Новая коронавирусная инфекция (COVID-19), вызванная вирусом SARS-CoV-2, представляет собой высококонтагиозное респираторное заболевание, которое может иметь достаточно широкий спектр клинических проявлений от бессимптомного течения до тяжелой дыхательной недостаточности, сепсиса, септического шока и полиорганной недостаточности. Тем не менее в большинстве случаев заболевание проявляется лихорадкой, сухим кашлем, одышкой и общим упадком сил [1, 2]. Часто инфекция осложняется двусторонним полисегментарным интерстициальным поражением легочной ткани.
Длительность персистирования симптомов COVID-19 неодинакова, в связи с чем актуальна оценка клинической картины и лабораторных показателей в ранние сроки болезни. Подавляющее большинство лиц с легким течением инфекции ведется амбулаторно без возможности детального контроля течения заболевания лечащим врачом. Поэтому наиболее важным представляется изучение динамики симптомов больных COVID-19 средней степени тяжести.
Целью настоящей работы стала оценка динамики клинических симптомов и лабораторных показателей у пациентов с COVID-19 за первую неделю госпитализации.
МАТЕРИАЛ И МЕТОДЫ
В проспективное когортное исследование были включены 38 пациентов (21 женщина и 17 мужчин) с COVID-19 средней тяжести, находившихся на стационарном лечении в «Центральной городской клинической больнице № 6» г. Екатеринбурга. Набор материала проводился в период с 20.06 по 14.08.2020.
Критерии включения в исследование: подтвержденное методом полимеразной цепной реакции инфицирование SARS-CoV-2, среднетяжелое течение COVID-19 и выявление минимального или среднего объема поражения легких по данным компьютерной томографии (не более 50%), подписанное информированное добровольное согласие на участие. Среднетяжелое течение определялось согласно критериям, указанным в актуальных на момент проведения исследования временных методических рекомендациях по профилактике, диагностике и лечению новой коронавирусной инфекции (COVID-19) версии 7 от 03.06.2020 [3].
Состояние пациента в процессе динамического наблюдения регистрировалось с помощью специально разработанной клинической карты, включавшей оценку следующих симптомов: кашля, одышки, ощущения заложенности в грудной клетке, боли в горле, заложенности носа, обоняния, ощущения вкуса, конъюнктивита, слабости, мышечных болей, головной боли, тошноты, рвоты, нарушения стула, кожной сыпи. В карту вносились данные антропометрии, измерения температуры тела, артериального давления (АД), частоты сердечных сокращений (ЧСС), частоты дыхательных движений (ЧДД), уровня оксигенации крови. Было проведено анкетирование с помощью европейского опросника качества жизни EQ-5D-5L, визуально-аналоговой шкалы состояния здоровья (ВАШ), госпитальной шкалы тревоги и депрессии HADS, оценены параметры клинического анализа крови.
Обследование пациентов выполнялось на момент госпитализации и спустя 7 дней на фоне проводимого лечения (антибактериальная терапия, респираторная поддержка, в ряде случаев противовирусная терапия), назначаемого согласно временным методическим рекомендациям по профилактике, диагностике и лечению новой коронавирусной инфекции (COVID-19) версии 7 от 03.06.2020 [3].
Статистическая обработка проводилась с помощью программного продукта Statistica 13.0. (лицензия JPZ904I805602ARCN25ACD-6). Распределение данных оценивалось с помощью критериев Шапиро–Уилка и Колмогорова–Смирнова в модификации Лиллиефорса. Учитывая, что распределение не подчинялось нормальному закону, данные представлены как медианы и квартили (25÷75%). Качественные зависимые показатели сравнивались с помощью критерия χ2 МакНемара, а количественные – Вилкоксона. Различия считали статистически значимыми при значениях р <0,050.
Проведение исследования было одобрено локальным этическим комитетом муниципального бюджетного учреждения «Центральная городская клиническая больница № 6» г. Екатеринбурга на заседании № 2 от 08.06.2020.
РЕЗУЛЬТАТЫ
В пилотное исследование были включены 38 человек, медиана возраста составила 55 (45÷64) лет, индекс массы тела – 27,8 (25,9÷31,2) кг/м2.
С момента появления первых признаков заболевания до госпитализации проходило в среднем 7 (5÷10) дней. У всех пациентов с помощью компьютерной томографии (КТ) была выявлена двусторонняя пневмония, объем поражения легочной ткани при этом не превышал 50%. Диагноз COVID-19 был подтвержден этиологически путем обнаружения рибонуклеиновой кислоты SARS-CoV-2 в отделяемом носоглотки методом полимеразной цепной реакции (ПЦР).
В таблице 1 приведена динамика клинических симптомов COVID-19 за 7 дней стационарного наблюдения.

Самыми распространенными симптомами, обнаруживаемыми в момент госпитализации, были общая слабость, кашель, головная боль и диарея. Несколько реже выявлялись одышка, аносмия, чувство заложенности в грудной клетке, миалгии, дисгевзия, тошнота и заложенность в носу. Наиболее редко встречались конъюнктивит и боль в горле. На момент госпитализации ни один больной не имел сыпи.
В течение недели наблюдения практически у всех больных регрессировали расстройства обоняния и вкуса, мышечные боли и конъюнктивит. Слабость, головная боль, одышка и гастроинтестинальные симптомы (тошнота и диарея) исчезли примерно у половины больных, их испытывавших. Лишь у четверти больных прошел кашель. Катаральные симптомы (боль в горле, заложенность в носу) сохранялись без существенной динамики. Отметим, что на 7-й день наблюдения у двух больных появилась экзантемная сыпь.
Параметры качества жизни обследованных представлены в таблице 2. Анкетирование выявило улучшение общего самочувствия за первую неделю госпитализации в среднем на 20 баллов по ВАШ. В течение 7 дней уровень боли/дискомфорта у больных снизился на 1 балл по шкале EQ-5D-5L.
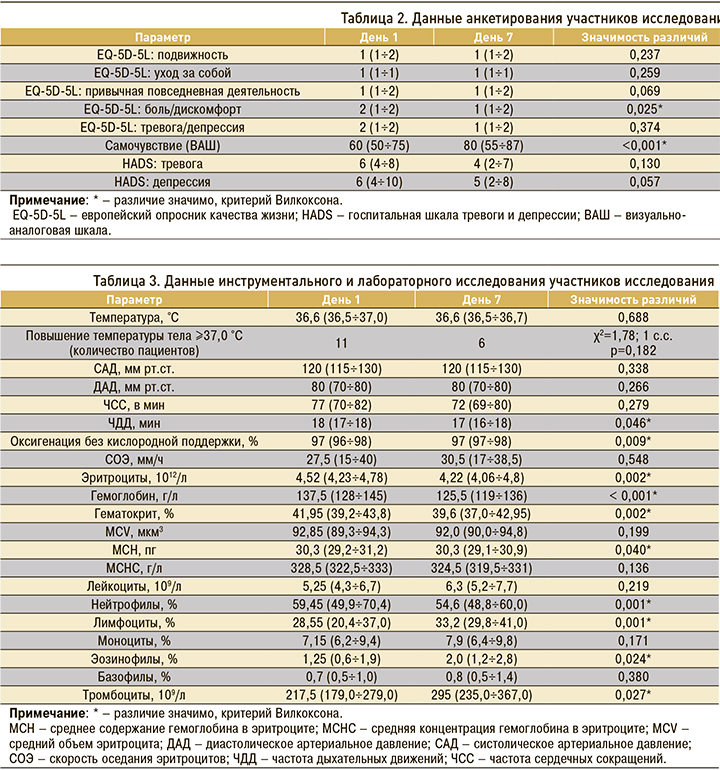
В таблице 3 суммированы данные инструментального и лабораторного исследования.
При сборе анамнеза 23 пациента отметили повышение температуры тела в первые дни болезни до фебрильных значений (≥38,0 °С), 11 – до субфебрильных (37,0–37,9 °С), у 4 обследованных температура тела не поднималась. В момент госпитализации температура тела была повышена у 11 пациентов, из них у 9 – до субфебрильных значений, у 2 – до фебрильных. Снижение температуры тела у больных от начала заболевания к моменту госпитализации было статистически значимо (χ2=17,93; 1 с.с., р <0,001). Тем не менее у двух пациентов наблюдалось отсроченное развитие лихорадки ближе к моменту госпитализации. На 7-й день наблюдения у 4 человек субфебрилитет сохранился, у 2 появился впервые. Статистической значимости динамика температуры тела пациентов в течение 7 дней стационарного наблюдения не достигла (см. табл. 3).
В течение 7 дней АД, ЧСС существенно не изменялись. Наблюдалось уменьшение ЧДД и повышение уровня оксигенации без кислородной поддержки. В то же время за неделю пребывания в стационаре у пациентов снизились уровни эритроцитов, гемоглобина, гематокрита, среднего содержания гемоглобина в эритроците. Также наблюдалась тенденция к повышению уровня тромбоцитов и снижению уровня нейтрофилов при увеличении количества лимфоцитов и эозинофилов.
ОБСУЖДЕНИЕ
Малый объем выборки пилотного исследования определялся действовавшим в период включения пациентов алгоритмом маршрутизации, не у всех больных инфицирование SARS-CoV-2 было подтверждено к моменту госпитализации.
Представленная группа была сформирована из лиц с умеренно тяжелым течением COVID-19, имевших дополнительные эпидемиологические и социальные показания для госпитализации в соответствии с действовавшими в период набора материала рекомендациями [3]. В обследованной группе основным критерием диагноза средней степени тяжести служил объем поражения легких, оцененный по компьютерной томографии органов грудной клетки.
Повышенная температура тела – первый симптом, возникающий по окончании инкубационного периода. При неосложненном течении заболевания ее длительность не превышает 2–3 дней [3]. Только четверть обследованных имели субфебрилитет при поступлении, однако большинство отмечало повышение температуры тела в первые дни болезни, что хорошо согласуется с клиническим описанием болезни в рекомендациях [3]. Нормальную температуру тела значительной доли обследованных можно объяснить тем, что они обращались за медицинской помощью при появлении других клинических симптомов через 5–7 дней от дебюта симптоматики.
Другие признаки системного воспалительного ответа (слабость, головная и мышечные боли) также отмечались в первые дни наблюдения, но в отличие от субфебрилитета они сохранялись дольше и редуцировались постепенно.
После окончания инкубационного периода также типичным было возникновение незначительного покашливания и першения в горле, трансформировавшихся в сухой кашель в течение нескольких дней после нормализации температуры тела. В исследуемой группе наблюдалась медленная стабильная регрессия кашля.
Заложенность в носу как следствие отека слизистой оболочки полости носа встречалась только у четверти больных, однако сохранялась на протяжении всего наблюдения.
Частичная или полная потеря обоняния и вкуса относятся к наиболее кратковременным симптомам легкого течения инфекции, что отражено и в нашем исследовании. Имеются данные о том, что расстройства обоняния и вкуса могут предшествовать остальным симптомам новой коронавирусной инфекции, являясь сильными предикторами инфицирования SARS-CoV-2 [4]. Однако на момент госпитализации их обычно удается зафиксировать, так как данные клинические проявления являются поводом для беспокойства больных и в совокупности с остальной симптоматикой становятся причиной вызова бригады скорой медицинской помощи. Аносмия и дисгевзия свидетельствуют о том, что вирус также способен проникать в центральную нервную систему [5]. Дополнительным фактором потери обоняния и извращения вкуса является заложенность в носу, персистировавшая у ряда больных на протяжении всего периода наблюдения.
Одним из самых опасных симптомов является одышка. Она носит нарастающий характер по причине постепенного ухудшения работы дыхательной системы, поэтому может потребовать неинвазивной кислородной поддержки и перехода к инвазивной оксигенации при искусственной вентиляции легких. Одышка выступает частым симптомом COVID-19, но в случае среднетяжелого течения болезни при применении прон-позиции и соответствующей симптоматической терапии может регрессировать в течение недели с момента ее появления [6] без использования аппарата искусственной вентиляции легких. Помимо этого, стоит учитывать, что одышка может быть симптомом сопутствующей патологии полиморбидного пациента. Поэтому необходим тщательный опрос и обследование больного, независимо от наличия основного диагноза COVID-19.
Чувство тяжести и заложенности в грудной клетке – субъективное ощущение, как правило, отражающее невозможность пациента совершить дыхательный акт полной грудью, что связано с наличием одышки и мышечной боли. При стихании этих клинических симптомов отмечалась соответствующая положительная динамика и в отношении заложенности в грудной клетке, однако она не достигла статистической значимости.
Уменьшение ЧДД и возрастание уровня оксигенации без кислородной поддержки обусловлено общим улучшением состояния пациента, подтверждаемым с помощью опросника EQ-5D-5L и ВАШ.
Появление желудочно-кишечных симптомов можно связать с тем, что SARS-CoV-2 атакует рецепторы ангиотензинпревращающего фермента (АПФ) и мембраносвязанной сериновой протеазы TMPRSS2, располагающихся не только в легких и эндотелии сосудов, но и верхних отделах пищевода, печени, тонкого и толстого кишечника [7]. Среди желудочно-кишечных расстройств, наряду с тошнотой и диареей, часто выявляется рвота [8]. Однако данный симптом отсутствовал у всей группы больных, что можно объяснить малым объемом выборки.
Кратковременное появление сыпи на 7-й день у двоих пациентов соответствует данным о достаточно невысокой частоте высыпаний при новой коронавирусной инфекции, ее патогенез не ясен [9]. Также имеются данные о том, что дерматологические проявления манифестируют спустя 13 дней после появления респираторных симптомов [10], вследствие чего зафиксировать их не представляется возможным в условиях поставленного времени наблюдения.
Снижение уровней эритроцитов, гемоглобина, гематокрита, среднего содержания гемоглобина в эритроците может быть объяснено способностью синтезируемых под действием SARS-CoV-2 специфических протеинов orf1ab, ORF10 и ORF3a вытеснять атом двухвалентного железа из 1-бета-цепи гемоглобина [11]. Возникающая вследствие этого процесса гиперферритинемия индуцирует дополнительные процессы перекисного окисления липидов, определяющие дальнейшее прогрессирующее снижение гемоглобина и нарушение метаболизма железа, которое, в свою очередь, может привести к развитию сидеробластной анемии и гемосидерозу [12].
Выявленное повышение уровня тромбоцитов может являться следствием связывания вируса с рецепторами АПФ, присутствующими на эндотелии сосудов, в результате чего возникает эндотелиальная дисфункция и индукция агрегации тромбоцитов. Количество тромбоцитов служит ключевым маркером определения прогноза пациентов с COVID-19 [13, 14].
Снижение количества нейтрофилов может быть показателем длительного воспалительного процесса. Лимфопения и эозинопения относятся к неблагоприятным прогностическим факторам [3], однако в нашем исследовании выявлялось небольшое увеличение количества лимфоцитов и эозинофилов.
Необходимо отметить, что все лабораторные показатели при их снижении или повышении тем не менее оставались в пределах нормальных значений; это свидетельствует об адекватности получаемой терапии, анализ структуры, эффективности, переносимости и безопасности которой будет представлен в следующих публикациях.
ЗАКЛЮЧЕНИЕ
Слабость, головная боль, мышечные боли, одышка, кашель, снижение обоняния и вкуса, тошнота, диарея постепенно регрессировали у пациентов с COVID-19 в течение первой недели наблюдения, тогда как боль в горле и заложенность в носу персистировали. К моменту госпитализации температура у большинства больных находилась в нормальном диапазоне, и во время разгара инфекции гипертермия отсутствовала. Отмечена негативная тенденция к снижению уровня эритроцитов, гемоглобина, гематокрита, среднего содержания гемоглобина в эритроците, уровня нейтрофилов, а также к повышению уровня тромбоцитов.
Вышеперечисленные изменения можно связать как с особенностями течения COVID-19, так и эффективностью проводимой терапии.


