Концепция моноклональной гаммапатии ренального значения (МГРЗ), предложенная Международной группой по изучению поражения почек и моноклональной гаммапатии (International Kidney and Monoclonal Gammopathy Research group) [1, 2], подразумевает патологическое состояние, обусловленное пролиферацией клона В-клеток или плазматических клеток, не достигающего критериев, необходимых для начала лечения по онкогематологическим показаниям, но продуцирующего нефротоксичный моноклональный иммуноглобулин (ИГ), что приводит к специфическому повреждению почек с неуклонным прогрессированием ренальной дисфункции и ухудшением прогноза болезни. Прогрессирование дисфункции почек, вплоть до утраты функции органа, согласно принятому международными экспертами мнению, является определяющим при решении вопроса в пользу назначения лечения, направленного на элиминацию патологического клона, несмотря на отсутствие критериальных онкогематологических показаний.
В России в последние годы появился ряд публикаций, посвященных МГРЗ, авторами которых были нефрологи [3–6]. Вместе с тем описанные ими клинические случаи очевидной связи аберрантного клона (порой минорного) и поражения почек остаются недостаточно распознаваемыми и врачами, и органами управления здравоохранением. Манифестация МГРЗ, как правило, связана не с клон-ассоциированными симптомами, а с такими общими «терапевтическими» симптомами, как артериальная гипертензия (АГ), отеки, протеинурия, прогрессирующая дисфункция почек. Пациенты с МГРЗ зачастую являются первичными пациентами врачей общей практики и терапевтов. В связи с недостаточной осведомленностью врачей первичного звена и специалистов в отношении МГРЗ, отсутствием утвержденных рекомендаций и медико-экономических стандартов лечения возникает ряд организационных проблем, включая недоступность для большинства пациентов эффективной, своевременной диагностики и лечения.
Применение эффективной терапии МГРЗ ограничено устаревшими подходами и стандартами оказания медицинской помощи, основанными главным образом на гематологических критериях начала лечения. Такой подход не является верным в отношении МГРЗ, при которой «небольшой» клон опасен и угрожает жизни [7–11], а своевременная терапия приводит к значимому улучшению прогноза [12–15]. Консенсус ведущих гематологов и нефрологов страны [16] призван наметить пути практического решения проблем диагностики и лечения МГРЗ в России, критичных для этой категории больных. Далее от имени Рабочей группы и профессиональных сообществ приводится сокращенный вариант текста Консенсуса [16], предназначенный для ознакомления с проблемой МГРЗ широкого круга специалистов, в первую очередь врачей первичного звена, которые должны хорошо понимать эту патологию для оптимизации путей маршрутизации пациента с точки зрения его обследования и консультации узкими специалистами.
ПОНЯТИЕ О МОНОКЛОНАЛЬНОЙ ГАММАПАТИИ РЕНАЛЬНОГО ЗНАЧЕНИЯ
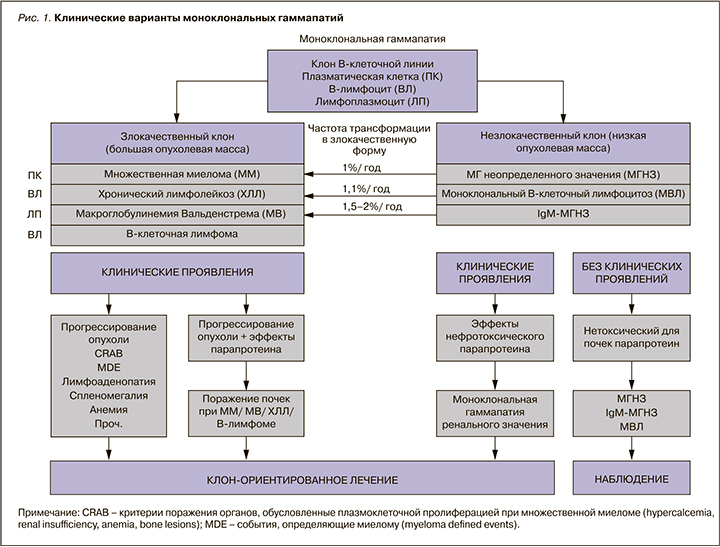
Под моноклональной гаммапатией (МГ) понимают наличие аберрантного клона B-клеточной линии дифференцировки, продуцирующего молекулу ИГ или ее части. Современный взгляд в отношении группы нозологий, обусловленных МГ, и место МГРЗ в классификации представлены на рисунке 1.
Клон – популяция клеток, возникшая из одной клетки-предшественницы и наследующая все ее свойства, в том числе способность продуцировать моноклональный парапротеин. Вырабатываемый моноклональный белок, называемый парапротеином или М-протеином, может обладать патологическими свойствами, которые реализуются различными путями, включая депозицию в органах и тканях, приводя к их повреждению.
Клинические проявления МГ связаны с: а) увеличением опухолевой массы; б) патологическими эффектами ИГ. Основная часть случаев МГ протекает субклинически, что отражает более ранние стадии болезни и входит в понятие моноклональной гаммапатии неопределенного значения (МГНЗ) (или моноклонального В-клеточного лимфоцитоза в случае лимфоцитарной пролиферации). В большинстве случаев МГНЗ продуцируемый парапротеин не обладает нефротоксичностью (т.е. способностью оказывать то или иное повреждающее воздействие на орган). Это состояние имеет благоприятное течение с частотой прогрессирования в злокачественную форму около 1% в год [17–19]. Увеличение массы опухоли приводит к поражению органов в виде симптомов CRAB (С – hypercalcemia; R – renal insufficiency; A – anemia; B – bone lesions) при множественной миеломе (ММ); лимфаденопатии, гепатоспленомегалии, признаков неопластического подавления кроветворения и другого при хроническом лимфолейкозе (ХЛЛ) и макроглобулинемии Вальденстрема. Появление таких симптомов является показанием к лечению.
Другая часть клинического спектра обусловлена эффектами парапротеина и его повреждающим действием на ткани и органы, включая почки. Симптомы, обусловленные парапротеином, могут возникать даже при низкой опухолевой массе и небольшой концентрации парапротеина в циркуляции. Концепция «небольшого, но опасного клона» при МГ, впервые предложенная Merlini G. и Stone M.J. в 2006 г. [20], предполагает клинически доминирующие органные поражения и ухудшение прогноза, вызванные патологическими эффектами парапротеина, но не прогрессией опухоли как таковой. Для описания подобных случаев недавно предложен термин «МГ клинического значения» [21].
МГРЗ – термин, который дифференцирует известное понятие МГНЗ, выводя ряд клинических случаев из рамок «неопределенности». МГРЗ также характеризуется клоном, который ниже уровня, соответствующего критериальному диагнозу ММ или лимфопролиферативного заболевания, требующего начала лечения. По данным НИИ нефрологии, среднее значение плазматизации костного мозга при МГРЗ составило 2,2%, а уровень парапротеина в сыворотке – 1,1 г/л [4, 22]. Вместе с тем в отличие от случаев МГНЗ продуцируемый М-протеин при МГРЗ обладает нефротоксичностью и приводит к клинически значимому повреждению почек, а также других органов. Нефротоксичный моноклональный ИГ может вырабатываться как при низкой, так и большой опухолевой массе. Если имеют место основания для критериального диагноза злокачественной пролиферации клона В-клеточной линии дифференцировки и поражения почек, это говорит о том, что продуцируемый парапротеин нефротоксичен. Такие случаи не относят к МГРЗ, при формулировке диагноза на первое место ставят гематологическую опухоль, а поражение почек считают осложнением. В случае нефротоксичности моноклонального парапротеина и «небольшого» клона диагноз должен быть определен как МГРЗ с расшифровкой характера поражения почек, ключевым в определении которого является морфологическое исследование почечной ткани.
ЭПИДЕМИОЛОГИЯ И ПРОГНОЗ
Поражение почек, обусловленное парапротеином, – нечастая патология в структуре болезней почек. По данным НИИ нефрологии, распространенность патологии почек, связанной с каким-либо вариантом МГ, составляет 7,5% среди всех пациентов, которым была выполнена диагностическая нефробиопсия. При этом МГРЗ была выявлена у 4% больных [4]. Эти цифры соотносятся с данными, представленными в мировой литературе [11, 23]. Заболеваемость МГРЗ в целом близка к критериям орфанного заболевания.
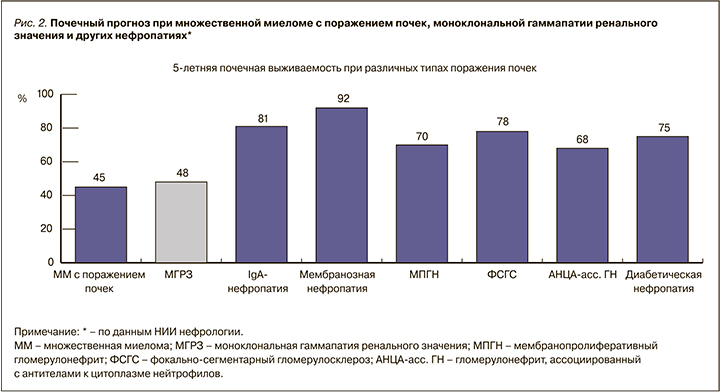
МГРЗ нельзя считать доброкачественным состоянием, поскольку клон за счет эффектов парапротеина неуклонно ведет к прогрессии дисфункции почек и в итоге к гибели органа (терминальной стадии хронической болезни почек). Медико-экономическое значение хронической болезни почек (ХБП) определяется резким увеличением рисков нефатальных и фатальных событий, инвалидизацией больных, а также значительными расходами на проведение диализа [24–28]. Почечный прогноз при МГРЗ сопоставим с таковым при ММ с поражением почек и значительно хуже, чем при других вариантах нефропатий (рис. 2). Кроме того, при наличии МГРЗ риск прогрессии клона в злокачественный выше, а значит, хуже прогноз в отношении продолжительности жизни. Так, риск трансформации клона в злокачественную форму при МГРЗ в 3,3 раза выше и в течение первого года составляет 10% [11], что сопоставимо с частотой прогрессирования тлеющей ММ в симптоматическую [29].
ОБОСНОВАНИЕ НЕОБХОДИМОСТИ ВВЕДЕНИЯ НОЗОЛОГИЧЕСКОЙ ГРУППЫ МОНОКЛОНАЛЬНОЙ ГАММАПАТИИ РЕНАЛЬНОГО ЗНАЧЕНИЯ
Неблагоприятное прогностическое значение МГРЗ делает очевидным необходимость лечения такого «неопасного» с формальной точки зрения классической онкогематологии клонального процесса [2]. Подобный «прецедент» хорошо известен в онкогематологии – это системный AL-амилоидоз, тяжелое заболевание с минимальным клоном плазмоцитов в костном мозге, но крайне неблагоприятным в отсутствие лечения прогнозом, которое длительное время являлось предметом неразрешимых противоречий между гематологами и нефрологами. Достаточно давно разработаны и применяются, в том числе и в России, эффективные схемы химиотерапии AL-амилоидоза, направленные на элиминацию опухолевого клона [30–33]. Такая же лечебная стратегия должна быть использована и при неамилоидных формах поражения почек, ассоциированных с МГ [12, 13, 34–37].
Преодоление стереотипа лечения только злокачественного клона в международной практике происходило поэтапно по мере накопления данных в отношении патофизиологии МГ, что отражено в ряде работ первого десятилетия XXI в. [7, 20, 38–40]. Наиболее значимой вехой стала известная работа Leung N. et al., опубликованная в 2012 г. в журнале Blood от имени Международной группы по изучению почек и моноклональной гаммапатии (International Kidney and Monoclonal Gammopathy Research Group) [1]. Название этой статьи «Monoclonal gammopathy of renal significance: when MGUS is no longer undetermined or insignificant» («Моноклональная гаммапатия ренального значения: когда моноклональная гаммапатия неопределенного значения становится определенной и значимой») раскрывает существенные перемены в понимании ведущими гематологами и нефрологами мира проблемы поражения почек при МГ и осознании необходимости лечения подобного состояния. Впоследствии опубликованы многочисленные статьи по этой проблематике [41–44], интерес к которой со стороны, в первую очередь нефрологов, обусловлен возможностью эффективного этиотропного лечения, минимизации/устранения эффектов нефротоксичного М-протеина, а в результате улучшения общего и почечного прогноза.
МЕХАНИЗМЫ И СТРУКТУРА ПОРАЖЕНИЯ ПОЧЕК ПРИ МОНОКЛОНАЛЬНОЙ ГАММАПАТИИ
Механизмы воздействия парапротеина на почечную ткань и структуры организма крайне разно-образны и пока окончательно не выяснены [21, 45]. В силу особенностей строения и соответствующим образом измененных физико-химических свойств самой молекулы парапротеина, а также действия местных факторов аномальные ИГ и/или легкие цепи (ЛЦ) способны:
- оказывать токсическое влияние на клетки;
- действовать наподобие антител по отношению к различным молекулам;
- активировать иммунную систему, в частности систему комплемента;
- взаимодействовать с мезангиоцитами и другими клетками нефрона и аккумулироваться в виде депозитов различной структуры, например в виде амилоидных фибрилл.
При МГРЗ патологическое действие моноклонального ИГ может быть реализовано на уровне любого компартмента нефрона: клубочка, канальцев, интерстиция, сосудов [46]. Отсюда происходит и разнообразие клинических проявлений МГРЗ, которое может заключаться в любом синдроме поражения почечной паренхимы или их комбинации (рис. 3).
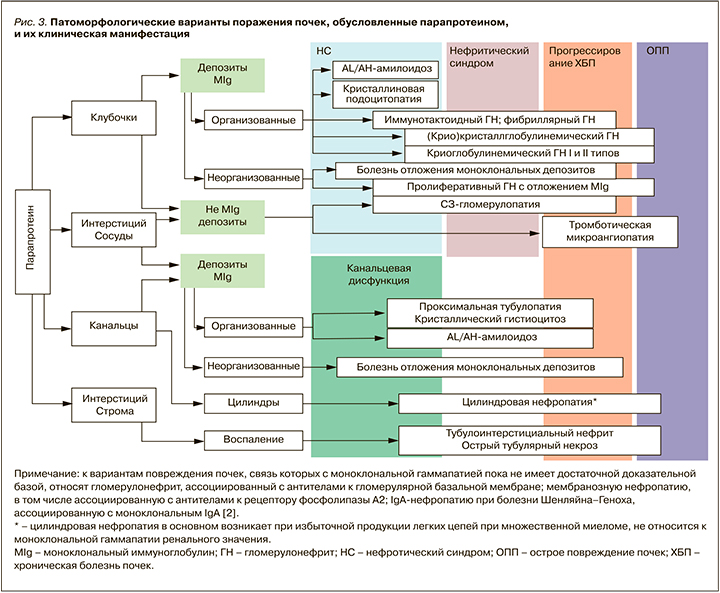
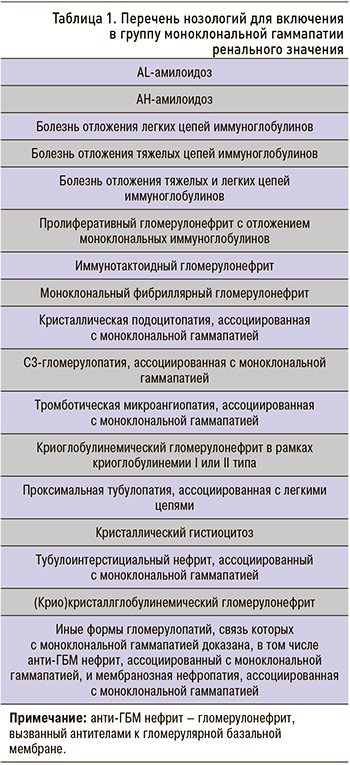
В связи с тем что клон плазматической клетки или В-лимфоцита «небольшой» и, как правило, не вызывает явных симптомов, ассоциированных с опухолью, пациенты с МГРЗ, имеющие преимущественно почечные проявления, первично оказываются пациентами врача-терапевта и нефролога, обращаясь по поводу развития «почечных» симптомов (АГ, отеков, гематурии, протеинурии, дисфункции почек и др.). Нозологии, которые входят в группу МГРЗ, представлены в таблице 1.
ДИАГНОСТИКА МОНОКЛОНАЛЬНОЙ ГАММАПАТИИ РЕНАЛЬНОГО ЗНАЧЕНИЯ
МГРЗ – проблема, находящаяся на стыке двух специальностей – гематологии и нефрологии, для решения которой требуется мультидисциплинарный подход.
Для установления диагноза МГРЗ необходимо:
- определить наличие клона B-клеточной линии дифференцировки;
- установить специфичность поражения почек, обусловленного воздействием продуцируемого клоном моноклонального белка.
В связи с этим диагностика включает гематологические и нефрологические методы исследования [2, 46]. Принимая во внимание существенное разнообразие вариантов поражения почек при МГРЗ, очевидно, что ключевым этапом диагностики этого состояния выступает морфологическое исследование почечной ткани [47]. Результат гистологического исследования и клинико-морфологический анализ раскрывают особенности МГРЗ в каждом конкретном случае, а также несут крайне важную для нефролога информацию в отношении почечного прогноза.
Морфологическая диагностика моноклональной гаммапатии ренального значения
С целью полноценной диагностики МГРЗ морфологическое исследование почечной ткани должно включать:
- светооптическое исследование с применением окрасок: гематоксилин/эозин, ШИК-реакция, серебрение по Джонсу, Конго-рот, трихромальная окраска по Массону, окраска на эластические волокна;
- иммуноморфологическое исследование: иммунофлюоресценция (ИФ) или иммуногистохимия (ИГХ) для выявления в почечной паренхиме депозитов молекул моноклонального ИГ [панель антител к IgA, IgM, IgG (типирование IgG), IgD, kappa, lambda, С3, С1q];
- ультраструктурное исследование позволяет оценить степень повреждения структур почки на субмикроскопическом уровне и характер депозитов, образованных моноклональным белком (организованные, неорганизованные). Последнее является ключевым в дифференциальной диагностике таких форм МГРЗ, как иммунотактоидный, фибриллярный, криоглобулинемический гломерулонефриты и др.
На завершающих этапах морфологической дифференциальной диагностики МГРЗ в рамках omics-технологий, и в частности протеомики, в некоторых зарубежных центрах применяют лазерную микродиссекцию с последующими разделением белковых компонентов почечной ткани методом капиллярного электрофореза и идентификацией молекулярного состава с помощью MALDI-TOF (матрично-активированная лазерная десорбция/ионизация с время-пролетным анализом и визуализирующей масс-спектрометрией) [47–49].
Вышеописанные подходы к морфологической диагностике должны быть осуществлены исключительно в высокоспециализированной и хорошо оснащенной морфологической лаборатории, где все необходимые методики будут применены и оценены опытным нефропатологом.
Гематологическая диагностика моноклональной гаммапатии ренального значения
Цель гематологического обследования – выявление парапротеина и клона B-клеточной линии дифференцировки. Объем обследования соответствует таковому при ММ, В-лимфоме или макроглобулинемии Вальденстрема и подробно описан в соответствующих рекомендациях [50–55].
Для успешной верификации «небольшого» клона важно использование высокочувствительных методик, позволяющих обнаруживать даже небольшой клон и малое количество парапротеина: иммунофенотипирование костного мозга, генетические исследования, иммунофиксация сыворотки крови и мочи, определение в сыворотке свободных ЛЦ методом Freelite или иными методами, сопоставимость которых с Freelite доказана. Эти методики служат основой не только для первичной гематологической диагностики, но и оценки эффективности лечения и прогрессии заболевания.
ЛЕЧЕНИЕ МОНОКЛОНАЛЬНОЙ ГАММАПАТИИ РЕНАЛЬНОГО ЗНАЧЕНИЯ
На мультидисциплинарном подходе основано и лечение МГРЗ, которое должно быть клон-ориентированным и включать известные препараты и схемы химиотерапии, применяемые при ММ, В-лимфоме, ХЛЛ и макроглобулинемии Вальденстрема [34, 36, 50–57]. Кратко современные подходы к этиотропной терапии МГРЗ отражены в таблице 2.
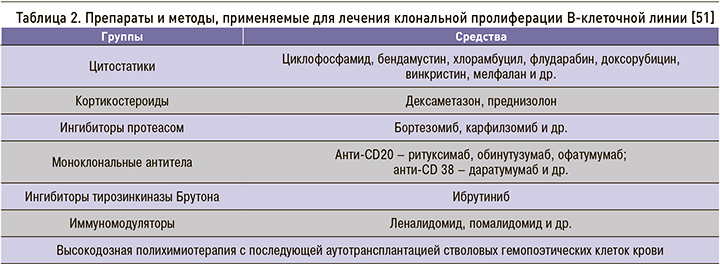
Цель лечения – снижение продукции патогенных ЛЦ/ИГ, уменьшение отложения парапротеина в органах и тканях, предупреждение дальнейшего прогрессирования их дисфункции, а также предотвращение трансформации клона в злокачественную форму [11]. Помимо химиотерапии, в качестве опции лечения МГРЗ должна рассматриваться высокодозная полихимиотерапия с поддержкой аутотрансплантацией гемопоэтических стволовых клеток (аутоТГСК).
В комплексное нефрологическое сопровождение терапии МГРЗ входят разнообразные мероприятия. Они заключаются в коррекции доз препаратов с учетом их потенциальной нефротоксичности, профилактике и лечении острого повреждения почек, воздействии на специфические патогенетические механизмы повреждения почек (лечение тромботической микроангиопатии, иммунокомплексного повреждения органа, увеличение клиренса депозитов ИГ), оценке функций почек в динамике и коррекции их нарушений, оценке почечного ответа, а также применении методов экстракорпоральной элиминации ЛЦ. Также важна подготовка потенциальных реципиентов аллотрансплантата почки и включение таких больных в лист ожидания. С учетом высокой частоты возврата МГРЗ в трансплантат почки первым этапом необходимо проводить клон-ориентированную терапию и консолидацию гематологического ответа с помощью аутоТГСК [58].
Консенсус не преследует цели подробно осветить методы лечения МГРЗ. Вопросы терапии обсуждаемой нозологии будут подробно описаны в виде клинических рекомендаций в дальнейшем.
Проблемы лечения моноклональной гаммапатии ренального значения в России
В настоящее время в отечественной практической медицине МГРЗ не рассматривается как нозология, и соответствующих пациентов формально относят к группе МГНЗ или случаям В-клеточной пролиферации без критериев для начала терапии. В результате традиционных, но сейчас устаревших представлений о том, что в случаях МГ лечению должен подвергаться исключительно злокачественный опухолевый клон, эффективной клон-ориентированной химиотерапией (бортезомиб, леналидомид, ритуксимаб и др.) обеспечены только пациенты со злокачественными формами МГ –
ММ, лимфомами, ХЛЛ. В то же время пациенты с МГРЗ, включая AL-амилоидоз, не соответствующей формальным критериям злокачественности, не входят в программы обеспечения необходимыми лекарствами (Федеральный закон от 03.08.2018 № 299 «О внесении изменений в Федеральный закон „Об основах охраны здоровья граждан в Российской Федерации”») и остаются без возможности получать адекватную характеру и прогнозу болезни терапию. Безусловно, в отношении МГРЗ подобный подход неприемлем.
Недоступность лечения, обусловленная в первую очередь тем, что диагноз «в списках не значится», а также непониманием истинной природы болезни и недооценкой ее клинико-прогностического значения, губительна для больных [59]. Пациенты с этой патологией должны быть обеспечены необходимыми препаратами и возможностью проведения лечения в рамках финансирования по каналу высоких технологий, включая аутоТГСК.
Предпосылки для создания онконефрологического центра
Патология почек, ассоциированная с МГ, стоит на стыке двух специальностей – гематологии и нефрологии. Понимание крайней актуальности этой проблемы в мире привела к возникновению новой узкоспециализированной области – онконефрологии [60, 61]. Очевидно, что диагностика МГРЗ, наблюдение и лечение таких пациентов должно осуществляться в специализированном онконефрологическом центре.
Опыт создания и работы таких центров реализован за рубежом [62]. Создание онконефрологического центра в России возможно на базе многопрофильного стационара, имеющего в своем составе отделения гематологии, нефрологии, заместительной почечной терапии, трансплантации стволовых клеток и почки. Другим определяющим моментом служит наличие соответствующих диагностических ресурсов, включая иммуноморфологическую лабораторию, обладающую необходимыми для полноценной диагностики МГРЗ методиками.
ЗАКЛЮЧЕНИЕ КОНСЕНСУСА ГЕМАТОЛОГОВ И НЕФРОЛОГОВ ПО МОНОКЛОНАЛЬНОЙ ГАММАПАТИИ РЕНАЛЬНОГО ЗНАЧЕНИЯ
МГРЗ – это не самостоятельное заболевание почек, не «хронический гломерулонефрит», а состояние, при котором поражение почек вторично по отношению к клональной В-клеточной пролиферации. Иными словами, МГРЗ – это пред-опухолевое заболевание в сочетании с ХБП, которое требует незамедлительного начала лечения. Последнее, однако, невозможно для пациентов в России в связи с отсутствием диагноза МГРЗ в перечне нозологий, а значит, и отсутствием помощи при этой патологии.
В рамках данного консенсуса нефрологи и гематологи ведущих клиник страны пришли к общему мнению в отношении МГРЗ и выносят на рассмотрение профессионального сообщества и органов управления здравоохранением РФ ряд предложений, реализация которых позволит существенно улучшить ситуацию в диагностике и лечении этой категории больных.
Заключительные положения консенсуса
- МГРЗ представляет собой группу заболеваний, при которых повреждение почек происходит в результате патологического действия моноклонального белка (иммуноглобулина или его части), продуцируемого опухолевым клоном В-клеточной линии дифференцировки. При этом критериев, позволяющих начать специфическую терапию лимфатической опухоли, нет.
- МГРЗ – гетерогенная группа заболеваний, при которой результат воздействия моноклонального белка на почечную ткань может быть различным, однако неизбежно приводит к прогрессирующей дисфункции почек, вплоть до полной утраты функции органа, и к уменьшению продолжительности жизни.
- Принимая во внимание крайне неблагоприятный прогноз в отношении функции почек и жизни, МГРЗ должна быть включена в реестр «жизнеугрожающих и хронических прогрессирующих (орфанных) заболеваний, приводящих к сокращению продолжительности жизни пациентов или их инвалидности», в виде общего названия, объединяющего ряд отдельных нозологий, включая AL-амилоидоз, болезнь отложения моноклональных депозитов и др. (см. табл. 1).
- При МГРЗ диагностика клональной пролиферации требует выполнения иммунофенотипических и молекулярных исследований, направленных на выявление «небольшого» клона, включая выявление парапротеина в крови и моче с использованием иммунофиксации и определения свободных легких цепей методом Freelite или иными методами, сопоставимость которых с Freelite доказана. Данные методики должны быть доступны в первую очередь в специализированных онкогематологических центрах, а также в других крупных стационарах России, так как являются основой не только для первичной гематологической диагностики, но и для оценки эффективности лечения и прогрессии заболевания.
- Наряду с выявлением опухолевого клона, диагностика МГРЗ требует обязательного проведения биопсии почки с морфологическими исследованиями, позволяющими подтвердить специфическое поражение органа. Морфологическое исследование нефробиоптата должно включать светооптический, иммуноморфологический, ультраструктурный методы. Основным признаком МГРЗ являются организованные и/или неорганизованные депозиты парапротеина моноклональной природы в компартментах почки. Тип моноклонального парапротеина, выявленного в сыворотке крови или в моче, должен совпадать с типом моноклонального белка, определенного морфологически и вызвавшего поражение почек.
- Диагноз МГРЗ должен быть обсужден консилиумом в составе гематолога, нефролога и почечного патолога и быть основан на констатации патогенетической связи поражения почек и имеющейся моноклональной пролиферации – клона В-лимфоцита/плазматической клетки и/или выявленного в сыворотке/крови парапротеина.
- Любой вариант МГРЗ требует начала клон-ориентированного лечения, финальной целью которого служит сохранение функции почек и предупреждение прогрессирования клона в сторону опухолевого процесса. Характер химио-терапии зависит от типа клональной пролиферации. Лечение должно быть назначено и проведено на мультидисциплинарной основе в соответствии с типом клона/парапротеина и особенностями повреждения почек гематологом и нефрологом, имеющими подобный опыт.
- Группу онкогематологических болезней, объединенных термином МГРЗ, необходимо включить в перечень патологий, требующих назначения дорогостоящих химиотерапевтических препаратов. Пациенты должны получать лечение в рамках канала финансирования «высокие технологии».
- Консолидация гематологического ответа может быть достигнута с помощью проведения высокодозной полихимиотерапии с последующей аутоТГСК, в связи с чем целесообразно расширить показания для аутоТГСК и включить в стандарты оказания данного вида помощи, помимо AL-амилоидоза, и другие типы МГРЗ.
- С целью успешной диагностики, своевременного эффективного лечения МГРЗ и долгосрочного наблюдения за пациентами с этой патологией целесообразно открытие специализированных отделений/центров онконефрологии в учреждениях, располагающих соответствующими ресурсами для диагностики и лечения и квалифицированными врачебными кадрами, имеющими соответствующий опыт в онкогематологии и нефрологии.
- На основании положений консенсуса целесо-образно создание национальных рекомендаций по этой клинической проблеме.