ВВЕДЕНИЕ
Повышение уровня мочевой кислоты сыворотки крови служит независимым фактором сердечно-сосудистого риска, способствующим развитию дисфункции эндотелия и быстрому прогрессированию всех составляющих метаболического синдрома [1, 2]. Известно, что повышение уровня мочевой кислоты ассоциировано с хронической болезнью почек [1, 2]. Снижение скорости клубочковой фильтрации (СКФ) связано с нарастанием гиперурикемии, а кристаллизация мочевой кислоты приводит к поражению как клубочкового, так и канальцевого аппарата почки и снижению СКФ, в еще большей степени повышая сердечно-сосудистый риск [3–5]. При этом отсутствие подагрического артрита у пациента с гиперурикемией не исключает увеличения кардиоваскулярного риска и риска поражения почек [2, 3]. Судя по данным литературных источников, критическими фактором поражения сосудов и почек является кристаллизация мочевой кислоты. Она, в свою очередь,зависит от многих условий, ведущим из которых является уровень самой мочевой кислоты [3–5].
В настоящий момент остается неясным, может ли нормализация уровня мочевой кислоты приводить к снижению сердечно-сосудистого риска и может ли на фоне улучшения функции почек снижаться суммарный риск кардиоваскулярных осложнений у этой категории пациентов [6–8]. Отсутствует и четкое понимание того, когда и при каких условиях необходимо лекарственное вмешательство при наличии бессимптомной гиперурикемии [6–9].
В крупных исследованиях уратснижающего лечения с применением фебуксостата и аллопуринола получены довольно разноречивые результаты [9]; это может быть обусловлено проблемой множественных сравнений в больших выборках, а также с тем, что в этих работах анализировались возможности улучшения функции почек при использовании уратснижающей терапии без контроля ее эффективности с точки зрения достижения целевого уровня мочевой кислоты. Поэтому в большинстве исследований не указано, на фоне какого целевого уровня мочевой кислоты проводился анализ динамики СКФ.
Отдельный фактор, определяющий отсутствие нормализации функции почек на фоне снижения уровня мочевой кислоты, – наличие первичной причины их поражения (например, волчаночного нефрита, АНЦА-васкулитов и др.). Мы понимаем, что в этом случае восстановление утраченной функции невозможно, так как гипериукемия здесь выступает не причиной, а следствием хронической болезни почек (ХБП).
С учетом указанных выше факторов представляется актуальным отслеживание клинических случаев, в которых наблюдалось увеличение СКФ при нормализации мочевой кислоты сыворотки крови.
Цель представленной работы – описание клинических случаев увеличения СКФ у пациентов с ХБП 3С стадии с высоким сердечно-сосудистым риском на фоне стойкой нормализации уровня мочевой кислоты сыворотки крови, обусловленной приемом фебуксостата.
МАТЕРИАЛ И МЕТОДЫ
Проведен анализ медицинской документации пациентов с бессимптомной гиперурикемией, наблюдавшейся не менее 5 лет. За бессимптомную гиперурикемию принималось зафиксированное более двух раз с интервалом более чем 1 мес, повышение уровня мочевой кислоты более 360 мкмоль/л. Расчет СКФ и определение стадий ХБП выполнялись в соответствии с рекомендациями KDIGO (2012).
РЕЗУЛЬТАТЫ
Мы наблюдали двух пациентов с однотипной клинической ситуацией, у которых, по данным медицинской документации, мочевая кислота крови была повышена (>500 мкмоль/л) в течение не менее 5 лет. В этот же период времени у обоих пациентов наблюдалось снижение СКФ до 3С стадии ХБП. Патология почек в рамках системных аутоиммунных и воспалительных заболеваний была исключена.
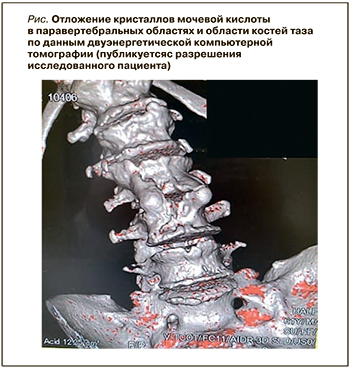
Также у обоих участников наблюдения клинически и по результатам ультразвукового исследования (УЗИ) первого плюснефалангового сустава была исключена подагра. Пациенту 1958 г.р. была выполнена двуэнергетическая компьютерная томография, подтвердившая отложение кристаллов мочевой кислоты в мягких тканях паравертебральной области и костей таза (рис.). Клинико-демографические характеристики исследованных пациентов представлены в таблице 1.
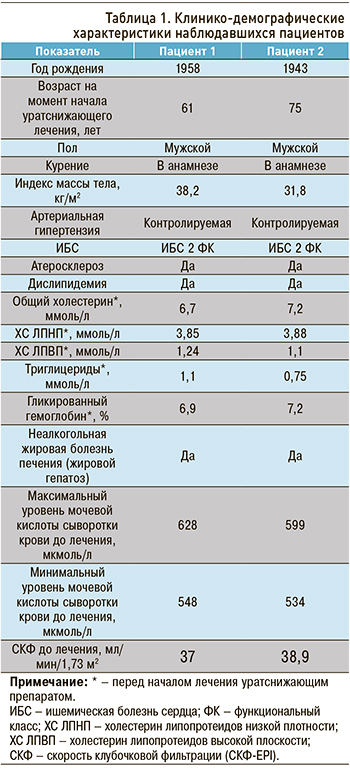
В общем анализе мочи у обоих пациентов значимых изменений выявлено не было, наблюдалась протеинурия, не превышающая 0,3 г/л. При УЗИ почек патологических изменений также не обнаружено; результат дуплексного исследования почечных артерий – без патологии.
Пациенты постоянно соблюдали низкоуглеводную диету с учетом наличия у них сахарного диабета 2-го типа и получали антигипертензивную терапию – ингибиторы АПФ, блокаторы кальциевых каналов, бета-блокаторы, мочегонные препараты (индапамид), статины (аторвастатин), метформин (1000 мг/сут). На момент начала уратснижающей терапии у наблюдавшихся имела место контролируемая артериальная гипертензия.
С учетом высокого риска сердечно-сосудистых осложнений пациентам был назначен фебуксостат (выбор препарата определялся с учетом мнения пациентов, не имевших возможность должным образом титровать дозу аллопуринола). Оба участника исходно получали фебуксостат в дозе 80 мг/сут, которая для достижения целевого уровня на 3 мес была увеличена до 120 мг/сут со снижением до исходной дозировки в последующем. За 6 мес лечения пациенты достигли уровня мочевой кислоты менее 360 мкмоль/л. Однако с учетом наличия у них высокого сердечно-сосудистого риска целевым было решено считать уровень этого биомаркера ≤300 мкмоль/л. Указанная концентрация мочевой кислоты была достигнута в течение 12 и 9 мес с момента назначения фебуксостата соответственно (табл. 2).
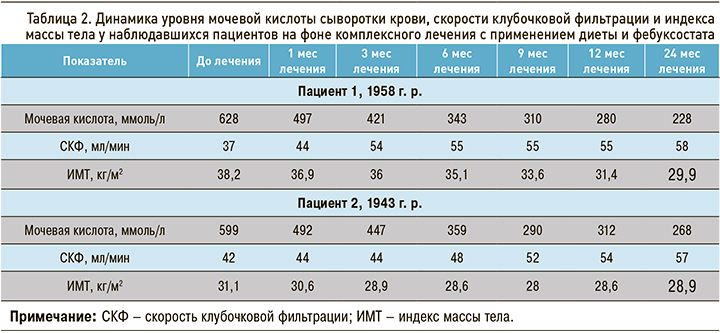
На фоне комплексного лечения с применением фебуксостата у пациентов наблюдалось снижение массы тела, уменьшение потребности в антигипертензивных препаратах (снижение дозировок ингибиторов АПФ вдвое от исходных), увеличение толерантности к физическим нагрузкам (с 3 до 6 тыс шагов в среднем в сутки, по оценкам с помощью шагомера).
На фоне нормализации мочевой кислоты было установлено и постепенное улучшение функции почек (увеличение СКФ, см. табл. 2).
Оба пациента констатировали улучшение общего состояния своего здоровья по 10-балльной шкале, где 0 – абсолютное здоровье, а 10 – наихудшее состояние болезни. Пациент 1958 г.р. отметил снижение влияния болезни на жизнь с 7 до 3 баллов, пациент 1943 г.р. – с 8 до 5 баллов.
ОБСУЖДЕНИЕ
Представленные нами сходные клинические ситуации показывают возможность увеличения СКФ за счет коррекции уровня мочевой кислоты и других факторов сердечно-сосудистого риска. Причиной ХБП у обоих пациентов, по-видимому, является комплексное воздействие факторов сердечно-сосудистого риска на клубочковый и канальцевый аппарат почек. Указанное предположение основано на наших знаниях о патогенетических механизмах развития клубочковой и канальцевой дисфункций у пациентов с высоким кардиоваскулярным риском, среди которых немаловажную роль играет повышение уровня мочевой кислоты крови [4, 5, 10, 11].
Тот факт, что снижение уровня мочевой кислоты на фоне комплексного лечения с применением фебуксостата привело к постепенному увеличению СКФ и уменьшению потребности в антигипертензивных препаратах, косвенно подтверждает данные экспериментальных исследований, демонстрирующих способность мочевой кислоты оказывать прямое повреждающее воздействие на эндотелий клубочкового аппарата почек и канальцевый аппарат [4, 5, 10, 11]. Наше наблюдение показывает, что такие изменения могут быть частично обратимыми.
Полученные результаты противоречат общим результатам плацебо-контролируемого исследования, выполненного Kimura K. et al. (2018), где было продемонстрировано отсутствие статистически достоверной разницы в изменении СКФ у пациентов, получавших фебуксостат [12]. Однако следует отметить, что в указанное исследование включали пациентов с любыми причинами ХБП и гиперурикемии, т.е. не исключено, что часть из них имела первичные причины поражения почек, отличные от гиперурикемии. В такой ситуации ждать улучшения функции почек не следует, так как снижение их функции поддерживается неметаболической причиной. Подобное заключение делают и сами авторы обсуждаемой работы: так, в группах фебуксостата и плацебо показана разноплановая динамика СКФ (увеличение этого показателя в группе фебуксостата и уменьшение в группе плацебо). Кроме того, в приведенном исследовании в подгруппе пациентов без значимой протеинурии были достигнуты статистически значимые различия в изменении СКФ между фебуксостатом и плацебо, и это опять же подтверждает постулат о том, что увеличения СКФ следует ждать при проведении уратснижающего лечения только тогда, когда нет других (вне метаболического синдрома) факторов повреждения клубочкового или канальцевого аппаратов почек [12].
Результаты других клинических исследований и метаанализов свидетельствуют, что интервенции с применением уратснижающего лечения, включающего фебуксостат, имеют преимущество перед отсутствием вмешательства в отношении улучшения СКФ [13]. К примеру, в метаанализе Gherghina M.E. et al. (2019), охватившем 11 клинических исследований с 1317 участниками, было продемонстрировано, что прием флебуксосотата не только значимо снижает уровень мочевой кислоты, но и ассоциируется с более высокой СКФ (средний уровень 2,36 мл/мин/1,73 м2; 95% доверительный интервал: 1,62–6,33) у пациентов с 3 и 4 стадиями ХБП по сравнению с группой плацебо [11].
В свою очередь, в многоцентровом 36-месячном наблюдении Verdoux H. et al. (2019), включившем 1070 пациентов старшей возрастной категории с высоким риском сердечно-сосудистых катастроф и гиперурикемией, в группе пациентов, получавших фебуксостат, прогрессирование микроальбуминурии, протеинурии и повышение креатинина отмечалось значимо реже. Более того, у пациентов, находившихся на уратснижающей терапии этим препаратом, не наблюдалось и прогрессирования ХБП [14]. Hsu Y.O. et al. выявили снижение на фоне приема фебуксостата риска трансформации преддиализной ХБП в диализную у пациентов с 5-й стадией этого заболевания [15].
В 2018 г. было опубликовано исследование CARES, показавшее повышение риска смерти от всех причин в группе фебуксостата по сравнению с аллопуринолом [16]. Однако к представленным данным следует относиться очень осторожно по двум причинам. Во-первых, в CARES имела место необычно высокая частота выбываний участников из исследования (56,6% в режиме исследования и 46% в ходе наблюдения), во-вторых же, не исключено, что врачи назначали фебуксостат преимущественно пациентам, имеющим ограничения к применению аллопуринола, что и определило повышение риска смерти от всех причин.
В этом плане показательны результаты метаанализа 17 исследований, выполненного Zhao L. et al. (2020): в нем было установлено отсутствие различий в сердечно-сосудистой и общей смертности пациентов, получающих фебуксостат и аллопуринол [17].
Возвращаясь к обсуждению полученных нами результатов лечения в сравнении с представленными литературными данными, необходимо остановиться на том, что результативность уратснижающей терапии в плане улучшения функции почек зависит не от самого факта применения препаратов, снижающих мочевую кислоту, а от их эффективности. В представленных нами случаях четко прослеживается взаимосвязь между уровнем мочевой кислоты и СКФ, причем оптимальный эффект был достигнут нами после снижения мочевой кислоты <300 мкмоль/л. Получение такого результата потребовало временного увеличения дозы фебуксостата до 120 мг/сут. В большинстве публикаций, демонстрирующих влияние фебуксостата на СКФ, не указано, какое число пациентов достигло того или иного целевого уровня мочевой кислоты сыворотки крови и насколько стойким был эффект лечения [11, 13–16]. Это обстоятельство может объяснять недостижение улучшения почечной функции пациентами, у которых гиперурикемия не разрешилась или у которых улучшение пуринового обмена носило нестойкий характер.
Добавим, что на результатах ряда исследований могло негативно сказаться отсутствие комплексного воздействия на факторы сердечно-сосудистого риска, т.е. проведение уратснижающей терапии без одновременной коррекции образа жизни, пищевых привычек, дислипидемии и артериальной гипертензии [2, 9, 17, 18]. В представленных же нами наблюдениях указанные комплексные меры были назначены кардиологом и эндокринологом за несколько месяцев до начала уратснижающего лечения. В целом при лечении пациентов высокого сердечно-сосудистого риска эффективность терапии определяется сочетанным влиянием немедикаментозных и медикаментозных мер на коррекцию факторов риска, при этом достижение должного уратснижающего эффекта, как и нормализация СКФ у лиц с высоким уровнем мочевой кислоты, без назначения уратснижающих лекарственных препаратов (в нашем варианте – фебуксостата) невозможно [19].
ЗАКЛЮЧЕНИЕ
Приведенные нами наблюдения иллюстрируют возможность улучшения почечной функции на фоне стойкой нормализации уровня мочевой кислоты крови у пациентов с ХБП 3С и высоким сердечно-сосудистым риском при использовании комплексного лечения, включающего фебуксостат.



