Диагностика
1.
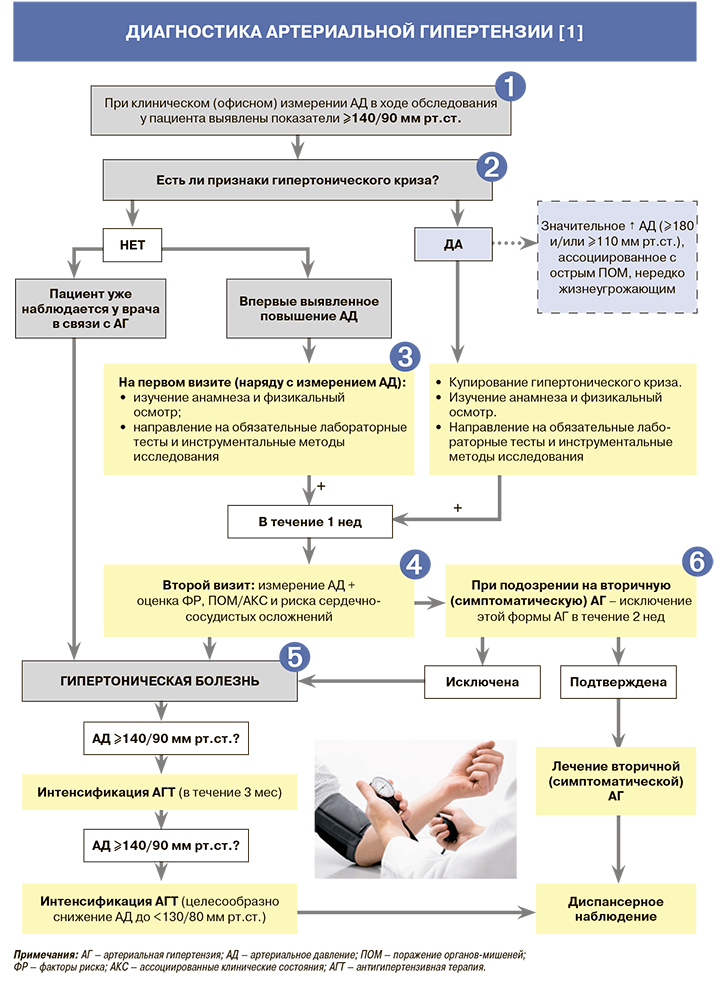
• В большинстве случаев артериальное давление (АД) повышается бессимптомно, и артериальную гипертензию (АГ) обнаруживают лишь в ходе объективного исследования пациента. В тех случаях, когда жалобы есть, они неспецифичны (головная боль, головокружение, сердцебиение и т.д.). При наличии перечисленных симптомов у любого пациента необходимо в процессе его обследования учитывать возможность уже диагностированной АГ [1].
• Диагноз АГ рекомендуется устанавливать при повышении АД выше 140 и/или 90 мм рт.ст. по результатам его клинического (офисного) измерения на двух разных визитах [2, 3]. При этом на каждом визите должно быть выполнено ≥2 измерений АД с интервалом в 1–2 мин и еще одно дополнительное измерение при разнице между первыми двумя результатами >10 мм рт.ст. Уровень АД – среднее из последних двух измерений [1].
• Именно клиническое измерение АД имеет наибольшую доказательную базу для диагностики АГ и оценки эффективности антигипертензивной терапии (АГТ) [1].
• АГ устанавливается сразу, если:
– показатели АД соответствуют АГ 3-й степени (≥180 и/или ≥110 мм рт.ст.), особенно у пациентов с высоким сердечно-сосудистым риском;
– повышенное АД выявлено по данным суточного мониторирования АД (средние показатели ≥130 и/или ≥80 мм рт.ст.) и/или мониторирования АД в домашних условиях (средние показатели ≥135 и/или ≥85 мм рт.ст.) при наличии показаний к их проведению [1].
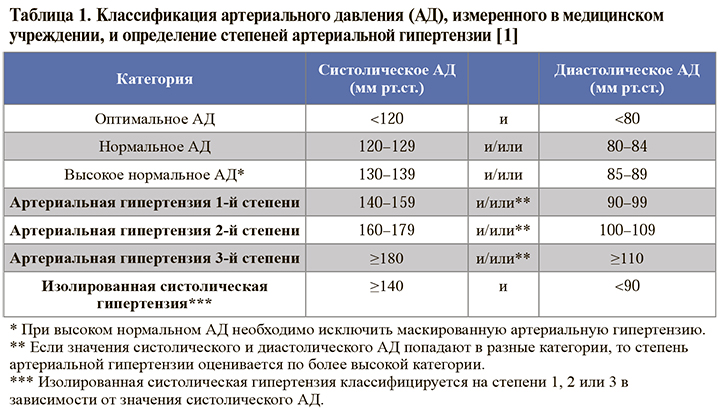
• Градация результатов клинического (офисного) измерения АД приведена в таблице 1.
2.
• При гипертоническом кризе значительное повышение АД (до 3-й степени) сопровождается острым поражением органов-мишеней (ПОМ). Типичные случаи:
– тяжелая злокачественная АГ, ассоциированная с изменениями на глазном дне (кровоизлияния и/или отек соска зрительного нерва), микроангиопатией и диссеминированным внутрисусосудистым свертыванием. Может приводить к энцефалопатии (≈15% случаев) [4], острой сердечной недостаточности, острому ухудшению функции почек [5];
– тяжелая АГ, ассоциированная с другими клиническими состояниями, требующими неотложного снижения АД – расслоением аорты, острой ишемией миокарда, острой сердечной недостаточности;
– внезапное повышение АД на фоне феохромоцитомы, ассоциированное с ПОМ;
– тяжелая АГ у беременных или преэклампсия [1].
• У всех пациентов с впервые диагностированным гипертоническим кризом, необходимо выявить причину повышения АД, в том числе вторичную симптоматическую АГ [1].
• Гипертонический криз требует немедленных квалифицированных действий, направленных на снижение АД, обычно с помощью внутривенной терапии. Лечение рекомендуется проводить в отделении неотложной кардиологии или палате интенсивной терапии [1].
• Термин «неосложненный гипертонический криз», ранее применявший по отношению к пациентам со значительным повышением АД, но без признаков острых изменений в органах-мишенях [6], в настоящее время не рекомендован к использованию. В этой группе больных снижение АД обычно может проводиться амбулаторно, чаще всего путем назначения пероральной терапии в соответствии со стандартным алгоритмом [1].
3.
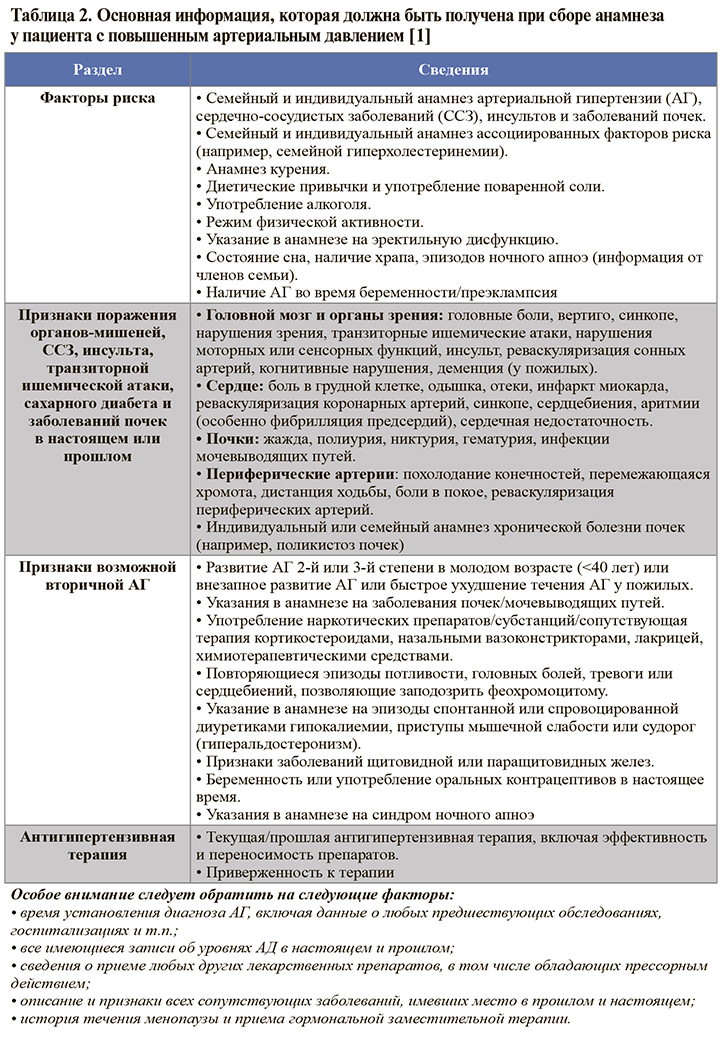
• Основная информация, которая должна быть получена при сборе анамнеза пациента с повышенным АД представлена в таблице 2.
• Физикальное обследование пациента с повышенным АД нацелено на выявление факторов риска (ФР), признаков вторичных форм АГ и ПОМ. Всем пациентам рекомендуется определение антропометрических данных для выявления избыточной массы тела/ожирения, оценка неврологического статуса и когнитивной функции, исследование глазного дна для выявления гипертонической ретинопатии, пальпация и аускультация сердца и сонных артерий, пальпация и аускультация периферических артерий для выявления патологических шумов, хотя бы однократное сравнение АД между руками, пальпация пульса в покое для измерения его частоты и ритмичности с целью выявления аритмий [1].
• Лабораторная диагностика непосредственно для установления диагноза АГ не требуется, но в то же время необходима для исключения вторичных форм заболевания, выявления ПОМ, оценки сердечно-сосудистого риска и сопутствующей патологии, способной негативно влиять на эффективность лечения и качество жизни пациента [1].
• Для исключения вторичной гипертензии всем пациентам с АГ рекомендуется проведение общего (клинического) анализа крови (гемоглобин/гематокрит, лейкоциты, тромбоциты) [1].
• Для выявления предиабета, сахарного диабета (СД) и оценки сердечно-сосудистого риска всем пациентам с АГ рекомендуется исследование уровня глюкозы в венозной крови [1].
• Для выявления нарушения функции почек и оценки сердечно-сосудистого риска всем пациентам с АГ рекомендуются исследование уровня креатинина в сыворотке крови и расчет скорости клубочковой фильтрации (СКФ) в мл/мин/1,73 м2 . С той же целью рекомендуется проводить общий (клинический) анализ мочи с микроскопическим исследованием осадка мочи, количественной оценкой альбуминурии или отношения альбумин/креатинин (оптимально) [1].
• Для стратификации сердечно-сосудистого риска и выявления нарушений липидного обмена всем пациентам рекомендуется исследование уровня общего холестерина (ОХС), холестерина липопротеинов высокой плотности (ХС ЛВП), холестерина липопротеинов низкой плотности (ХС ЛНП) и триглицеридов (ТГ) в крови [1].
• Для выявления электролитных нарушений и дифференциального диагноза с вторичной АГ всем пациентам с АГ рекомендуется исследование уровня калия и натрия в крови [1].
• Для выявления гиперурикемии всем пациентам с АГ рекомендуется исследование уровня мочевой кислоты в крови [1].
• Проведение инструментальных методов диагностики необходимо для исключения вторичных форм АГ, выявления поражения органов-мишеней, оценки сердечнососудистого риска и сопутствующей патологии, влияющей на эффективность лечения и качество жизни пациента [1].
• Для выявления гипертрофии левого желудочка (ГЛЖ) и определения сердечнососудистого риска всем пациентам с АГ рекомендуется проведение 12-канальной электрокардиографии (ЭКГ) [1].
• При наличии изменений на ЭКГ или симптомов/признаков дисфункции левого желудочка рекомендуется проведение эхокардиографии (ЭхоКГ) для выявления степени ГЛЖ [1].
• Пациентам с цереброваскулярной болезнью или признаками атеросклеротического поражения сосудов других локализаций при указании в анамнезе на преходящую слабость в конечностях с одной стороны или онемение половины тела, а также мужчинам старше 40 лет, женщинам старше 50 лет и больным с высоким общим сердечно-сосудистым риском рекомендуется дуплексное сканирование брахиоцефальных артерий для выявления атеросклеротических бляшек/ стенозов внутренних сонных артерий [1].
• Рекомендуется определение лодыжечно-плечевого индекса (ЛПИ) для уточнения категории риска пациентам с симптомами значимого атеросклероза артерий нижних конечностей или пациентам умеренного риска, у которых положительные результаты данного исследования приведут к изменению категории риска [1].
• Всем пациентам с нарушением функции почек, альбуминурией и при подозрении на вторичную АГ рекомендуется проведение ультразвукового исследования (УЗИ) почек и дуплексного сканирования артерий почек для оценки размеров, структуры, а также наличия врожденных аномалий почек или стеноза почечных артерий [1].
• Пациентам с АГ 2–3-й степеней, всем пациентам с СД и АГ рекомендуется исследование глазного дна врачом-офтальмологом (геморрагии, экссудаты, отек соска зрительного нерва) для выявления гипертонической ретинопатии [1].
• Пациентам с АГ при наличии неврологических симптомов и/или когнитивных нарушений рекомендуется компьютерная томография (КТ) или магнитно-резонансная томография (МРТ) головного мозга для исключения инфарктов мозга, микрокровоизлияний и повреждений белого вещества и других патологических образований [1].
• Иные диагностические исследования в рамках диагностики АГ не предусмотрены. Расширение диагностических исследований возможно по решению врача в зависимости от клинической ситуации и состояния пациента [1].
4.
• К сердечно-сосудистым ФР у пациентов с АГ относятся:
– пол (мужчины >женщины);
– возраст ≥55 лет у мужчин, ≥65 лет у женщин;
– курение в настоящем или прошлом. Курение в прошлом следует рассматривать как ФР при отказе от курения в течение последнего года;
– дислипидемия (ОХС >4,9 ммоль/л, и/или ХС ЛПНП >3,0 ммоль/л, и/или ХС ЛПВП <1,0 ммоль/л (40 мг/дл) у мужчин и <1,2 ммоль/л (46 мг/дл) у женщин, и/или ТГ >1,7 ммоль/л);
– уровень мочевой кислоты ≥360 мкмоль/л у женщин, ≥420 мкмоль/л у мужчин;
– нарушение гликемии натощак (глюкоза плазмы натощак 5,6–6,9 ммоль/л);
– нарушение толерантности к глюкозе;
– избыточная масса тела (индекс массы тела 25–29,9 кг/м2 ) или ожирение (≥30 кг/м2 );
– семейный анамнез развития ССЗ в молодом возрасте (<55 лет для мужчин и <65 лет для женщин);
– развитие АГ в молодом возрасте у родителей или в семье;
– ранняя менопауза;
– малоподвижный образ жизни;
– психологические и социально-экономические факторы;
– частота сердечных сокращений в покое >80 уд./мин [1].
• К ПОМ у пациентов с АГ относятся:
– артериальная жесткость (пульсовое давление у пожилых пациентов ≥60 мм рт.ст., каротидно-феморальная скорость пульсовой волны >10 м/с;
– ЭКГ-признаки ГЛЖ на (индекс Соколова–Лайона >35 мм, или амплитуда зубца R в отведении aVL ≥11 мм, корнельское произведение >2440 мм × мс, или корнельский вольтажный индекс >28 мм для мужчин и >20 мм для женщин);
– ЭхоКГ-признаки ГЛЖ (индекс массы ЛЖ >50 г/м2 и >47 г/м2 для женщин; для пациентов с нормальной массой тела – индексация на площадь поверхности тела >115 г/м2 у мужчин и >95 г/м2 у женщин);
– альбуминурия 30–300 мг/24 ч или отношение альбумин–креатинин 30–300 мг/г или 3,4–34 мг/ммоль (предпочтительно в утренней порции мочи);
– ХБП С3 стадии с СКФ 30–59 мл/мин/1,73 м2;
– ЛПИ <0,9; – выраженная ретинопатия: наличие кровоизлияний, экссудатов или отека соска зрительного нерва [1].
• Основные ассоциированные клинические состояния (АКС) при АГ:
– ишемический инсульт, геморрагический инсульт, транзиторная ишемическая атака (ТИА);
– ишемическая болезнь сердца (инфаркт миокарда, стенокардия, реваскуляризация миокарда);
– наличие атероматозных бляшек при визуализации (стеноз ≥50%);
– сердечная недостаточность, в том числе с сохраненной фракцией выброса;
– заболевания периферических артерий;
– фибрилляция предсердий;
– тяжелая хроническая болезнь почек (ХБП) С4–С5 с СКФ <30 мл/мин/1,73 м2 [1].
• Дополнительным состоянием, усугубляющим сердечно-сосудистый риск, является СД (глюкоза плазмы натощак ≥7,0 ммоль/л при двух последовательных измерениях и/или HbA1c ≥6,5%, и/ или глюкоза плазмы после нагрузки или при случайном определении ≥11,1 ммоль/л) [1].
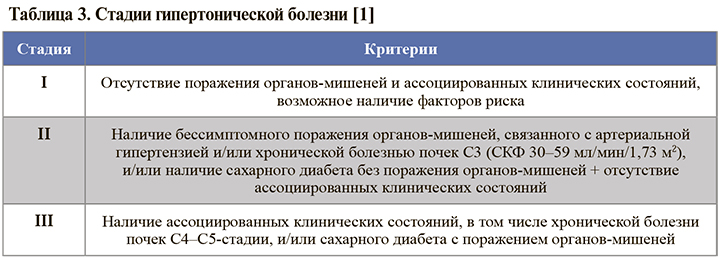
• Стадийная классификация гипертонической болезни, в зависимости от наличия ФР, ПОМ, АКС, ХБП и СД, приведена в таблице 3. Стадия АГ не зависит от уровня АД [1].
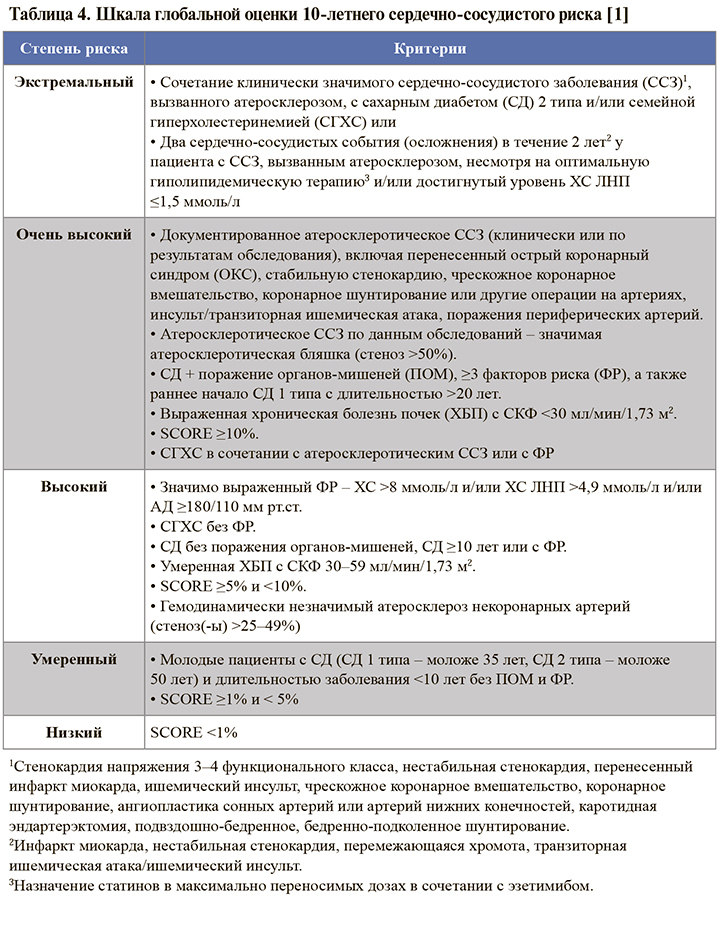
• На основании уровня АД, наличия ФР, ПОМ, АКС, СД выделяют 5 категорий риска сердечно-сосудистых осложнений (табл. 4). Наиболее значимым является определение категории риска у пациентов с гипертонической болезнью I и II стадий [1].
5.
• Гипертоническая болезнь – хронически протекающее заболевание, основным проявлением которого является повышение АД, не связанное с выявлением явных причин, приводящих к развитию вторичных форм АГ (симптоматические АГ).
• При формулировке диагноза необходимо указать:
– стадию гипертонической болезни;
– у пациентов с впервые диагностированной АГ – степень повышения АД;
– если пациент уже применяет антигипертензивную терапию – наличие контроля АД (контролируемая/неконтролируемая АГ);
– ФР, ПОМ, ССЗ, ХБП и категорию сердечно-сосудистого риска;
– целевой уровень АД для конкретного пациента.
• Пример формулировки диагноза: ГБ II стадии. Неконтролируемая АГ. Нарушенная гликемия натощак. Гиперлипидемия. ГЛЖ. Риск 3 (высокий). Целевое АД <130/<80 мм рт.ст. [1].
• При вторичной (симптоматической) гипертонии жалобы обусловлены основным заболеванием. К таким заболеваниям относятся:
– синдром обструктивного апноэ во сне (признаки – храп, головная боль по утрам, сонливость в дневное время, нарушение памяти, внимания, неполноценный ночной сон);
– первичный гиперальдостеронизм (мышечная слабость, полиурия, полидипсия, запоры);
– феохромоцитома (пароксизмальная АГ, головная боль, профузная потливость, сердцебиение, лабильное повышение АД, ортостатическая гипотония);
– синдром Иценко–Кушинга (лунообразное лицо, плетора, жировой горбик, гирсутизм, центральное ожирение, атрофия кожи, багровые стрии, синяки, нарушения углеводного обмена);
– заболевания щитовидной железы (симптомы тиреотоксикоза или гипотиреоза);
– коарктация аорты (головная боль, холодные конечности, боль в ногах при физических нагрузках, носовые кровотечения) [1].
• Рекомендуется при установлении диагноза учитывать возможность вторичной (симптоматической) формы АГ и проводить диагностические мероприятия, направленные на ее исключение, при наличии следующих признаков:
– АГ 2-й степени у пациентов моложе 40 лет или любое повышение АД у детей;
– внезапное острое развитие АГ у пациентов с ранее документированной стойкой нормотонией;
– резистентная АГ 3-й степени или гипертонический криз;
– признаки значительных изменений в органах-мишенях;
– клинические или лабораторные признаки, позволяющие подозревать эндокринные причины АГ или ХБП;
– клинические симптомы синдрома обструктивного апноэ во сне;
– симптомы, позволяющие заподозрить феохромоцитому, или семейный анамнез данной опухоли.
• Для диагностики вторичных форм АГ важно детальное обследование пациента, начиная с рутинных методов (опроса, осмотра, лабораторной диагностики) до выполнения сложных инструментальных исследований [1].
Лечение
1.
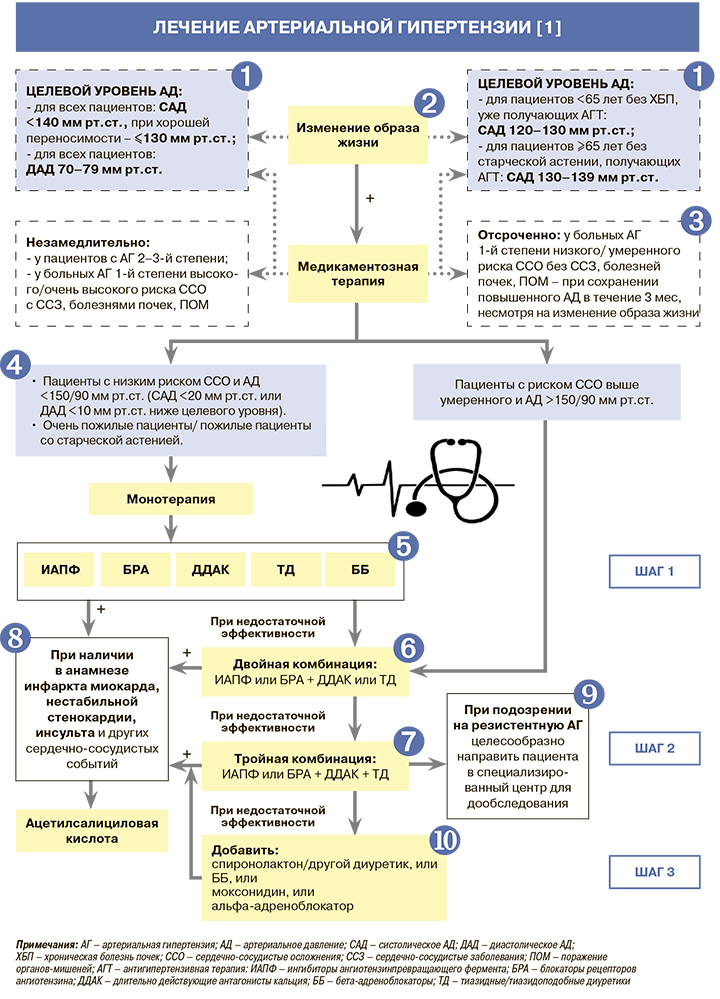
• Нижняя граница безопасности целевых уровней артериального давления (АД) установлена на основании результатов исследований, проведенных преимущественно в группах пациентов высокого и очень высокого риска (пожилые с коморбидностью, установленными сердечно-сосудистыми заболеваниями, в том числе лица с ИБС, заболеванием периферических артерий). Таким образом, в общей популяции пациентов с артериальной гипертензией (АГ), вероятно, нет необходимости в коррекции лечения при уровне систолического АД (САД) <120 мм рт.ст. и диастолического АД (ДАД) <70 мм рт.ст. в случае его хорошей переносимости [1].
• Пациентам ≥65 лет, получающим антигипертензивную терапию (АГТ), при каждом визите к врачу рекомендуется проводить оценку возможных нежелательных явлений [1].
2.
• Немедикаментозные методы лечения АГ способствуют снижению АД, уменьшают потребность в антигипертензивных препаратах и повышают их эффективность, позволяют осуществлять коррекцию факторов риска (ФР) [7, 8].
• Меры по изменению образа жизни рекомендованы не только всем пациентам с АГ, но и людям с высоким нормальным АД (130–139/85–89 мм рт.ст.) и/или ФР для первичной профилактики АГ [1].
• Всем пациентам с АГ для улучшения контроля заболевания рекомендуется ограничение употребления соли до <5 г/сут [1].
• Всем пациентам с АГ для улучшения контроля заболевания рекомендуется ограничить употребления алкоголя (<14 единиц в неделю для мужчин и <8 единиц в неделю для женщин, где 1 единица соответствует 125 мл вина или 250 мл пива) и избегать хронического злоупотребления спиртным [1].
• Всем пациентам с АГ для улучшения метаболических показателей рекомендуется увеличить употребление овощей, свежих фруктов, рыбы, орехов и ненасыщенных жирных кислот (оливковое масло), молочных продуктов низкой жирности, уменьшить употребление мяса [1].
• Всем пациентам с АГ с целью снижения АД и сердечно-сосудистого риска рекомендуется контроль массы тела для предупреждения развития ожирения, достижение/ поддержание индекса массы тела (ИМТ) в пределах 20–25 кг/м2 , окружности талии <94 см у мужчин и <80 см у женщин [1].
• Всем пациентам с АГ в связи с доказанным положительным эффектом на уровень сердечно-сосудистой смертности рекомендуются регулярные аэробные физические упражнения (≥30 мин динамических упражнений умеренной интенсивности 5–7 дней в неделю) [1].
• Всем пациентам с АГ в связи с доказанным негативным эффектом курения на уровень смертности рекомендуются прекращение курения, психологическая поддержка и выполнение программ по отказу от этой вредной привычки [1].
3.
Возможность применения фармакотерапии может быть рассмотрена и при высоком нормальном АД у пациентов высокого риска с сердечно-сосудистыми заболеваниями ССЗ), особенно с ишемической болезнью сердца [1].
4.
• Пожилым пациентам с АГ (даже в возрасте >80 лет), находящимся в удовлетворительном физическом состоянии, рекомендуется изменение образа жизни + АГТ при уровне САД ≥160 мм рт.ст. В случае хорошей переносимости АГТ у этой группы пациентов (отсутствие ортостатической гипотонии, развития/усугубления гериатрических синдромов и снижения функционального статуса) отменять ее не следует в связи с доказанными преимуществами в снижении сердечно-сосудистой смертности [1].
• Пожилым пациентам в возрасте 66–79 лет, находящимся в удовлетворительном физическом состоянии (без синдрома старческой астении), при САД 140–159 мм рт.ст. (АГ 1-й степени), изменение образа жизни в сочетании с АГТ рекомендовано при хорошей переносимости антигипертензивных препаратов [1].
5.
• К ингибиторам АПФ (ИАПФ), зарегистрированным в России, относятся зофеноприл, каптоприл, лизиноприл, периндоприл, рамиприл, спираприл, трандолаприл, фозиноприл, хинаприл, цилазаприл, эналаприл. Блокаторы рецепторов ангиотензина II (БРА, сартаны), представленные в России – азилсартана медоксомил, валсартан, ирбесартан, кандесартан, лозартан, олмесартана медоксомил, телмисартан, эпросартан [9].
• ИАПФ и БРА эффективно предотвращают или приводят к обратному развитию поражения органов-мишеней (гипертрофии левого желудочка, ремоделирования мелких артерий) на фоне соответствующего снижения АД. Обе группы препаратов снижают риск пароксизмов фибрилляции предсердий (ФП), что может быть обусловлено улучшением функции левого желудочка (ЛЖ) и более эффективным регрессом его структурных изменений [10].
• ИАПФ и БРА обладают сходной эффективностью в отношении сердечно-сосудистых осложнений и смертности по сравнению как друг с другом, так и с другими классами антигипертензивных препаратов [1]. БРА по сравнению с другими классами характеризуются более низкой частотой отмены из-за побочных эффектов, сопоставимой с плацебо [11, 12].
• ИАПФ и БРА снижают альбуминурию в большей степени, чем другие антигипертензивные препараты, и эффективно замедляют прогрессирование диабетической и недиабетической ХБП [13]. По данным метаанализов, блокаторы ИАПФ и БРА единственные из всех антигипертензивных препаратов доказанно снижают риск терминальной ХБП.
• Прием ИАПФ ассоциирован с умеренным повышением риска ангионевротического отека, особенно у представителей негроидной расы. У таких пациентов следует отдавать предпочтение БРА [1].
• ИАПФ и БРА абсолютно противопоказаны при высокой гиперкалиемии (≥5,5 ммоль/л), двухстороннем стенозе почечных артерий, стенозе почечной артерии единственной почки, беременным и кормящим женщинам, а также пациентам с ангионевротическим отеком в анамнезе [1].
• Длительно действующие антагонисты кальция (АК), зарегистрированные в России для лечения АГ:
– дигидропиридиновые – амлодипин, лацидипин, левамлодипин, лерканидипин, нитрендипин, нифедипин (пролонгированные формы), фелодипин;
– недигидропиридиновые – прологированные формы верапамила и дилтиазема [9].
• Все АК метаболически нейтральны и не оказывают отрицательного действия на углеводный, липидный и пуриновый обмен. Помимо антигипертензивного, они оказывают антиангинальное и органопротективное действие, тормозят агрегацию тромбоцитов. В целом их влияние на сердечно-сосудистый риск схоже с другими классами антигипертензивных препаратов [10, 14].
• АК обладают большим эффектом в отношении профилактики инсультов, чем этого можно было ожидать только от антигипертензивного эффекта, однако менее эффективны в плане профилактики хронической сердечной недостаточности (ХСН) с низкой фракцией выброса (ФВ) [1].
• Не рекомендуется (абсолютное противопоказание) назначение недигидропиридиновых АК при атриовентрикулярной блокаде 2–3-й степени, ХСН с низкой ФВ ЛЖ. Для дигидропиридиновых АК абсолютных противопоказаний нет.
• К тиазидным/тиазидоподобным диуретикам (ТД), зарегистрированным в России, относятся гидрохлоротиазид, индапамид, хлорталидон [9]. Они обладают выраженным антигипертензивным эффектом и остаются краеугольным камнем антигипертензивной терапии (АГТ). Их эффективность в предотвращении всех вариантов сердечнососудистых осложнений и смертности подтверждена в рандомизированных клинических исследованиях (РКИ) и метаанализах [15].
• Диуретики более эффективно предотвращают сердечную недостаточность, чем другие классы препаратов [10].
• В настоящее время ведутся дискуссии о том, следует ли предпочесть тиазидоподобные диуретики (индапамид, хлорталидон) классическим тиазидным диуретикам (гидрохлоротиазид), хотя их превосходство не было подтверждено в РКИ с прямым сравнением. Недавний метаанализ плацебо-контролируемых РКИ показал сходные эффекты всех терх указанных диуретических лекарственных средств на сердечнососудистые исходы [15]. Таким образом, в отсутствие прямых сравнительных исследований и с учетом того, что гидрохлоротиазид является компонентом многих фиксированных комбинаций, можно рекомендовать равноценное использование тиазидов, хлорталидона и индапамида.
• ТД снижают уровень сывороточного калия и имеют менее благоприятный профиль безопасности, чем ИАПФ и БРА [15, 16]. Они также могут способствовать повышению инсулинорезистентности и риска развития СД. Недавно проведенные исследования показали, что снизить негативное влияние ТД на метаболизм глюкозы можно добавлением калийсберегающего диуретика [17].
• ТД характеризуются снижением антигипертензивной эффективности при СКФ <45 мл/мин/1,73 м2 , а при СКФ <30 мл/мин/1,73 м2 становятся вовсе неэффективными. В этом случае в качестве альтернативы следует использовать петлевые диуретики (торасемид, фуросемид) [1].
• У пациентов, не достигших целевого АД при использовании монотерапии или комбинированной АГТ, не включавшей диуретики, рекомендуется назначение низких доз ТД в составе комбинированной терапии с БРА, ИАПФ и АК для усиления антигипертензивного эффекта и достижения целевого АД [18].
• Абсолютными противопоказаниями для гидрохлортиазида и хлорталидона и относительным для индапамида служат подагра и бессимптомная гиперурикемия [1].
• Для лечения АГ показаны бета-блокаторы (ББ) с вазодилатирующими свойствами (карведилол, небиволол) и высокоселективные β1-блокаторы (бисопролол, метопролол замедленного высвобождения) [1].
• ББ рекомендованы в качестве АГТ в особых клинических ситуациях. Их назначение предпочтительно при симптомной стенокардии напряжения, перенесенном инфаркте миокарда (ИМ), хронической ХСН с низкой ФВ, ФП, аневризме аорты, контроле частоты сердечных сокращений, а также для лечения АГ у женщин детородного возраста, особенно планирующих беременность [1].
• В отдельных исследованиях продемонстрированы неодинаковые эффекты классических и вазодилатирующих ББ в отношении центрального АД, артериальной ригидности, риска развития сахарного диабета (СД), исходов при ХСН. Однако РКИ по сопоставлению эффективности ББ с разными свойствами у пациентов с АГ не проводились. У физически активных пациентов и при наличии метаболического синдрома, нарушенной толерантности к глюкозе (НТГ) рекомендованы ББ с вазодилатирующим эффектом (карведилол, небиволол), не оказывающие отрицательного влияния на инсулинорезистетность [1].
• Абсолютные противопоказания для назначения ББ – синоатриальная, атриовентрикулярная блокада 2–3-й степени, синдром слабости синусового узла и бронхиальная астма [1].
6.
• Многочисленными РКИ показано, что монотерапия эффективно снижает АД лишь у ограниченного числа пациентов с АГ, и большинству больных для удовлетворительного контроля АД требуется комбинация как минимум из двух препаратов. Метаанализ более 40 исследований продемонстрировал, что рациональные комбинация двух препаратов из любых двух классов антигипертензивных средств усиливает степень снижения АД намного сильнее, чем повышение дозы одного препарата. Еще одно преимущество комбинированной терапии – возможность физиологического и фармакологического синергизма между препаратами разных классов, что может не только лежать в основе более выраженного снижения АД и лучшей переносимости. Комбинированная терапия позволяет также подавить контррегуляторные механизмы повышения АД. К рациональным комбинациям антигипертезнивных средств относятся ИАПФ + ТД; БРА + ТД; ИАПФ + АК; БРА + АК; дигидропиридиновый АК + ББ; АК + ТД; ББ + ТД [1].
• На практике могут быть использованы и другие комбинации пяти основных классов антигипертензивных средств при наличии индивидуальных показаний. В случае клинической целесообразности, с учетом особенностей клинического течения заболевания, коморбидной патологии, переносимости лечения и профиля побочных эффектов, а также при наличии предпочтений пациента, связанных с его личным позитивным или негативным опытом и соответственно с учетом ожидаемой приверженности к лечению, врач имеет право назначать любой антигипертензивный препарат, который зарегистрирован для лечения АГ в России как в монотерапии, так и в комбинации. При этом отклонение от стандартных схем терапии требует соответствующего объяснения в истории болезни [1].
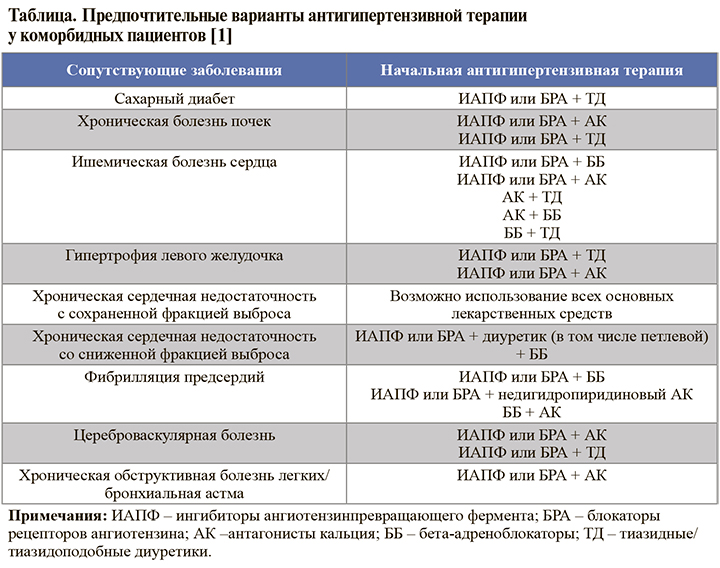
• Предпочтительные варианты начальной АГТ при наличии у пациента с АГ ряда распространенных сопутствующих заболеваний представлена в таблице 1.
• Фиксированные комбинации антигипертензивных средств разных классов повышают приверженность к лечению [1].
• К запрещенным сочетаниям антигипертензивных средств относится комбинация ИАПФ + БРА [1].
7.
• Совершение «шага» в рамках АГТ при недостаточной эффективности используемой комбинации предполагает либо использование более высоких дозировок в комбинации, либо сразу переход на 3-компонентную схему лечения. Оба подхода допустимы на этапе применения двойной комбинации антигипертензивных средств, но при этом они должны обеспечить достижение целевого АД в течение 3 мес с шагом титрации дозы приблизительно 4 нед [1].
• В реальной практике на первом шаге комбинированной АГТ необходимо назначать препараты в оптимальных терапевтических дозах, которые могут обеспечить достижение целевого АД в первые 3 мес. В этом случае при недостижении целевого АД рациональным будет переход на следующий шаг – к тройной терапии [1].
• При оценке необходимости расширения АГТ необходимо помнить, что целевые уровни АД являются рекомендованными для достижения в каждой подгруппе пациентов, но важнейшим принципом их достижения служит соблюдение безопасности и сохранения качества жизни пациента. Поэтому скорость достижения целевых значений и степень снижения АД может быть скорректирована у конкретного пациента в зависимости от конкретной клинической ситуации. При этом плохая переносимость снижения АД может быть основанием для более медленной титрации доз и числа назначаемых препаратов; равно как при хорошей переносимости АГТ, АД может быть снижено до более низких значений, чем рекомендовано в среднем [1].
• Недостижение целевого АД за 3 мес не считается неудачей АГТ, если это продиктовано клинической необходимостью. Если врач считает, что препятствием к достижению целевого АД выступает плохая приверженность пациента, это должно находить отражение в медицинской документации и должны быть предприняты и зафиксированы меры по повышению комплаенса. В этих случаях недостижение целевого уровня не должно считаться дефектом оказания помощи [1].
• К рекомендуемым комбинациям трех антигипертензивных препаратов относятся ИАПФ + АК + диуретик и БРА + АК + диуретик. По показаниям, при наличии особых условий можно использовать и другие комбинации: ИАПФ + дигидропиридиновый АК + ББ; БРА + дигидропиридиновый АК + ББ; ИАПФ + диуретик + ББ; БРА + диуретик + ББ; дигидропиридиновый АК + диуретик + ББ [1].
• В России зарегистрированы две рациональные тройные фиксированные комбинации антигипертензивных средств, рекомендованные при недостаточной эффективности двойной терапии: лизиноприл + индапамид + амлодипин и периндоприл + индапамид + амлодипин [9]. При их недоступности возможно использование двойной фиксированной комбинации + третьего компонента в виде монопрепарата или сочетание трех монопрепаратов.
8.
• Больным АГ с перенесенными сердечно-сосудистыми событиями рекомендуется назначение ацетилсалициловой кислоты в низких дозах (75–150 мг) [19]. Длительный прием ее в рамках вторичной профилактики снижает частоту сердечно-сосудистой смерти на 15%, несмертельных сосудистых событий – на 30% [20]. Применение ацетилсалициловой кислоты в течение 2 лет у пациентов после ИМ ассоциировано с абсолютным снижением риска кардиоваскулярных событий на 33±7%/1000 пролеченных больных и на 39±5%/1000 пролеченных больных в течение 1 мес. После перенесенного инсульта или транзиторной ишемической атаки снижение частоты сердечно-сосудистых событий составляет 27±8% на 1000 больных, пролеченных в течение 34 мес [21]. В исследование у пациентов со стабильной стенокардией прием ацетилсалициловой кислоты (75 мг/сут) в течение 15 мес по сравнению с плацебо суммарно снижал частоту ИМ и внезапной смерти на 34%, а других сосудистых событий и сердечно-сосудистой смертности – на 22–32% [22].
9.
• Резистентная АГ устанавливается на основании следующих критериев:
– соблюдение мероприятий по изменению образа жизни и лечение с использованием оптимальных (или максимальных переносимых) доз трех и более лекарственных препаратов, включая ИАПФ или БРА, АК и диуретик не приводит к снижению САД и ДАД до значений <140 и/или <90 мм рт.ст. соответственно;
– неадекватность контроля АД подтверждена с помощью суточного мониторирования АД (СМАД) и/или мониторирования АД в домашних условиях (ДМАД);
– подтверждена приверженность пациента к лечению;
– исключены причины псевдорезистентности и причины вторичной АГ [1].
• Прежде чем диагностировать резистентную АГ, необходимо исключить причины псевдорезистентности:
– низкая приверженность к назначенной терапии, которая выявляется у ≤50% пациентов и прямо зависит от количества назначенных таблеток [23];
– феномен «белого халата» (при котором АД, измеренное в медицинском учреждении, повышено, но по данным СМАД или ДМАД уровень АД контролируется);
– нарушение правил измерения АД в медицинском учреждении, включая использование манжеты меньшего размера, может привести к ложному выявлению повышенного АД;
– выраженный кальциноз плечевой артерии, особенно у пожилых пациентов;
– клиническая инертность, приводящая к назначению нерациональных комбинаций и неадекватных доз антигипертензивных препаратов [1].
10.
• У 15–20% пациентов контроль АД может быть не достигнут при использовании трех препаратов. В этом случае используется комбинация из ≥4 антигипертензивных препаратов (предпочтительно в двух таблетках). Однако в случаях резистентной АГ при добавлении каждого нового препарата необходимо контролировать их эффективность, и неэффективные антигипертензивные средства следует отменять, а не сохранять в рамках постепенного усиления многокомпонентной АГТ [1].
• Пациентам с АГ, не достигшим целевого АД на фоне тройной комбинированной терапии, рекомендуется добавление спиронолактона, который оказывает положительный эффект при сердечной недостаточности и резистентной АГ [1].
• При непереносимости спиронолактона в качестве 4-го компонента терапии АГ возможно использование других диуретиков (эплеренона, петлевых диуретиков, в том числе в более высоких дозах), ББ, альфа-адреноблокаторов или препаратов центрального действия [24].
• Эплеренон, как и спиронолактон, продемонстрировал положительный эффект при сердечной недостаточности и резистентной АГ. Для лечения АГ спиронолактон и эплеренон используются в низких суточных дозах (25–50 мг). Абсолютным противопоказанием к их использованию является СКФ <30 мл/мин/1,73 м2 из-за повышения риска гиперкалиемии и ухудшения функции почек [1].
• Агонист имидазолиновых рецепторов моксонидин повышает чувствительность тканей к инсулину у пациентов с избыточной массой тела, мягкой АГ и инсулинорезистентностью и нарушением углеводного обмена. Назначение этого препарата возможно при ведении пациентов с АГ, ожирением и инсулинорезистентностью [25]. Его назначение противопоказано при синдроме слабости синусового узла, синоатриальной, атриовентрикулярной блокаде 2–3-й степени, выраженной брадикардии с ЧСС <50 в минуту, ХСН III–IV функционального класса [1].
• Предпочтительным показанием для альфа-адреноблокаторов (доксазозин, празозин) является наличие у пациентов с АГ доброкачественной гиперплазии предстательной железы. Они улучшают углеводный и липидный обмены, повышают чувствительность тканей к инсулину, улучшают почечную гемодинамику. Ввиду того что эти препараты вызывают постуральную гипотензию, их с осторожностью применяют у пациентов с диабетической нейропатией и у пациентов старше 65 лет [1].