Неалкогольная жировая болезнь печени (НАЖБП) – одно из наиболее распространенных хронических заболеваний печени среди взрослых. Патоморфологические особенности позволяют разделить НАЖБП на диффузный стеатоз гепатоцитов (неалкогольная жировая дистрофия печени) и неалкогольный стеатогепатит (НАСГ), включающий воспаление и повреждение клеток печени и в некоторых случаях цирроз печени, который может быть причиной развития гепатоцеллюлярной карциномы (ГЦК).
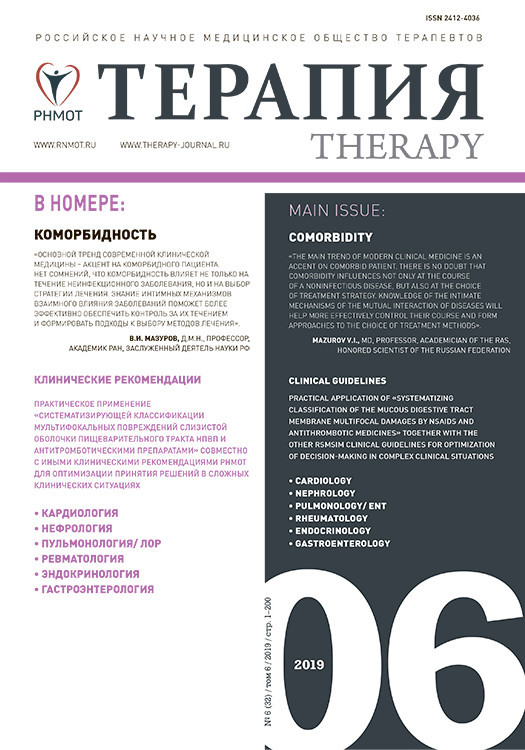
По данным Минздрава России 2018 г. [1], в структуре смертности по основным классам заболеваний болезни органов пищеварения (БОП) занимают 3-е место, уступая лишь болезням системы кровообращения и онкологическим заболеваниям. При этом на долю хронических заболеваний печени приходится около половины летальных исходов, связанных с БОП (рис. 1).
Так, в Санкт-Петербурге среди БОП, являющихся причинами летальных исходов, доля заболеваний печени различной этиологии составляет 47%, причем 11% приходится на алкогольную болезнь печени (АБП), а 89% – на другие гепатологические заболевания, среди которых, по-видимому, может быть и НАЖБП [1].
 Согласно данным исследования C.D. Williams (2011), в котором диагноз устанавливали по данным ультразвукового исследования (УЗИ), распространенность НАЖБП в популяции США составила 46% [2].
Согласно данным исследования C.D. Williams (2011), в котором диагноз устанавливали по данным ультразвукового исследования (УЗИ), распространенность НАЖБП в популяции США составила 46% [2].
В исследовании Dionysos (2004) НАЖБП была выявлена у 94% пациентов с ожирением (ИМТ >30), у 67% пациентов с избыточным весом (ИМТ >25) и у 25% с нормальной массой тела. При этом увеличение распространенности ожирения коррелировало с возрастанием распространенности НАЖБП [3].
R.J. Wong et al. показали, что с 2002 по 2012 г. НАЖБП стала третьей по значимости причиной трансплантации печени в США (рис. 2) [4].
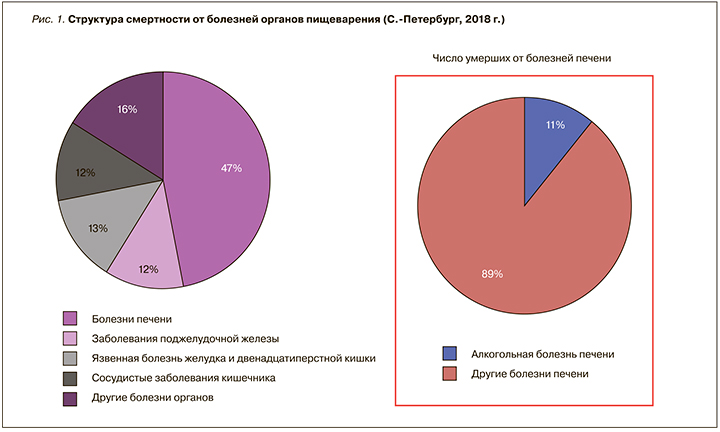
В России встречаемость НАЖБП, по данным российского многоцентрового эпидемиологического исследования, увеличилась с 27 до 37,3%. При этом ее распространенность резко возрастает в возрасте старше 30 лет. Так, наиболее часто НАЖБП выявлялась в следующих возрастных группах: 50–59 лет – 31,1%, 40–49 лет – 23,6%, 60–69 лет – 18,1% (рис. 3) [5].
В настоящее время НАЖБП считается мультифакторным заболеванием, при этом большое внимание уделяется коморбидным состояниям. Например, НАЖБП увеличивает риск развития сахарного диабета 2 типа (СД 2), болезней системы кровообращения и хронической болезни почек (ХБП). Кроме того, появляется все больше данных о том, что НАЖБП связана с другими хроническими заболеваниями, такими как апноэ во сне, колоректальный рак, остеопороз, псориаз, гастроэзофагеальная рефлюксная болезнь (ГЭРБ), различные эндокринопатии (например, синдром поликистозных яичников) и др. [6].
Патофизиологическая связь СД 2, НАЖБП и ГЦК представлена на рисунке 4 [7]. Отметим, что биологические механизмы, лежащие в основе ассоциации между этими заболеваниями, до конца не изучены. СД 2 и НАЖБП тесно связаны с абдоминальным ожирением, инсулинорезистентностью, хроническим воспалением и нарастанием окислительного стресса, что может способствовать развитию и прогрессированию ГЦК, увеличению клеточного роста и пролиферации, ингибированию клеточного апоптоза, увеличению ангиогенеза и повреждению ДНК. Кроме того, увеличение продукции инсулина, фактора роста 1 (IGF-1) дополнительно повышает клеточный рост/пролиферацию и блокирует апоптоз внутри печени. Хроническая гиперинсулинемия также активирует субстрат-1 рецептора инсулина (IRS-1), который играет ключевую роль в регуляции множественных цитокиновых путей, потенциально вовлеченных в патофизиологию ГЦК. Есть данные, что инсулинорезистентность изменяет микробиоту кишки и увеличивает циркуляцию уровня свободных жирных кислот, которые усугубляют печеночный стеатоз.

Предполагается, что понимание влияния коморбидности на прогрессирование НАЖБП, знание интимных механизмов взаимного влияния сопутствующих заболеваний поможет обеспечить более эффективный контроль над заболеванием у коморбидного пациента.
НАЖБП И САХАРНЫЙ ДИАБЕТ 2 ТИПА
Уже много лет известно, что ожирение и СД 2 повышают риск развития ГЦК, но биологическое объяснение этой связи остается не до конца изученным. НАСГ часто встречается у пациентов с ожирением, инсулинорезистентностью, СД 2 и повышает риск развития ГЦК [8]. Тем не менее неясно, существует ли специфический фактор для диабета/ожирения, который увеличивает угрозу развития ГЦК, или общие патологические механизмы, которые возникают как при ГЦК, так и при СД 2/ожирении. Есть данные, что за последние 30 лет отмечается возрастание заболеваемости и смертности от ГЦК примерно в два раза как у мужчин, так и женщин при наличии факторов риска, даже у людей без цирроза печени [9].
M.A. Konerman et al. (2018) проанализировали распространенность СД 2 у взрослых и связь этого заболевания с НАЖБП в США. Глобальная распространенность СД 2 среди взрослых лиц увеличилась с 4,7% в 1980 г. до 8,5% в 2014 г. Показатели встречаемости НАЖБП среди лиц с метаболическим синдромом заметно выше. Приблизительно 1/3 пациентов с артериальной гипертензией, 1/2 пациентов с дислипидемией, 2/3 пациентов с СД 2 и более 90% пациентов, перенесших бариатрическую операцию, имели признаки НАЖБП [10].
Наличие СД 2 также ухудшает гистологические признаки НАЖБП. У пациентов с НАЖБП и СД 2 наблюдается высокая распространенность НАСГ и фиброза, что позволяет считать СД 2 сильным прогностическим фактором тяжести заболевания [11].
Следует добавить, что НАЖБП в сочетании с СД 2 протекает более агрессивно по сравнению с пациентами без диабета, что требует комплексного подхода и оптимальных методов терапии.
НАЖБП И БОЛЕЗНИ СИСТЕМЫ КРОВООБРАЩЕНИЯ
У пациентов с НАЖБП как в сочетании с СД 2, так и без диабета установлена высокая распространенность болезней системы кровообращения (БСК) по сравнению с пациентами без НАЖБП вне зависимости от наличия ожирения и факторов риска БСК. Эпидемиологические исследования показали, что имеется связь между НАЖБП и большей распространенностью коронарных стенозов и повышенной распространенностью атеросклеротических бляшек сонных артерий. На этом фоне противоречивые данные также свидетельствуют об ассоциации между НАЖБП и увеличением частоты смертельных и нефатальных сердечно-сосудистых событий у пациентов с НАЖБП при наличии СД 2 и без СД 2 [12].
В метаанализе с участием 25 837 больных НАЖБП был выявлен более высокий риск развития ишемической болезни сердца (ИБС) по сравнению с группой контроля (RR: 1,77; 95% ДИ: 1,26–2,48; p <0,001). Отличия определялись в наличии повышенной толщины интимы (intima media) сонной артерии, нарушении эндотелиальной потокопосредованной вазодилатации, повышении уровня кальция в коронарных сосудах и наличии маркеров раннего атеросклероза. Кроме того, риск от сердечно-сосудистой смертности был также выше в группе НАЖБП (1,46 РРА; 95% ДИ 1,31–1,64; р <0,001) [13].
Интересными представляются данные исследования по определению распространенности НАЖБП у пациентов с острым коронарным синдромом (ОКС), поступивших в центр скорой помощи. Средний возраст 120 участников – 75 (62,5%) мужчин и 45 (37,5%) женщин – составил 61,28±11,83 года. НАЖБП наблюдали у 56 (46,7%) пациентов с ОКС. Было показано, что у пациентов с НАЖБП отмечался более высокий показатель GRACE, чем у пациентов без НАЖБП (120,2±26,9 против 92,3±24,2; p <0,001). Это также увеличивает смертность от ОКС [14].
A.M. Minhas et al. (2017) провели систематический обзор и метаанализ имеющихся данных о возможной связи риска развития фибрилляции предсердий (ФП) и НАЖБП. В рамках этого исследования были проанализированы группа пациентов с НАЖБП (n=1044) и контрольная группа (n=1016).
Было описано несколько гипотетических механизмов, с помощью которых НАЖБП может привести к ФП:
- При НАЖБП происходит накопление жира в гепатоцитах, отмечается окислительный стресс, что приводит к повышению продукции провоспалительных цитокинов. В результате формируется системное воспаление, выступающее фактором риска ФП.
- На фоне НАЖБП развивается вегетативная дисфункция, при этом нерегулярная симпатостимуляция служит риском развития ФП и может быть причинно-следственной связью между НАЖБП и ФП.
- Ряд исследователей рассматривает НАЖБП как независимый фактор риска развития сердечной диастолической дисфункции и развития ФП.
Таким образом, было отмечено, что у больных НАЖБП в 2,5 раза чаще развивается ФП (OR=2,47; CI=1,30–4,66; p=0,005) [15].
Во Франкфрутском университете доказали связь между наличием и тяжестью ИБС и НАЖБП с помощью транзиторной эластографии и контролируемого параметра затухания (CAP). Пациенты с ИБС показали значительно более высокие значения CAP по сравнению с пациентами без ИБС (235 dB/m при ИБС 0-го функционального класса (ФК), 271 dB/m при ИБС 1-го ФК, 269 dB/m при ИБС 2-го ФК и 273 dB/m при ИБС 3-го ФК).
В группе пациентов с ИБС CAP существенно не отличался в зависимости от различных стадий заболевания. Это справедливо и для распространенности НАЖБП [16].
Коморбидность НАЖБП и БСК – мощный фактор декомпенсированного состояния пациентов, ухудшающий не только прогноз, но и увеличивающий риск полипрагмазии и требующий строгого учета лекарственных взаимодействий.
НАЖБП И ГАСТРОЭЗОФАГЕАЛЬНАЯ РЕФЛЮКСНАЯ БОЛЕЗНЬ
Немаловажную роль в развитии БСК играет коморбидное течение НАЖБП и гастроэзофагеальной рефлюксной болезни (ГЭРБ). К.М. Лю с соавт. (2017) провели теоретический обзор данных, подтверждающих влияние коморбидного течения НАЖБП и ГЭРБ на развитие БСК [17].
K. Wijarnpreecha et al. (2017) провели всесторонний обзор литературы с использованием баз данных MEDLINE и EMBASE до ноября 2016 г. для определения связи НАЖБП и ГЭРБ. В метаанализ были включены 8 исследований (4 перекрестных исследования и 4 исследования «случай–контроль») с 31 322 участниками. Риск НАЖБП среди больных ГЭРБ был значительно выше, чем у пациентов без ГЭРБ, с коэффициентом суммарных шансов 2,07 (95% ДИ, 1,54–2,79). Статистическая неоднородность была высокой – 87%.
J. Xue et al. (2019) для изучения взаимосвязи НАЖБП и ГЭРБ провели системный обзор и метаанализ 7 перекрестных и 2 когортных исследований, включавших 185 118 пациентов, с использованием баз данных PubMed, Scopus, Embase и Web of Science, опубликованных с января 1975 по декабрь 2018 г. Полученные данные свидетельствовали о выраженной связи НАЖБП с высоким риском развития ГЭРБ (суммарное отношение шансов 1,28; 95% ДИ=1,12–1,44) [18].
В настоящее время обсуждаются различные возможные механизмы взаимосвязи НАЖБП и ГЭРБ. Часть ученых придерживается мнения, что связь между НАЖБП и ГЭРБ не причина, а результат влияния общих факторов риска, таких как избыточная масса тела, ожирение, малоподвижный образ жизни, повышенное употребление жиров и газированных напитков. Центральное ожирение является ключевой особенностью метаболического синдрома и связано как с НАЖБП, так и ГЭРБ. Хорошо известно, что висцеральный жир играет важную роль в резистентности к инсулину – главному фактору патогенеза НАЖБП. В то же время повышенное давление в брюшной полости из-за накопления висцерального жира служит причиной повышения давления в желудке, увеличения количества расслаблений кардиального жома и рефлюкса кислого желудочного содержимого в пищевод. Кроме того, висцеральная жировая ткань у человека продуцирует некоторые провоспалительные цитокины, секреция которых приводит к снижению тонуса нижнего пищеводного сфинктера, что может предрасполагать к развитию ГЭРБ.
Однако, по мнению других исследователей, НАЖБП выступает самостоятельным фактором риска развития ГЭРБ. Так, H.J. Yang et al. (2017) в обсервационном исследовании 117 377 пациентов в период с 2002 по 2014 г. была продемонстрирована роль НАЖБП в развитии эрозивного эзофагита – независимая от других факторов, влияющих на обмен веществ (возраста, пола, ИМТ, СД 2, гипертриглицеридемии) [19]. W.C. Hung et al. (2014) опубликовали результаты поперечного исследования с участием 12 090 пациентов, согласно которым установлена независимая от других факторов положительная ассоциация НАЖБП и эрозивного эзофагита. Независимым фактором риска развития эрозивного эзофагита оказалась также гипертриглицеридемия [20].
Интересно, что триглицериды могут влиять на тонус нижнего пищеводного сфинктера, что, возможно, является общим звеном патогенеза, лежащим в основе взаимосвязи между НАЖБП и ГЭРБ. Обсуждается также роль интерлейкинов-1 и -6, которые способствуют снижению двигательной активности пищевода, его клиренса и увеличению времени экспозиции кислоты в пищеводе. Установлено, что оксидативный стресс, снижение антиоксидантной активности и эндотелиальная дисфункция у пациентов с НАЖБП способствуют повреждению и замедлению регенерации слизистой оболочки пищевода. Кроме того, НАЖБП может быть связана с ГЭРБ через дисфункцию вегетативной нервной системы. Исследования показали, что у пациентов с НАЖБП распространенность вегетативных нарушений гораздо выше, она может привести к нарушению моторики желудка и пищевода и, таким образом, к развитию ГЭРБ [21].
Установлено, что при НАЖБП происходит изменение физико-химического состава желчи. По данным разных авторов, у 50–70% больных НАЖБП встречается билиарный сладж, желчнокаменная болезнь и нарушения моторики билиарного тракта. В свою очередь, нарушения моторики билиарного тракта, сопровождающиеся дуоденогастроэзофагеальным рефлюксом, могут способствовать повреждению, метаплазии и дисплазии эпителия слизистой оболочки пищевода.
Учитывая патогенетические механизмы развития ГЭРБ и НАЖБП, одновременное наличие осложняет течение этих заболеваний в несколько раз, что также требует адекватного диагностического и терапевтического подхода.
НАЖБП И HELICOBACTER PYLORI
Существуют интересные данные о связи между инфекцией Helicobacter pylori (H. pylori) и риском развития НАЖБП. A. Mantovani et al. (2019) провели систематический обзор 13 обсервационных (11 поперечных и 2 продольных) исследований, в которых участвовало в общей сложности 81 162 человека среднего возраста, преимущественно азиатского происхождения (47,5% из них имели инфекцию H. pylori). Метаанализ данных перекрестных исследований и исследований «случай–контроль» показал, что инфекция H. pylori была связана с повышенным риском развития НАЖБП (n=11 исследований; отношение шансов случайных эффектов 1,20; 95% ДИ 1,07–1,35; I2=59,6%). Этот риск оставался значительным в тех исследованиях, где анализ был полностью скорректирован по возрасту, полу, курению, показателям ожирения, диабету или дислипидемии (случайные эффекты ИЛИ 1,19; 95% ДИ 1,07–1,32, I2=0%). Метаанализ данных продольных исследований показал, что инфекция H. pylori также была связана с повышенной заболеваемостью НАЖБП (n=2 исследования; коэффициент риска случайных эффектов 1,14, 95% ДИ 1,05–1,23; I2=0%) [22].
Независимо от метаболических и воспалительных факторов риска очевидна связь H. pylori и НАЖБП. Инфекция H. pylori может играть патофизиологическую роль в развитии НАЖБП. С другой стороны, следует учитывать то, что эрадикация H. pylori может влиять на снижение риска НАЖБП.
НАЖБП И ДИСЛИПИДЕМИЯ
Расстройства липидного обмена при НАЖБП – один из кардинальных признаков заболевания. По данным А.Б. Кривошеева с соавт. (2016), у мужчин чаще встречается тяжелая гиперхолестеринемия (более 7,8 ммоль/л). Дислипидемия при НАЖБП характеризуется повышением уровня триглицеридов >1,7 ммоль/л и гипоальфахолестеринемией, при этом уровень ХС ЛПВП <1,0 ммоль/л у мужчин и <1,2 ммоль/л у женщин, что является диагностическим критерием для НАЖБП [5, 23].
Подводя итоги, можно констатировать, что поражение печени потенцирует дислипидемию, тем самым нарушая работу эндотелия сосудов. Это также способствует развитию и более тяжелому течению атеросклероза, повышенному риску ИБС, инфаркта миокарда и инсульта.
НАЖБП И ХРОНИЧЕСКАЯ БОЛЕЗНЬ ПОЧЕК
В последнее время привлекает значительный научный интерес связь между НАЖБП и хронической болезнью почек (ХБП) [24].
В крупных перекрестных популяционных исследованиях, в которых участвовали как взрослые без диабета, так и пациенты с диабетом, показано, что распространенность ХБП (верифицируемая при снижении скорости клубочковой фильтрации и/или протеинурии) увеличивается у пациентов с НАЖБП. Диагноз НАЖБП в этих исследованиях был подтвержден либо с помощью УЗИ, либо биопсии печени с исключением пациентов с терминальной почечной недостаточностью и цирроза печени в исходе хронических заболеваний печени (злоупотребление алкоголем, вирусный гепатит и применение гепатотоксичных лекарств во всех исследованиях, гемохроматоз и аутоиммунный гепатит). В этих исследованиях распространенность ХБП у пациентов с НАЖБП варьировала от 20 до 55% по сравнению с 5–35% у пациентов без НАЖБП. Кроме того, наличие и тяжесть НАЖБП были связаны со стадиями ХБП независимо от установленных факторов сердечно-почечного риска [24].
В систематическом обзоре и метаанализе 20 поперечных и 13 продольных исследований (63 902 пациента) Musso et al. (2014) подтвердили, что диагноз НАЖБП, диагностированный с помощью гепатобиопсии, был в значительной степени связан с повышенным риском распространенности (ОШ 2,12; 95% ДИ 1,69–2,66) и возникновения ХБП (ОШ 1,79; 95% ДИ 1,65–1,95). Кроме того, НАСГ был связан с более высокой распространенностью (ОШ 2,53; 95% ДИ 1,58–4,05) и частотой ХБП (ОШ 2,12; 95% ДИ 1,42–3,17), чем простой стеатоз [26].
Представляется, что раннее выявление поражения почек у больных НАЖБП позволит подобрать правильные дозы лекарственных препаратов, избегая побочных эффектов.
НАЖБП И ВОСПАЛИТЕЛЬНЫЕ ЗАБОЛЕВАНИЯ КИШЕЧНИКА
На сегодня данные литературы свидетельствуют о частоте выявления НАЖБП среди пациентов с воспалительными заболеваниями кишечника (ВЗК) в диапазоне от 1,5 до 40%. Такая вариабельность частоты связана с использованием различающихся нестандартизированных критериев для верифицирования НАЖБП. В современной литературе имеются данные, что развитие НАЖБП у больных ВЗК, возможно, связано с применением медикаментов (таких как стероиды), изменениями микробиома кишки с вовлечением в воспалительный процесс тонкой кишки, резекциями кишечника, а также с распространенностью поражения в кишке и дефицитом питания [29, 31, 32, 34, 37].
Так, J. Silva et al. (2019) в исследовании, включавшем 306 больных ВЗК, определили частоту НАЖБП в обследуемой когорте как 7,2% [28].
Напротив, по данным новосибирских авторов (Краснер Я.А. и соавт.), при анализе данных 245 больных ВЗК отмечена более высокая частота выявления стеатоза: у 34,2% пациентов с болезнью Крона и у 30,4% с язвенным колитом. При этом на различия в частоте выявления НАЖБП влияли применение в анамнезе глюкокортикостероидов (63,6 против 53%; р=0,0006), большая длительность ВЗК (медиана 5,9 года; Q1/Q3 – 2,7/12,9 года против 4,5; 2,9/8,5 года; р=0,0324) и ИМТ (медиана 24,1; Q1/Q3 – 21,4/29,9 против 21; 18,6/23,5; p=0,0336). Интересным результатом проведенной работы стало выявление синдрома избыточного бактериального роста как независимого фактора, ассоциированного с более высокими шансами развития НАЖБП у пациентов с ВЗК, с увеличением таковых до 2,34 (ОШ 2,34; 95% ДИ 1,4–4,8; р=0,021) [27].
Т. Bessissow et al. в 2016 г. опубликовали результаты исследования с участием 321 больных ВЗК без скомпрометированной печени с последующим длительным наблюдением (средний период наблюдения 3,2 года). Итогом работы явилось заключение о том, что НАЖБП – частая сопутствующая патология при ВЗК, развивающаяся у 33,6% больных, с заболеваемостью 9 на 100 пациенто-лет. За период наблюдения НАЖБП в большей степени развивалась у пациентов с наличием диабета и при более высоком уровне ИМТ [29].
Однако в целом распространенность диабета и ожирения в популяции пациентов с одновременным наличием ВЗК и НАЖБП невысока. Это позволяет сделать вывод об иных, помимо метаболического, триггерах развития НАЖБП.
Некоторые авторы выдвигают гипотезу о взаимосвязи патогенеза НАЖБП у больных ВЗК со специфическими для заболевания факторами, связанными, например, с воспалением и его активностью. С этой точки зрения активность и продолжительность заболевания, вовлечение тонкой кишки в воспаление, использование стероидов, операции на тонкой кишке и изменения микробиоты могут быть предикторами НАЖБП у таких пациентов [30, 33].
K. Glassner, H.M. Malaty et al. в 2017 г. опубликовали результаты исследования, целью которого была попытка выявить факторы риска развития НАЖБП у пациентов с ВЗК. Исследователи пришли к заключению, что НАЖБП на фоне ВЗК развивается при статистически значимо меньшем количестве метаболических факторов риска, по сравнению с группой изолированного неалкогольного жирового поражения печени. Среди больных ВЗК с НАЖБП реже выявлялись ожирение (40 против 59%; р=0,03), гиперлипидемия (17,5 против 53%; р=0,03), диабет (16 против 40%; р <0,0001) и гипертония (33 против 55%; р=0,02) по сравнению с группой больных с НАЖБП без ВЗК [32].
В то же время ретроспективное когортное исследование R.M. Carr et al. (2017) с анализом 84 больных ВЗК и доказанной НАЖБП продемонстрировало, что тяжесть НАЖБП при наличии метаболического синдрома в большей степени зависит от его выраженности, а не тяжести течения ВЗК. В то же время, как и у пациентов без метаболического синдрома, тяжесть НАЖБП была ассоциирована с активностью ВЗК и фактом приема стероидов [30].
В одной из крупных работ по этой тематике, выполненной и опубликованной A. Sartini et al. в 2018 г., были установлены факторы риска тяжелого стеатоза у пациентов с ВЗК и факторы риска развития гипертрансаминаземии при сочетании НАЖБП с ВЗК [36].
В результате исследования авторами было определено, что риск тяжелого стеатоза (степень S3) у больных ВЗК в 17,3 раза выше при наличии более чем одного рецидива ВЗК в течение года болезни (ОШ 17,3; 95% ДИ 3,6–84; р <0,001) и в 15,1 раз выше у пациентов с оперированной кишкой по поводу ВЗК (ОШ 15,1; 95% ДИ 3,1–73,7; р=0,001) и в 19,4 раза выше при распространенном поражении кишечника (ОШ 19,4; 95% ДИ 3,4–110,9; р=0,001). При этом наличие метаболического синдрома не было ассоциировано с развитием тяжелого стеатоза (р=0,48), и в целом у пациентов с сочетанием ВЗК и НАЖБП частота метаболического синдрома была меньше по сравнению с больными НАЖБП без ВЗК (18 против 56%, р <0,0001) [36].
Факторами, ассоциированными с повышением уровня трансаминаз при наличии НАЖБП у больных с ВЗК, по результатам исследования оказались: тяжелый стеатоз (S3) (ОШ 3,5; 95% ДИ 1,3–9,3; р=0,01), распространенное ВЗК (ОШ 3,2; 95% ДИ 1,2–8,1; р=0,02), а текущая терапия ингибиторами ФНО-α, напротив, стала единственным фактором, снижающим уровень трансаминаз у этой категории пациентов (ОШ 0,2; 95% ДИ 0–0,8; р= 0,03) [36].
В научной литературе есть сведения о том, что наличие первичного склерозирующего холангита (ПСХ) у пациентов с ВЗК служит протективным фактором против развития стеатоза, хотя на сегодняшний день взаимовлияния НАЖБП и ПСХ не изучены [35].
Таким образом, по сумме литературных данных можно сделать вывод о том, что более тяжелое течение ВЗК способствует развитию стеатоза печени, а тяжелый стеатоз, в свою очередь, дополнительно ухудшает течение ВЗК. Известно, что у НАЖБП и ВЗК есть точки соприкосновения в патогенезе развития заболевания – это повышенная проницаемость кишки и изменения микробиома [34], однако необходимы дальнейшие исследования для изучения патоморфологических механизмов связи этих патологий с поиском патогенетических возможностей их разрешения.
НАЖБП И ХРОНИЧЕСКАЯ ОБСТРУКТИВНАЯ БОЛЕЗНЬ ЛЕГКИХ
В настоящее время активно изучается сочетанное течение НАЖБП и хронической обструктивной болезни легких (ХОБЛ). Связано это с общими звеньями патогенеза, такими как оксидативный стресс и системное воспаление. НАЖБП недостаточно изучена у пациентов с ХОБЛ, хотя существует обоснование, подтверждающее гипотезу о высокой распространенности НАЖБП у пациентов с ХОБЛ. До сих пор ведутся споры по поводу теории «перетекания»: окислительный стресс и системное воспаление, о существовании которых сообщалось при некоторых подтипах ХОБЛ, могут участвовать в выработке активных форм кислорода и воспалении печени. Пациенты с ХОБЛ имеют увеличенный висцеральный жир, что приводит к накоплению свободных жирных кислот в печени, а это может приводить к развитию НАЖБП.
В последнее время отдельно выделяют пациентов с формой ХОБЛ в сочетании с метаболическим синдромом. В исследовании D. Jung et al. с участием 2119 корейцев, страдающих НАЖБП, всем больным было выполнено исследование по изучению функции внешнего дыхания. У пациентов с НАЖБП уровень жизненной емкости легких (ЖЕЛ) и объем форсированного выдоха за 1 с (ОФВ1) был ниже по сравнению с контрольной группой. Ухудшение показателей функции внешнего дыхания коррелировало со степенью ожирения печени [38].
Изучение сочетанной легочной патологии и НАЖБП актуально в связи с высоким риском летальных исходов у больных ХОБЛ с присоединением сопутствующих заболеваний. Вопрос изучения данной коморбидной патологии до конца не изучен и имеет как практическую, так и теоретическую значимость в современной медицине.
НАЖБП И ВИЧ
Особый контингент составляют пациенты с ВИЧ-инфекцией, среди которых частота встречаемости стеатоза печени достигает примерно 30%. Немаловажным фактором, способствующим формированию жировой дистрофии печени, служит коинфекция ВИЧ и хронического гепатита C.
В мире насчитывается примерно 2 278 400 таких пациентов, а распространенность стеатоза среди них может достигать 40–72%.
Риск развития НАЖБП при ВИЧ возрастает с каждым годом лечения. Известно, что нуклеозидные ингибиторы обратной транскриптазы приводят к развитию стеатоза за счет блокирования митохондриальной ДНК-полимеразы-γ, снижая тем самым интенсивность репликации митохондриальной ДНК. Это ведет к депонированию триглицеридов, в том числе в печени. Ингибиторы протеазы, которые входят в схемы лечения ВИЧ инфекции, стимулируют развитие стеатоза печени посредством усиленной экспрессии SREBP-1 [39, 40].
НАЖБП И ХРОНИЧЕСКИЙ ГЕПАТИТ С
Ожирение играет важную роль в развитии стеатоза печени на фоне течения HCV-инфекции, особенно у пациентов с генотипом 1. Абдоминальное ожирение у пациентов с хроническим гепатитом С приводит к развитию инсулинорезистентности и НАЖБП в 50% случаев. HCV-инфекция в течение своего жизненного цикла нарушает липидный обмен и может вызывать стеатоз печени и резистентность к инсулину. Стеатоз печени, определяемый как чрезмерное отложение триглицеридов в гепатоцитах, встречается примерно в половине случаев инфицирования вирусом гепатита С.
Генетические факторы и коморбидное течение НАЖБП с хроническим гепатитом C могут приводить к прогрессированию стеатоза, который, в свою очередь, может способствовать усилению фиброза и развитию цирроза печени и ГЦК. Наличие полиморфизмов в генах, которые модулируют отложение липидов в гепатоцитах, таких как белок 3, содержащий пататин-подобный фосфолипазный домен (PNPLA3) и трансмембранный член 6 суперсемейства 2 (TM6SF2), создает предпосылки к стеатозу [41, 42].
Есть сведения о том, что развитие стеатоза при хроническим гепатите C напрямую связано с 3 генотипом HCV и может приводить к инсулинорезистентности. С другой стороны, коррекция инсулинорезистентности перед противовирусной терапией приводила к повышению эффективности лечения при применении интерферон-содержащих схем [43–45].
Учитывая представленные факты, становится понятной актуальность не только проведения скрининга на HCV-инфекцию в различных группах населения с целью своевременной противовирусной терапии для излечения от хронического гепатита С, но и для профилактики таких различных социально значимых заболеваний, как НАЖБП, СД 2, патологии системы кровообращения и т.д.
ЗАКЛЮЧЕНИЕ
Данные литературы свидетельствуют о рисках коморбидности при НАЖБП и наличии в каждом втором случае сопутствующей патологии со стороны сердечно-сосудистой, эндокринной, мочевыделительной и других систем. Коморбидное течение НАЖБП хотя бы с одной из вышеперечисленных патологий может приводить к запуску патогенетических мультифакторных механизмов, приводя к развитию агрессивных осложнений. Считается доказанным взаимное влияние на развитие НАЖБП патологий сердечно-сосудистой системы, СД 2, дислипидемии.
Не вызывает сомнения повышение риска НАЖБП при длительной медикаментозной терапии у пациентов с различной хронической патологией (ХОБЛ, ХБП и др.). Представляется интересным дальнейшее изучение причин повышения заболеваемости НАЖБП при ВЗК, хеликобактерной инфекции, ГЭРБ и др. Изучение данных взаимоотношений и механизмов их развития требует накопления опыта и проведения дальнейших научных исследований, так как существует возможность не только истинных сочетаний в клинике внутренних болезней, но и ятрогений. При различных комбинациях коморбидных состояний у пациентов с НАЖБП возникают вопросы не только относительно патогенеза, но и рационального лечения сочетанных патологий. Поэтому своевременное выявление факторов коморбидности и лечение сопутствующих заболеваний – ключ к успеху в комплексной терапии НАЖБП.