приказу Минздрава России от 10.05.2017 № 203н «Об утверждении критериев оценки качества медицинской помощи».
9. ПРИЛОЖЕНИЯ
Приложение 1. Методология разработки клинических рекомендаций
Данные клинические рекомендации разработаны для врачей первичного звена здравоохранения – врачей общей практики, терапевтов, гастроэнтерологов.
Разработка рекомендаций проводилась с учетом следующего нормативного документа: Приказа Минздрава России от 12.11.2012 № 906н «Об утверждении порядка оказания медицинской помощи населению по профилю „Гастроэнтерология”» (зарегистрировано в Минюсте России 21 января 2013 г. № 2664).
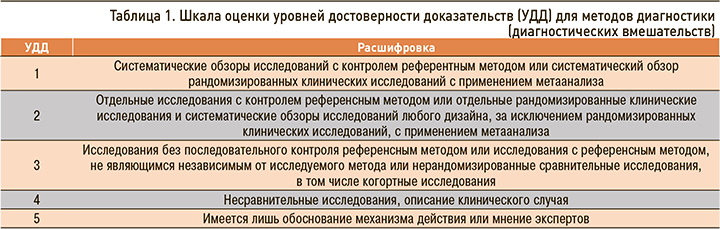
При создании рекомендаций использовались материалы, полученные в результате поиска по базам данных PubMed и Cochrane за 20 лет до сентября 2019 г. Все данные в рекомендациях приведены с указанием уровней достоверности доказательств (УДД) и уровня убедительности рекомендаций (УУР) для методов диагностики, профилактики, лечения и реабилитации (табл. 1–3) согласно Приложению № 2 к Требованиям к структуре клинических рекомендаций, составу и научной обоснованности включаемой в клинические рекомендации информации, утвержденным Приказом Минздрава России от 28.02.2019 № 103н «Об утверждении порядка и сроков разработки клинических рекомендаций, их пересмотра, типовой формы клинических рекомендаций и требований к их структуре, составу и научной обоснованности включаемой в клинические рекомендации информации».
Приложение 2. Справочные материалы
Физиологические основы функции толстого кишечника и патофизиология хронических запоров
Абсорбция воды. Толстый кишечник ежедневно получает приблизительно 1,5 л жидкого эффлюента из тонкой кишки. Функции толстой кишки состоят в том, чтобы абсорбировать жидкость и транспортировать каловые массы в прямую кишку, где они удаляются или хранятся до тех пор, пока дефекация не станет удобной. Удаление воды из фекальной суспензии зависит от времени пребывания каловых масс и активно регулируется, может существенно увеличиваться в состояниях дегидратации и при нарушениях водно-солевого обмена [37].
Двигательная активность кишечника определяет продвижение содержимого кишечника (повторяющиеся непропульсивные сокращения способствуют поглощению и смешиванию содержимого), а скоординированные высокоамплитудные сокращения [HAPCs] продвигают каловые массы от восходящего отдела толстой кишки до левого нисходящего отдела толстого кишечника [38]. Перистальтическая деятельность кишечника регулируется вегетативной нервной системой (внешняя регуляция), интрамуральными нервными структурами и действием нейропептидов (внутренняя регуляция). Растяжение стенки кишечника болюсом кала приводит к формированию локального рефлекса, опосредованного энтеральными нервами, при этом происходит высвобождение стимулирующих нейротрансмиттеров (например, ацетилхолина, который вызывает сокращение мышц) позади болюса и ингибирующих нейротрансмиттеров (такие как оксид азота, который вызывает расслабление мышц) перед болюсом; таким образом, болюс продвигается вперед по ЖКТ.
У здорового человека за ночь, как правило, происходит полный переход тонкокишечного содержимого в толстую кишку. Принятие вертикального положения и двигательная активность после пробуждения способствуют толстокишечному пассажу и переходу содержимого в прямую кишку. Поэтому дефекация чаще всего происходит в утренние часы. Кроме того, этому способствует гастроцекальный рефлекс – попадание пищи в желудок вызывает усиление толстокишечной перистальтики, достигающей прямой кишки [37]. У людей, оправляющихся в утренние часы (с 06:00 до 12:00), распространенность запоров составляет 10%; у тех же, кто оправляется позднее, запоры встречаются в 40%. У пациентов с запорами среднее время транзита колеблется от 67 до 120 ч.
В нормальных физиологических условиях прямая кишка здорового человека свободна от фекальных масс практически все время, за исключением тех моментов, которые предшествуют акту дефекации. В тот момент, когда человек ощущает первые позывы к дефекации, усиленная перистальтика толстой кишки проталкивает фекалии из сигмовидной кишки в прямую кишку. Позыв к дефекации сопровождается рефлексом сокращения прямой кишки и рефлекторным расслаблением анального сфинктера.
Акт дефекации возникает под влиянием специальных рефлексов. Первичный рефлекс является внутренним рефлексом, который реализуется за счет энтеральной нервной системы прямой кишки. В тот момент, когда фекальные массы перемещаются из переполненной сигмовидной кишки в прямую кишку, стенки последней растягиваются, что инициирует афферентные центростремительные импульсы, которые от гладких мышц прямой кишки распространяются по межмышечному нервному сплетению в центры дефекации. Это приводит к стимуляции перистальтических волн в трех участках толстой кишки: нисходящей ободочной, сигмовидной и прямой кишке. Такая перистальтика способствует проталкиванию фекальных масс в проксимодистальном направлении в сторону ануса. После того как перистальтика приблизится к анусу, внутренний анальный сфинктер под влиянием тормозных импульсов из межмышечного сплетения расслабится. Ощущение усиленного позыва к дефекации приводит к тому, что в это время наружный анальный сфинктер сознательно расслабляется и акт дефекации реализуется.
При гармоничном расслаблении внутреннего и наружного анальных сфинктеров возникает пропульсивный акт дефекации, который иногда реализуется за счет эффективной эвакуации практически всего дистального участка толстой кишки от селезеночного угла до ануса.
Сознательный компонент акта дефекации реализуется именно тогда, когда человеку это удобно. Акт дефекации может быть сознательно вызван путем реализации глубокого вдоха для опущения диафрагмы вниз, а также за счет сокращений мышц брюшного пресса с целью повышения уровня внутрибрюшного давления. В тех случаях, когда человек подавляет естественные позывы на дефекацию, возникает адаптация рецепторов прямой кишки к повышенному давлению, что при частом подавлении позывов приводит к возникновению хронических запоров. Это следует учитывать при проведении не медикаментозных лечебных мероприятий запора.
По Парфенову А.И. (2002) дефекация реализуется путем повышения внутрибрюшного давления под влиянием сокращения мышц брюшной стенки и опущения диафрагмы в процессе натуживания [39]. При этом происходит «отпирание» структур, ответственных за функцию держания кала: раскрываются «хлопающий» клапан и клапан-заслонка, а также расслабляются анальные сфинктеры. После реализации акта дефекации происходит быстрое повышение сократительной активности наружного анального сфинктера и мышц тазового дна. Это приводит к подниманию тазового дна и восстановлению аноректального угла.
В условиях, неблагоприятных для реализации акта дефекации, сознательное, произвольное сокращение наружного анального сфинктера приводит к подъему мышц тазового дна и увеличению аноректального угла. Эти сокращения приводят к возвращению фекальных масс в ампулу прямой кишки. Частое и повторно сознательное торможение акта дефекации может приводить к постепенной адаптации механорецепторов прямой кишки к повышению интраректального давления. Дефекационный рефлекс при таком поведении, а значит, и позыв к дефекации начнут возникать только лишь при более высоком (чем было ранее) интраректальном давлении. Такая адаптация рецепторов прямой кишки к повышению внутрипросветного давления может лежать в основе механизма формирования хронических запоров и так называемой инертной «ленивой» прямой кишки [39].
Подавление рефлекса на дефекацию очень широко распространено в цивилизованном мире.
Факторами, затрудняющими акт дефекации, что в итоге приводит к возникновению простого колоностаза, является недостаточная физическая активность, бесшлаковая диета с пониженным уровнем пищевых волокон, а также привычка к подавлению нормального позыва на дефекацию [40].
Не следует забывать, что важнейшей мерой профилактики нарушений акта дефекации и ХЗ служат элементарные гигиенические правила. Одним из основных этих правил считается соблюдение одного и того же (отработанного в течение многих лет) времени реализации акта дефекации. Желательно, чтобы акт дефекации обязательно реализовался в утренние часы после завтрака после всегда возникающего желудочно-прямокишечного рефлекса, способствующего физиологическому опорожнению кишечника. Время, когда реализуется акт дефекации, должно строго повторять в течение всей жизни современного человека.
С позиций хронобиологии и хрономедицины акт дефекации является проявлением циркадианного ритма жизнедеятельности организма человека. В нормальных физиологических условиях у здорового человека дефекация является ежедневной регулярной функцией с частотой не ниже 7 раз в неделю. Оптимальное время реализации акта дефекации или акрофаза ритма стула – это именно утренние часы (от пробуждения до полудня), так как порция фекалий, готовая к эвакуации из кишечника, готовится за период ночного сна. Как ночной сон, так и утренняя дефекация относятся к фундаментальным проявлениям циркадианного ритма жизнедеятельности организма человека [40].
Патогенетические особенности формирования хронического запора у пациентов с соматической патологией
Метаболические состояния
Первичный и вторичный гиперальдостеронизм. Формирование запора при первичном и вторичном гиперальдостеронизме связано с повышением активной реабсорбции натрия и пассивной (по осмотическому градиенту) реабсорбции воды эпителием кишечника, что сопровождается уплотнением каловых масс [41].
Сахарный диабет (СД). Нарушения опорожнения кишечника встречается у 60% больных СД, выступая наиболее частым проявлением диабетической энтеропатии [42–43], вплоть до развития картины «инертной толстой кишки». Диабетическая нейропатия способствует уменьшению ректальной чувствительности и/или нарушению функции внешнего сфинктера, что сопровождается симптомами ректальной дисфункции, такими как императивные позывы на дефекацию и чувство неполного опорожнения. Формирование диабетической нейропатии и нарушения автономной иннервации кишечника способствуют десинхронизации перистальтики кишечника и работы сфинктерного аппарата [42, 44]. Развитие моторных нарушений при диабетической энтропатии обусловлено уменьшением количества энтеральных нейронов [45] и генетической предрасположенностью [44] с уменьшением количества энтероглюкагон- и серотонин-иммунореактивных клеток и снижением секреции интестинальных гормонов и провоспалительных цитокинов. Другими предпосылками к развитию таких нарушений служит уменьшение продукции в кишечнике важнейшего нейротрансмиттера – нейронной окиси азота [46] и утрата «гастроколитического рефлекса» [42].
К факторам, ассоциированным с ХЗ у больных СД, относятся уровень гликированного гемоглобина ≥8,0%, индекс массы тела (ИМТ) <25 кг/м2, использование инсулина [47].
Гипотиреоз. Жалобы на редкий стул встречаются у 19–21% пациентов с гипотиреозом [48]. Отмечено, что патогенез запора при снижении функциональной активности тиреоидных гормонов связан, во-первых, со снижением двигательной активности не только толстого кишечника, но и дисмоторикой ЖКТ в целом [49–50]. Во-вторых, дефицит тиреоидных гомонов способствует метаболическим расстройствам и формированию отечности мышечного слоя кишечника за счет накопления гликозаминогликанов (преимущественно гиалуроновой кислоты). Отмечена важная роль тиреоидных гормонов в контроле и осуществлении эпителиального транспорта как одного из аспектов функционирования ЖКТ. Тиреоидные гормоны стимулируют активность Na+, K+-АТФазы и поглощение Na+ в эпителии кишечника, стимулируют активность апикальных, амилорид-чувствительных каналов Na+ в толстой кишке. Снижается активность мембранного транспортера Cl-/HCO3- [51], что также может способствовать формированию замедленной моторной активности кишечника. Тяжелый гипотиреоз может способствовать формированию динамической кишечной непроходимости и развитию мегаколона [52]. Следует отметить, что косвенным доказательством патогенетической роли гипотиреоза в формировании мегаколона служит положительный эффект заместительной терапии тиреоидными гормонами в отношении регресса кишечной симптоматики.
Акромегалия. Акромегалия – заболевание, обусловленное хронической гиперпродукцией гормона роста, может проявляться не только высокой частотой встречаемости запоров, но и распространенностью колоректальных полипов [53], рака толстого кишки [54], дивертикулярной болезни [55], долихосигмы [56]. Это может способствовать формированию ХЗ при акромегалии. В исследовании Renehan A.G. et al. [56] показано, что общая длина толстого кишечника у пациентов с акромегалией была увеличена на 20%, коррелируя с длительностью заболевания. Одной из причин запоров при акромегалии служит появление нарушений моторной функции кишечника, замедление кишечного транзита, а также появление добавочных петель кишечника [56].
Гиперпаратиреоз. Гиперпаратиреоз может манифестироваться не только симптомами нарушения опорожнения кишечника, которое встречается у четверти пациентов [57], но и другими желудочно-кишечными расстройствами. Пациенты предъявляют жалобы на снижение аппетита, тошноту, рвоту, боль в животе неясного характера; отмечается образование симптоматических язв желудка и двенадцатиперстной кишки. Причина формирования нарушений моторной функции при гиперпаратиреозе до конца не ясна. Высказано предположение о нарушении экспрессии генов, регулирующих сократительную активность кишечника, которое формируется в условиях постоянной гиперпродукции паратгормона. Показано, что у пациентов с уровнем кальция ≥11,2 мг/дл частота встречаемости запоров была достоверно ниже, чем у пациентов с уровнем кальция <11,2 мг/дл [58].
ХЗ у менопаузальных женщин. Частота встречаемости запоров у женщин в период менопаузы достигает 30–40%. В кросс-секционном исследовании женщин в постменопаузе в возрасте старше 45 лет в 91,9% случаев отмечено чрезмерное натуживание при дефекации; чувство неполной эвакуации отмечали 83,8% женщин с запорами, появление комковатого и твердого стула – 81,1%, а наличие менее трех актов дефекации в неделю – 62,2%. Отмечено, что 45,9% женщин с запорами использовали пальцевое пособие при акте дефекации [59]. Безусловно, основной причиной формирования запоров у женщин в этот период выступает активная гормональная перестройка организма. Гормоны яичников влияют на функцию ЖКТ, поскольку рецепторы эстрогенов обнаружены в слизистой оболочке желудка и кишечника. На тканевом уровне женские половые стероидные гормоны ингибируют мышечную сократимость, включая толстый кишечник. По мере снижения активности яичников исчезают периоды повышения уровня эстрогенов, отмечается снижение плотности ß-рецепторов к эстрогенам на клетках энтерального нервного сплетения [60], способствуя формированию аноректальных расстройств по типу обструкции при дефекации [61]. Высокий уровень прогестерон оказывает угнетающее влияние на перистальтику кишечника и способствует формированию запоров с замедленным транзитом.
Запоры при неврологических заболеваниях
Четверо из 10 пациентов с каким-либо неврологическим заболеванием страдают ХЗ, у 7 из 10 больных отмечается недержание кала. Более половины пациентов испытывают затруднения при дефекации, тратят более 30 мин на опорожнение кишечника и сообщают, что колоректальная дисфункция вызывает серьезные ограничения социальной активности [62]. Причиной тому могут быть как неврологические расстройства (поражение лобных долей, гипоталамическая вегетативная дисфункция, спинномозговые нарушения), так и полипрагмазия. Ряд препаратов сам по себе или в сочетании с неврологическим заболеванием способен вызвать или усугублять запор (диуретики, препараты железа, антигипертензивные, антипсихотические и антихолинергические средства, антациды, содержащие алюминий и кальций, противосудорожные средства, опиоидные анальгетики, ганглиоблокаторы).
Наиболее часто ХЗ встречается у пациентов с болезнью Паркинсона (по данным Американской гастроэнтерологической ассоциации OR=6,3 [2,6; 14,9]). Главной причиной этого является замедление кишечного транзита, связанное с нарушениями парасимпатической иннервации у данной категории пациентов. Реже имеют место нарушения опорожнения, связанные с диссинергией мышц тазового дна. Лекарственные препараты, используемые для лечения болезни Паркинсона, и прежде всего леводопа, могут усиливать проявления ХЗ [63]. Это связано с непосредственным замедлением двигательной активности толстого кишечника под действием норадреналина, образующегося в процессе метаболизма препарата.
Формирование запоров при болезни Паркинсона обусловлено также отсутствием достаточной двигательной активности, сокращением потребления клетчатки и жидкости из-за проблем с жеванием (брадикинезии) и дисфагии.
Второй по частоте неврологической патологией, при которой встречается ХЗ, является рассеянный склероз. При этом у 39–73% пациентов имеет место сочетание запора и недержания каловых масс [64]. Формирование расстройств дефекации складывается из нескольких патогенетических механизмов: замедления моторики кишечника и транзита каловых масс по кишечнику, нарушений в сочетании с аноректальными нарушениями, замедленного формирования условного рефлекса на акт дефекации или его утратой, потери контроля за анальными сфинктерами [65]. Аналогичные механизмы формирования ХЗ присущи пациентам с нарушениями функций спинного мозга, парасимпатической иннервации из крестцового сплетения, при автономной нейропатии на фоне СД (синдром кишечной псевдообструкции). Следует помнить, что в этой группе пациентов (при запоре с органической или функциональной обструкцией выхода и повреждениях спинного мозга) увеличенное содержание волокон в пище как метод немедикаментозного лечения в ряде случаев может спровоцировать формирование калового завала. Поэтому пищевые волокна должны рекомендоваться таким пациентам в постепенно возрастающей дозе, под контролем индивидуальной переносимости.
Другие причины формирования запоров
ХЗ при воспалительных заболеваниях кишечника. Как правило, при воспалительных заболеваниях кишечника нарушения стула представлены диарейным синдромом и лишь у 0,3% пациентов имеет место хронический запор. В случае язвенного колита запор появляется у пациентов при левостороннем процессе. При этом отмечается повышение скорости транзита каловых масс по нисходящему отделу толстого кишечника в связи с наличием воспалительных изменений и замедляется в той части кишечника, которая не вовлечена в воспалительный процесс («проксимальный запор») [66]. Еще одной из причин формирования запора у пациентов с воспалительными заболеваниями кишечника могут быть стриктуры, вызывающие нарушения продвижения каловых масс, а также анальные трещины. При наличии аноректальной патологии развивается запор по типу обструкции выхода, когда функциональная обструкция развивается как «защитная» антиболевая реакция. В этом случае пациенты задерживают позывы на дефекацию, опасаясь болезненности при прохождении каловых массы через прямую кишку, что и способствует формированию запоров [67].
У пациентов с болезнью Крона формированию запора может способствовать снижение содержание клетчатки в пище, прием некоторых лекарственных средств (например, препаратов железа). Однако следует помнить, что возникновение запора у пациента с болезнью Крона может быть первым симптомом осложненного течения заболевания, формирования стриктур и обструкции кишечника, а у оперированных пациентов – свидетельствовать о нарушении функционирования анастомоза. Это требует проведения дополнительного инструментального обследования пациента.
Запоры у пациентов с сердечно-сосудистыми заболеваниями
Вторичный анализ, проведенный среди 93 696 женщин в ходе наблюдательного исследования Women’s Health Initiative (средний срок наблюдения 6,9 лет), показал, что запором (по данным опросников самооценки) страдали 73 047 пациенток. Отмечено, что частота встречаемости запоров ассоциировалась с возрастом, курением, присутствием СД и ожирения, артериальной гипертензией, низкой физической активностью, высоким уровнем холестерина, низким потреблением клетчатки и депрессией. Оценка риска сердечно-сосудистых событий (включая смертность от ишемической болезни сердца, инфаркта миокарда, развитие стенокардии, потребность в коронарной реваскуляризаци, инсульт и транзиторную ишемическую атаку) продемонстрировала, что у пациенток со среднетяжелыми и тяжелыми запорами частота сердечно-сосудистых событий составила 14,2 и 19,1 события/1000 человеко-лет соответственно по сравнению с женщинами без признаков запора (9,6/1000 человеко-лет). После корректировки показателей с исключением демографических факторов, диетических погрешностей, приема лекарственных препаратов и других переменных сделан вывод, что в группе постменопаузальных женщин с тяжелыми проявлениями запора риск развития сердечно-сосудистых событий повышен на 23% [68].
В исследовании The Ohsaki cohort study (2016) проводилась оценка связи частоты дефекаций с риском развития сердечно-сосудистых событий. В исследовании приняли участие 45 112 мужчин и женщин, частота встречаемости неблагоприятных сердечно-сосудистых событий отдельно рассчитывалась для лиц с частотой дефекаций 1 раз в день, 1 раз в 2–3 дня, 1 раз в 4 дня. За 13,3 года наблюдения (490 086 человеко-лет) было зарегистрировано 2028 случаев смерти от сердечно-сосудистых заболеваний, в том числе 462 смерти от ишемической болезни сердца и 928 – от инсульта (геморрагический инсульт – 232, ишемический инсульт – 424, субарахноидальное кровоизлияние – 136 случаев). По сравнению с лицами, имевшими частоту дефекации 1 раз/день, риск общей смерти от сердечно-сосудистых заболеваний был значимо выше в группах с дефекацией 1 раз в 2–3 дня [1,21 (95% ДИ: 1,08–1,35)] и 1 раз в 4 дня [1,39 (95% ДИ: 1,06–1,81)] соответственно вне зависимости от пола и возраста [69]. Обсуждая отмеченную взаимосвязь неблагоприятных сердечно-сосудистых событий у пациентов в The Ohsaki cohort study, авторы выдвинули две гипотезы возникновения этой ассоциации: во-первых, роль напряжения при дефекации как причины развития геморрагического инсульта и субарахноидального кровоизлияния, так как показано, что затруднения при дефекации и натуживание служат факторами риска разрыва внутричерепных сосудов. Во-вторых, обсуждается роль замедленного транзита каловых масс как фактора риска кардиоваскулярной смертности. В обсуждении результатов The Ohsaki cohort study Gabrio Bassotti (2016) [70] пишет, что еще одной причиной может быть фекальная обструкция, что было продемонстрировано в ранее проведенных исследованиях.
Взаимосвязь частоты дефекации и риска развития сердечно-сосудистой и общей смертности обсуждалась в итогах 30-летнего наблюдения за женщинами Nurses’ Health Study (2016) [71]. Определение частоты было проведено в 1982 г. у 86 289 женщин, не имеющих сердечно-сосудистую патологию. На протяжении 30 лет наблюдения зарегистрировали 7628 случаев возникновения сердечно-сосудистых заболеваний и 21 084 смертельных исхода. После корректировки данных на характер потребляемой пищи, образ жизни, использование лекарств и другие факторы у пациенток с частотой стула реже 1 раза в день выявлена достоверная связь с повышенным риском сердечно-сосудистых заболеваний (отношение рисков [HR]: 1,13; 95% доверительный интервал [CI]: 1,05–1,21), общей смертностью (HR: 1,17; 95% ДИ: 1,12–1,22) и сердечно-сосудистой смертностью (HR: 1,17; 95% ДИ: 1,07–1,28). При дальнейшей корректировке индекса массы тела и наличия СД связь с общей смертностью оставалась значительной (HR: 1,10; 95% ДИ: 1,06–1,15), тогда как ассоциации с сердечно-сосудистыми заболеваниями и сердечно-сосудистой смертностью снизилась.
Обсуждаются такие факторы повышения риска сердечно-сосудистого риска у лиц с ХЗ, как повышение артериального давления и урежение сердечного ритма в момент натуживания [84].
ХЗ у лиц с нетрадиционной сексуальной ориентацией
Проблема ХЗ у лиц с нетрадиционной сексуальной ориентацией практически не изучена. Имеются единичные исследования, посвященные нарушениям процесса дефекации у этих лиц. Отмечено, что в большей степени имеет место недержание каловых масс вне зависимости от консистенции каловых масс как у женщин, так и у мужчин с нетрадиционной сексуальной ориентацией [72]. Техника полового анального акта предусматривает резкое повышение давления в прямой кишке, растягивающее и повреждающее воздействие на все анальные сфинктеры. Кроме того, отмечаются повреждение и снижение чувствительности нервных окончаний анального сплетения, что и способствует формированию нарушений позывов на дефекацию, нарушению моторной деятельности прямой кишки и скоординированной работы наружного и внутреннего анальных сфинктеров.
Подготовка пациента к колоноскопическому исследованию [76]
Колоноилеоскопия в настоящее время является стандартным и ведущим методом исследования толстой кишки и терминального отдела подвздошной кишки. Сам результат исследования, его диагностическая точность и терапевтическая безопасность во многом зависят от качества подготовки толстой кишки к колоноскопии. Требования же к степени чистоты толстой кишки возрастают десятикратно, когда основной задачей колоноскопии становится выявление самых ранних, мелких и прогностически опасных неполиповидных новообразований либо небольших ангиэктазий, являющихся источником кишечного кровотечения [76].
Схемы подготовки толстой кишки, как правило, включают диетические ограничения и пероральные слабительные препараты.
Накануне колоноскопии рекомендуется прием прозрачных жидкостей и отнесенных к ним продуктов, а именно прозрачного мясного бульона, кофе без сливок, чая, фруктовых соков без мякоти, желе, негазированных минеральных напитков, фруктового льда, обычной питьевой воды. Прием жидкости при этом не ограничивается. Разрешен их прием и в день проведения колоноскопии, но не позже чем за 2 ч до начала исследования.
Время и режим приема слабительных средств являются одним из важнейших факторов, влияющих на качество очищения кишки.
Пероральный лаваж кишечника – метод общего промывания ЖКТ, при котором используется большой объем водно-электролитных растворов различного состава. В настоящее время лаваж осмотически сбалансированными растворами считается оптимальным и физиологичным, а также гарантирует высокое качество и относительную быстроту подготовки. ПЭГ представляет собой изоосмотический раствор макрогола с электролитами, который после приема внутрь увеличивает объем жидкости в кишечнике. Раствор проходит через кишечник, не всасываясь и не метаболизируясь, в результате чего удается избежать нарушения водно-электролитного баланса и обеспечить эффективный кишечный лаваж.
Традиционно считается, что для достижения очищающего эффекта необходимы достаточно большие объемы (4 л) препарата. Первый жидкий стул обычно появляется после употребления первого литра ПЭГ-ЭЛР, т.е. через 1–2 ч от начала приема препарата; слабительный эффект сохраняется, а опорожнение кишечника завершается в течение 2–3 ч после окончания его приема.
Доказано, что на качество подготовки кишечника влияет схема и время назначения ПЭГ. Проводимые исследования демонстрируют превосходство режимов раздельных доз над режимами с однократным приемом препарата [77].
Прием части (обычно половины) дозы очищающего кишку препарата накануне исследования, а оставшейся части (половины) в день проведения колоноскопии (что называется раздельным, split-режимом подготовки) обеспечивает более высокое качество подготовки толстой кишки по сравнению с приемом полной дозы препарата в день или вечер накануне колоноскопии [78]. Обычно стандартная схема раздельного режима подготовки заключается в разделении дозы препарата на две равные части и приеме одной половины вечером накануне исследования, а второй – утром в день исследования. Время начала приема второй (утренней) дозы препарата должно быть рассчитано таким образом, чтобы пациенту хватило времени на завершение приема препарата, очищения кишечника в комфортных условиях и дорогу до кабинета колоноскопии. Рекомендуемое время между окончанием приема второй дозы препарата и началом процедуры составляет 3–6 ч (одновременно необходим контроль характера стула), но не более 8 ч [79].
Данные проведенного метаанализа представили многочисленные доказательства максимальной эффективности и наилучшей подготовки толстой кишки путем приема 4 л ПЭГ в раздельном режиме (2 л + 2 л), и именно этот подход на сегодняшний день считается критерием стандартной подготовки к колоноскопии [80]. Противопоказаниями для применения ПЭГ-ЭЛР являются повышенная чувствительность к действующим веществам или любому другому компоненту препарата; тяжелое общее состояние пациента, например дегидратация или тяжелая сердечная недостаточность; язва желудка; распространенная злокачественная опухоль или другое заболевание толстой кишки, сопровождающееся обширным поражением слизистой оболочки кишечника; желудочно-кишечная непроходимость; обструкция ЖКТ; перфорация или риск перфорации ЖКТ; нарушения опорожнения желудка (в том числе гастропарез); токсический колит или токсический мегаколон, детский возраст до 18 лет (эффективность и безопасность не установлена у данной популяции; для препарата Фортранс® согласно инструкции по медицинскому применения).
При нарушении функции почек, сердечной недостаточности у пациентов с сопутствующей мочегонной терапией, больных, склонных к развитию водно-электролитного дисбаланса, включая гипонатриемию и гипокалиемию, пациентов с неврологическими нарушениями, у лежачих пациентов и/или у больных с нарушением двигательных функций, лиц со склонностью к аспирации и/или находящихся в полубессознательном состоянии ПЭГ-ЭЛР может применяться с осторожностью (для препарата Фортранс® согласно инструкции по медицинскому применения; информация не эквивалентна для всех препаратов на основе макрогола).
Согласно клиническим рекомендациям Российского эндоскопического общества (2017) [76] ПЭГ-ЭЛР, являясь стандартом подготовки к колоноскопии, позволяет быстро и эффективно подготовить кишку к исследованию, а раздельный режим приема лучше переносится пациентами (класс IA). Клизмы, бисакодил и метоклопрамид в качестве средств, дополняющих полнообъемные режимы ПЭГ-ЭЛР, не приводят к повышению эффективности очищения толстой кишки или переносимости подготовки пациентами; следовательно, их применение в дополнение к 4 л ПЭГ-ЭЛР нецелесообразно (класс IIB).
Препараты на основе ПЭГ обладают более высоким профилем безопасности чем осмотические слабительные на основе фосфата натрия у пациентов с нарушениями водно-электролитного баланса, в частности у пациентов с почечной, печеночной или застойной сердечной недостаточностью, следовательно, его использование предпочтительно у этих групп пациентов (класс IA) (81).
Осмотически сбалансированный электролитный раствор для лаважа на основе полиэтиленгликоля (ПЭГ-ЭЛР)
МНН: макрогол 4000
Препараты:
- Фортранс® (РУ П No 014306/01) – порошок для приготовления раствора. Один пакетик весом 73,69 г содержит макрогол 4000 – 64 г, калия хлорид – 0,75 г, натрия гидрокарбонат – 1,68 г, натрия сульфат безводный – 5,7 г, натрия хлорид – 1,46 мг; натрия сахаринат – 0,1 г.
- Лавакол (РУ ЛС-000443) – порошок для приготовления раствора. Один пакетик весом 14 г содержит макрогол 4000 – 12 г, калия хлорид – 0,2 г, натрия гидрокарбонат – 0,6 г, натрия сульфат – 1 г, натрия хлорид – 0,2 г.
Малообъемный осмотически сбалансированный электролитный раствор для лаважа на основе полиэтиленгликоля и аскорбиновой кислоты
МНН: макрогол 3350
Препарат Мовипреп® (РУ ЛП-002630) – порошок для приготовления раствора. Один пакетик (саше А) содержит макрогол 3350 – 100 г, натрия сульфат – 7,5 г, натрия хлорид – 2,691 г, калия хлорид – 1,015 г; вспомогательные вещества аспартам (E951) – 0,233 г, ацесульфам калия – 0,117 г, ароматизатор лимонный (V3938-1 N1) – 0, 34 г. Второй пакетик (саше Б) содержит аскорбиновую кислоту — 4,7 г, натрия аскорбат XV.
Солевые слабительные
Препарат Эзиклен® (РУ: ЛП-004957) – малообъемный препарат для очищения толстой кишки у взрослых при подготовке к эндоскопическому и радиологическому исследованию толстой кишки или к хирургическим вмешательствам, требующим отсутствия содержимого в толстой кишке. Является осмотическим слабительным средством. Состав концентрата для приготовления раствора для приема внутрь Эзиклен® (г/один флакон): действующие вещества: натрия сульфат безводный – 17,510; магния сульфата гептагидрат – 3,276; калия сульфат – 3,130.
Механизм действия препарата Эзиклен® (трисульфат) обусловлен ограниченным по насыщаемости процессом активного транспорта сульфатов: при достижении порога насыщения всасывания сульфаты остаются в просвете кишечника и обеспечивают осмотический эффект (прием внутрь значительного объема воды вызывает задержку воды в кишечнике, что обеспечивает слабительное действие, вызывая обильную водянистую диарею, и приводит к очищению кишечника). Основной путь выведения сульфатов – кишечником (около 70% от принятого количества); абсорбированные сульфаты выводятся преимущественно почками.
Противопоказания: гиперчувствительность к действующим веществам или к любому из компонентов препарата; желудочно-кишечная обструкция или подозрение на таковую; перфорация кишечника; нарушение опорожнения желудка (в том числе гастропарез); кишечная непроходимость; токсический колит или токсический мегаколон; профузная рвота; дегидратация тяжелой степени; застойная сердечная недостаточность; асцит; тяжелая почечная недостаточность (скорость клубочковой фильтрации <30 мл/ мин/1,73м2); активная фаза воспалительных заболеваний кишечника (таких как болезнь Крона, язвенный колит); беременность и период грудного вскармливания.
Применение трисульфата возможно в разведенном виде с приемом дополнительного объема воды в режиме дробного или единовременного применения.
Трисульфат показал сопоставимую эффективность с полнообъемным и малообъемным растворами ПЭГ и превосходит по эффективности раствор пикосульфата натрия. Он обладает благоприятным профилем безопасности и хорошей переносимостью. Рекомендован для подготовки кишечника к колоноскопии Руководством Европейского общества желудочно-кишечной эндоскопии (ESGE) – 2019 [81–83].
Доказательная база по дифференцированному применению слабительных препаратов различных фармгрупп в лечении вторичного хронического запора при различных заболеваниях
Болезнь Паркинсона
Данные систематического анализа Pedrosa Carrasco A.J. et al. (2018) показали, что наибольший эффект по применению слабительных препаратов у пациентов с болезнью Паркинсона продемонстрировали макрогол и псиллиум (увеличение частоты стула до 2,9 и 2,2 раза в неделю соответственно). Минимально эффективная длительность приема макрогола в среднем составляла от 4 до 8 нед, кратность приема – 1–2 раза/сут. Максимальная длительность приема составила 21 нед. Побочные эффекты носили единичный характер (тошнота, непереносимость вкуса препарата).
Псиллиум назначался в дозе 5 г 2 раза/сут в течение 8 нед. Было отмечено не только увеличение частоты стула, но и объема каловых масс [85, 87].
Способ применения и дозы макрогола 4000: внутрь по 1–2 пакетика (предпочтительно в виде однократного приема по утрам) или по 1 пакету утром и вечером в случае приема 2 пакетов в день.
Ежедневная доза должна корректироваться в соответствии с клиническим эффектом и может варьировать от 1 пакета каждый день до 2 пакетов в день.
Содержимое каждого пакета следует растворить в стакане с водой непосредственно перед приемом.
Эффект от приема препарата выражен в течение 24–48 ч после приема.
Рекомендуемый курс лечения ‒ 3 месц.
Сердечно-сосудистые заболевания
Одной из особенностей лечения вторичного хронического запора у пациентов с сердечно-сосудистой патологией является ограничение приема магнийсодержащих слабительных препаратов [84], что связано с потенциальной возможностью развития гипермагнеземии у пациентов и формированием аритмического синдрома.
Не рекомендовано использование препаратов ревеня в связи с возможностью развития нефротоксичности [86]. Особое внимание следует уделять длительности акта дефекации, его комфорности и отсутствию натуживания при акте дефекации [84].
Пациенты с избыточной массой тела, сахарным диабетом и дислипидемией [85, 87]
Слепое рандомизированное плацебо-контролируемое исследование по эффективности псиллиума в дозе 10 г в течение 12 нед у пациентов с ХЗ, избыточной массой тела и СД 2 типа продемонстрировало не только достоверное учащение стула, но и положительное влияние терапии на массу тела, уровень гликированного гемоглобина и общего холестерина. Статистически значимый послабляющий эффект был отмечен к 8-й неделе приема псиллиума. На момент окончания приема препарата (12 нед) масса тела статистически значимо снизилась в среднем на 2 кг, уровень гликированного гемоглобина – на 0,8% (p=0,002). Кроме этого, улучшилось соотношение содержания общего холестерина к показателям холестерина липопротеинов низкой плотности (p=0,05).
Для лечения ХЗ и состояний, при которых необходима мягкая консистенция стула (анальные трещины, геморрой), 5 г псиллиума размешивают в 150 мл воды, фруктового сока. Полученную суспензию принимают, запивая дополнительным количеством жидкости (не менее 1 стакана). Прием препарата осуществляется 2–3 раза/сут. При приеме препарата следует выпивать не менее 1,5 литров жидкости в сутки.
Приложение 3. Информация для пациента
Диетическая коррекция рациона питания часто оказывается самым эффективным средством лечения и профилактики запоров.
В качестве примера представлена диета № 3.
Показания к диете № 3 – хронические заболевания кишечника, сопровождающиеся гипомоторной дискинезией (упорным запором).
Целевое назначение диеты № 3 – восстановление нарушенных функций кишечника, стимулирование процессов регенерации слизистой оболочки, восстановление нарушенного обмена веществ. Диета направлена на усиление перистальтики, имеет целью опорожнение кишечника с включением в рацион механических, физических и температурных раздражителей. Эта диета применяется при запорах, причиной которых служит неправильное питание без резко выраженных признаков раздражения кишечника.
Общая характеристика диеты № 3: физиологически полноценная диета с нормальным содержанием белков, углеводов и жира, 30% которого составляет растительное масло. Содержание витаминов и минеральных веществ соответствует потребности в них здорового человека.
Химический состав и энергоценность диеты № 3: белки – 100 г; жиры – 90–100 г; углеводы – 400 г; поваренная соль – 6–8 г; калорийность – 2500–2900 ккал; ретинол – 2 мг; тиамин – 4 мг; рибофлавин – 4 мг; никотиновая кислота – 30 мг; аскорбиновая кислота – 100 мг; кальций – 0,8 г; фосфор – 1,2 г; магний – 0;5 г; железо – 0,015 г.
Температура пищи обычная. Пища солится нормально. Жидкость рекомендуется употреблять в количестве 1,2–1,5 л.
Рекомендуется принимать пищу не реже 4–5 раз/сут, обязательно в одни и те же часы. Недопустимы большие перерывы во времени между отдельными приемами пищи.
Когда пищевые продукты попадают в верхние отделы ЖКТ, это рефлекторно вызывает усиление сокращений нижерасположенных отделов кишечника, что способствует ускорению его опорожнения.
Характер кулинарной обработки пищевых продуктов также имеет определенное лечебное значение. В частности, при приготовлении салатов и гарниров не следует очень измельчать морковь, редьку и другие овощи, с этой целью рекомендуется использовать более крупную терку.
В диету включают блюда, богатые растительной клетчаткой, но не раздражающие слизистую оболочку ЖКТ. Рекомендуется включать в рацион салаты из свежих овощей, зелени по 100–150 г 2–3 раза/сут, печеные яблоки, овощи в тушеном виде, разбавленные овощные и фруктовые соки с мякотью. Пища приготовляется в любом виде (преимущественно в неизмельченном виде, на пару или отваривают в воде).
При отсутствии противопоказаний предпочтителен прием овощей и фруктов в сыром виде. Особенно рекомендуются свекла, морковь, помидоры, лиственный салат, кабачки, тыква, цветная капуста, яблоки. Сухофрукты (чернослив, курага, инжир) дают в размоченном виде и в блюдах. Капуста белокочанная, зеленый горошек, молодая стручковая фасоль разрешаются при хорошей переносимости. Зелень петрушки, укропа, сельдерея можно добавить к различным блюдам и салатам.
При запорах у лиц с воспалительными заболеваниями кишечника составляют рацион питания, руководствуясь теми же принципами, но с целью соблюдения принципа щажения слизистой оболочки от возможных неблагоприятных воздействий пищи, овощи применяют в вареном виде.
Рекомендуемые продукты и блюда для диеты № 3:
- продукты, богатые клетчаткой: овощи и фрукты, зелень, черный хлеб, квашеная капуста, а также газированные напитки, яйца, сваренные вкрутую;
- хлебные изделия – пшеничный хлеб из муки грубого помола, хрустящие хлебцы (размоченные), ржаной хлеб, сеяный и из муки обойного помола, отрубный, зерновой, докторский, вчерашней выпечки;
- печенье и другие изделия из теста;
- закуски – салаты из свежих овощей, винегреты с растительным маслом, сельдь, красная икра. Салаты, винегреты с майонезом, заливная рыба, творожная паста;
- супы на некрепком обезжиренном мясном, рыбном бульоне, овощном отваре, с перловой крупой, холодные супы, фруктовые и овощные супы (свекольный суп, ботвинья, окрошка, щавелевый суп и др.). Борщи, свекольники, щи из свежей капусты;
- мясо, птица (изделия из говядины, телятины, птицы, баранины и свинины), рыба нежирных сортов, отварные, запеченные преимущественно куском;
- блюда и гарниры из муки, крупы, бобовых и макаронных изделий – рассыпчатые и полувязкие каши, пудинги, запеканки из круп, макаронных изделий, отварные и в виде запеканок, особенно рекомендуются блюда из гречневой крупы. Из бобовых: зеленый горошек, соевый творог;
- жиры – масло сливочное, масло оливковое, рафинированное, подсолнечное, кукурузное;
- яйца и блюда из них – не более одного яйца в день (в необходимых случаях по кулинарным показаниям добавляются только в блюда);
- блюда и гарниры из овощей и грибов – различные виды овощей и зелень, некислая квашеная капуста. Особенно рекомендуется свекла;
- овощи – свекла, морковь, томаты, салат, огурцы, кабачки, тыква, сырые, вареные на гарнир и в виде запеканок;
- овощи и фрукты разрешаются как в сыром, так и вареном и запеченном виде. Рекомендуются ягоды, фрукты и овощи, стимулирующие функцию кишечника, но не усиливающие брожения и не раздражающие слизистую оболочку кишечника. Особенно рекомендуются дыни, слива, инжир, абрикосы, чернослив, сахар, варенье, особенно рябиновое, муссы, фруктовые конфеты. Сушеные фрукты в размоченном виде (курага, чернослив);
- молоко, молочные продукты и блюда из них – молоко (при переносимости сладкое), сметана, творог, простокваша, одно- и двухдневный кефир, ацидофильное молоко, сыры;
- соусы и пряности молочные, сметанные, на овощном отваре, фруктово-ягодные подливки. Соусы на некрепком мясном, рыбном бульоне;
- напитки – чай некрепкий, чай с молоком, кофе некрепкий натуральный с молоком, фруктово-ягодные соки, сладкие. Соки рекомендуются в холодном виде;
- витамины в виде отвара плодов шиповника, различных сладких ягодных и фруктовых соков, овощных сырых ягод и фруктов, помидоров, пюре из сырой моркови.
Исключаемые продукты и блюда для диеты № 3:
- ограничиваются горячие блюда, кисели и протертые каши;
- для уменьшения негативного влияния на другие органы пищеварительного тракта, что особенно актуально при сочетанной патологии, стараются избегать овощей, богатых эфирными маслами и клетчаткой (лук, редис, репа, шпинат, перец), грибов;
- исключают продукты, богатые холестерином, а также продукты расщепления жира, образующиеся при жарении;
- хлеб из муки высших сортов, сдобные булочные изделия;
- жирные сорта мяса, рыбы, птицы, копчености, мясные и рыбные консервы;
- острые и жирные соусы, хрен, горчица, перец, какао, крепкий чай, животные и кулинарные жиры;
- исключаются хрен, перец, горчица, пряности;
- нежелательны рис, манная крупа, вермишель;
- бобовые, редька, редис, чеснок, лук, грибы;
- кисель, черника, айва;
- шоколад, изделия из крема, какао;
- запрещается употребление алкогольных напитков.
Примерное меню диеты № 3
Вариант № 1:
- первый завтрак: масло, творог со сметаной, гречневая каша с маслом, стакан чая с молоком;
- второй завтрак: тертая морковь со сметаной, стакан отвара шиповника;
- обед: борщ вегетарианский со сметаной, жареное мясо с отварным картофелем и свеклой, квашеная капуста, компот из свежих фруктов (ревеня);
- полдник: стакан слабого чая с хрустящим хлебцем и с медом;
- ужин: голубцы с морковью (вегетарианские), пирог с сухими фруктами (чернослив), стакан слабого чая;
- на ночь – фруктово-ягодный компот;
- на весь день: хлеб грубого помола – 200 г, хлеб ржаной – 200 г, сахар – 50 г.
Вариант № 2:
- утром натощак: стакан холодной воды с сахаром, солью, вареньем или настой чернослива, чернослив, холодный лимонад;
- первый завтрак: стакан некрепкого чая или кофе с молоком, салат, винегрет или тертые редька с морковью и сметаной или постным маслом, 100 г творога или сырок, каша из овсяной крупы или хлопьев «Геркулес», 100 г ржаного хлеба или бородинского («Здоровье»), 20 г масла;
- второй завтрак: сырое яблоко, морковь, стакан отвара шиповника, 1 стакан кефира (простокваши), 100 г черного хлеба, 10 г масла;
- обед: щи из квашеной капусты, фруктовый или овощной суп, окрошка, мясо (жареное или тушеное), рыба, кура, гарниры из свеклы, капусты, картофеля, кабачков, салат, компот из свежих фруктов, сливы, изюм, свежие фрукты;
- ужин: жареная рыба с картофелем, капустой, огурцом, гречневая или ячневая каша с маслом, овощная запеканка, творожники, тушеная капуста, винегрет, фрукты, черный хлеб с маслом салат, тертая редька с морковью и сметаной или кефиром, некрепкий чай с сахаром, варенье.
- на ночь: кефир (1 стакан), размоченный чернослив или пюре из вареной свеклы, фрукты в зависимости от сезона.