АКТУАЛЬНОСТЬ
С момента первой вспышки в конце 2019 г. новая коронавирусная инфекция COVID-19 за последние 3 года распространилась более чем в 235 странах, и по состоянию на 01.02.2022 в мире было зарегистрировано 382 057 476 случаев заражения SARS-CoV-2, из которых 5 692 117 закончились летальными исходами [1, 2]. Помимо высокой смертности, связанной с пандемией, все большее внимание исследователей привлекают отсроченные или поздние последствия COVID-19 у выживших пациентов. Неслучайно в оборот был введен новый термин – «постковидный синдром» (ПКС, long-COVID, post-COVID-19 syndrome, post-acute COVID-19 syndrome), описывающий признаки и симптомы, которые развиваются во время или после заболевания COVID-19, продолжаются более 12 нед (в 2,3% случаев – дольше), возникают волнообразно или на постоянной основе и не имеют альтернативного объяснения (диагноза). ПКС получил официальный статус болезни и появился в новой редакции МКБ-10, где обозначен как «post-COVID-19 condition» под кодом U09.9.
Согласно имеющимся в настоящее время данным, COVID-19 может поражать в организме каждый орган, приводя к острым повреждениям и долгосрочным последствиям. По мере накопления данных клинических и лабораторных исследований стало очевидным, что новая коронавирусная инфекция способна индуцировать как прямое, так и опосредованное воздействие на нервную систему. Независимо от прямого или опосредованного воздействия вируса, повреждение центральной и периферической нервной системы вследствие COVID-19 может стать необратимым [1, 2].
В связи с этим целью нашего исследования стало изучение клинико-эпидемиологической характеристики неврологических вариантов ПКС на примере данных неврологической клиники ГБУЗ НО «Государственная Новосибирская областная клиническая больница» (ГНОКБ) за период с июля 2020 года по февраль 2022 г.
Следуя этой цели, мы поставили перед собой следующие задачи.
1. Изучение литературных данных о неврологических вариантах ПКС в зарубежной и отечественной практике.
2. Проведение клинико-эпидемиологического ретроспективного анализа историй болезни пациентов с различными неврологическими вариантами постковидного синдрома в неврологической клинике ГНОКБ.
3. Выявление клинических особенностей типичных неврологических нозологий, спровоцированных новой коронавирусной инфекцией на основании анализа историй болезни пациентов.
МАТЕРИАЛ И МЕТОДЫ
Нами был выполнен комплексный поиск литературы в системах SCOPUS, Embase, Google Scholar и LitCOVID28 (включая все статьи по теме COVID- 19, опубликованные в базах данных PubMed и Medline) до февраля 2022 г. В качестве поисковых запросов использовалось сочетание следующих терминов: long-haul COVID-19, post-COVID, post-acute COVID syndrome (PACS), «post-acute sequelae of SARS-CoV-2 (PASC).
Осуществлен ретроспективный анализ в общей сложности 1500 историй болезни пациентов: среди них было выявлено 30 человек с наличием в анамнезе лабораторно подтвержденного COVID- 19 и различными манифестирующими неврологическими заболеваниями, которые поступили в ГНОКБ с за период с июля 2020 по февраль 2022 г.
РЕЗУЛЬТАТЫ И ОБСУЖДЕНИЕ
Существует множество патогенетических гипотез ПКС, однако единой теории на этот счет в настоящее время нет. Все гипотезы не противоречат друг другу, и рассматриваемые в них факторы могут вносить свой вклад в формирование ПКС. Несомненно, что его патогенез связан с базовыми механизмами развития и течения COVID-19.
Первоначально считалось, что SARS-CoV-2 не способен преодолевать гематоэнцефалический барьер (ГЭБ), однако последующие исследования заставили пересмотреть эту точку зрения [1]. Во-первых, рецептор связывания белка SARS-CoV-2 spike (S), ангиотензинпревращающий фермент 2 (АПФ 2), в высокой степени экспрессируется в черной субстанции, сосудистых сплетениях, желудочках, средней височной извилине, задней части поясной извилины и обонятельной луковице. Белок также экспрессируется в цитоплазме как нейрональных, так и глиальных клеток головного мозга человека, в симпатических путях ствола мозга и в моторной коре; более того, транскриптомный анализ показал, что АПФ 2 в высокой степени экспрессируется как в возбуждающих, так и в тормозных нейронах, астроцитах, олигодендроцитах и эндотелиальных клетках [2]. Во-вторых, белок S может вызывать воспалительную реакцию эндотелиальных клеток в микроциркуляторном русле, которая изменяет функцию ГЭБ [2, 3]. Таким образом, SARS-CoV-2 может как непосредственно, так и опосредованно повреждать ГЭБ и проникать в головной мозг, способствуя появлению неврологических симптомов. Наряду с этим SARS-CoV-2 способен проникать в головной мозг посредством транссинаптического переноса через каналы зрительного и обонятельного нервов и эндотелиальных клеток сосудов. Также выявлены альтернативные гипотетические пути попадания SARS-CoV-2 в центральную нервную систему (ЦНС) – через дыхательную систему (эпителий путей к капиллярам или альвеолярные клетки пневмоцитов к капиллярам), что приводит к проникновению вируса в легочную/общую циркуляцию, и через желудочно-кишечный тракт. В последнем случае энтероцитарная и параэнтероцитарная инфекция обеспечивает доступ вируса к подслизистой капиллярной сети системы воротной вены с инфицированием воспалительных клеток в подслизистой соединительной ткани; в результате инфекционного поражения нейронов подслизистого и/или мышечно-кишечного сплетения создаются условия для прямого попадания вирионов в ЦНС по пути нейрон–нейрон [2].
Существенную роль в повреждении нервной системы играет массивный синдром системного воспаления, вызываемый SARS-CoV-2. Системное увеличение содержания медиаторов воспаления, таких как интерлейкин 6 (ИЛ-6), ИЛ-12, ИЛ-15 и фактор некроза опухоли-альфа (ФНО-α), называемое «цитокиновым штормом», может объяснить влияние вируса на ЦНС: высвобождение большого количества провоспалительных цитокинов повышает проницаемость сосудов в ЦНС и вызывает нарушение свертываемости крови с образованием микротромбов, облегчая проникновение SARS-CoV-2 через ГЭБ в головной мозг [4].
Не последнее значение в патогенезе поздних неврологических осложнений имеют и ятрогенные факторы. Продолжительное применение глюкокортикостероидов в больших дозах, моноклональных антител, направленных на различные звенья воспалительного каскада, проведение длительной аппаратной дыхательной поддержки являются факторами, которые активно влияют на кровоток в головном и спинном мозге и напрямую или косвенно воздействуют на метаболизм нервных клеток. Прослеживается тенденция к увеличению частоты и тяжести неврологических осложнений в случаях тяжелого течения COVID-19, что свидетельствует в пользу данного предположения.
На настоящий момент выделяют 3 группы неврологических осложнений, связанных с перенесенной COVID-19-инфекцией:
1) поражение ЦНС;
2) поражение периферической нервной системы;
3) поражение скелетно-мышечной системы.
Неспецифичные симптомы неврологических осложнений при COVID-19 включают головную боль, спутанность сознания, головокружение, усталость, повышенную утомляемость, снижение работоспособности, тошноту, рвоту, синкопе [5].
В недавнем исследовании, опубликованном в Lancet Psychiatry в 2021 г., была проведена ретроспективная количественная оценка частоты неврологических или психических осложнений в когорте из 236 379 больных, выживших после COVID-19, и в контрольной группе пациентов, которые переболели гриппом или какой-либо другой респираторной инфекцией, но не имели COVID-19. Заболеваемость любыми такими осложнениями в группе новой коронавирусной инфекции составила 33,6%, включая тревогу (17,4%), депрессию (13,7%), бессонницу (5,4%), энцефалопатию (4,7%), плекситы/невриты (2,85%), ишемический инсульт (2,1%), деменцию (2,67%), психоз (1,4%), нервно-мышечные и мышечные заболевания (0,5%), геморрагический инсульт (0,56%), паркинсонизм (0,11%), энцефалиты (0,1%), синдром Гийена–Барре (0,08%) [6].
В свою очередь, в недавно опубликованном систематическом обзоре и метаанализе Lopez-Leon S. et al. (2021), включившем данные 47 910 пациентов, были представлены результаты оценки распространенности долгосрочных эффектов COVID-19. Этот метаанализ показал, что у 80% пациентов, инфицированных SARS- CoV-2, развились один или несколько длительных неврологических симптомов, наиболее частыми из которых были усталость (58%), головная боль (44%) и расстройство внимания (27%). Из других неврологических проявлений наблюдались аносмия (21%), потеря памяти (16%), потеря слуха или шум в ушах (15%), озноб (7%), головокружение (3%) и инсульт (3%) [7].
Бульбарные нарушения при COVID-19 были обнаружены только в исследовании Lechien J.R. et al., проведенном в Европе в 2020 г. (средний возраст пациентов 39 лет): частота встречаемости дисфонии в нем составила 28%, дисфагии — 19% [8].
В исследовании Mao L. et al. (2020), по результатам обследования 214 пациентов, госпитализированных по поводу COVID-19, частота острого нарушения мозгового кровообращения (ОНМК) составила 2,8 % (6 случаев, в том числе 5 по ишемическому типу), а при тяжелом течении COVID- 19 – 5,7% (5 случаев, в том числе 4 по ишемическому типу) [9].
Острый миелит относится к достаточно редким осложнениям коронавирусной инфекции, однако требует внимания из-за тяжести неврологических нарушений. В обзоре Roman G.C. et al. (2021) были проанализированы 43 наблюдения острого поперечного миелита, ассоциированного с COVID-19, у пациентов из 21 страны: частота развития этого осложнения составила 0,5 на 1 млн человек с примерно равным распределением между мужчинами и женщинами (53 и 47% соответственно). Средний возраст пациентов за вычетом детей (n=3) составил 49 лет (от 21 года до 73 лет). Основными клиническими проявлениями миелита выступали тетраплегия (58%) и параплегия (42%), которые развивались у большинства (68%) наблюдаемых через 10–42 сут после дебюта COVID-19; в 32% случаев этот период составлял от 15 ч до 5 дней. В 70% случаев объем поражения спинного мозга был представлен четырьмя сегментами [10].
Переходя непосредственно к ретроспективному анализу историй болезни пациентов 8-го неврологического отделения ГНОКБ, хотелось бы отметить, что полученные нами результаты несколько отличаются от данных зарубежных коллег, что можно связать с особенностями маршрутизации пациентов.
Нами были выявлены следующие особенности течения ПКС (табл.).
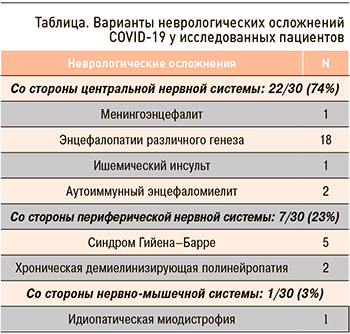
1) Подавляющее преобладание токсико-метаболических энцефалопатий, проявляющихся преимущественно синдромами спутанности, угнетения сознания вследствие токсико-метаболических изменений, вызванных вирусным агентом, а также агрессивно проводимой противовирусной и антибактериальной терапии.
2) Зарегистрированы случаи провокации аутоиммунного энцефаломиелита с явлениями гипоталамического синдрома (центральная гипертермия, несахарный диабет).
3) Из выявленных нами случаев синдрома Гийена–Баре (СГБ) наиболее часто регистрировалось типичное его течение, однако в ряде случаев отмечалась склонность к быстрому его прогрессированию. При этом наблюдались перекрестные варианты течения данного осложнения – сочетание тяжелого СГБ с транзиторной демиелинизацией волокон среднего мозга, подтвержденное результатами нейровизуализации. Такой overlap фенотип ассоциировался с худшим восстановлением на фоне проводимой терапии.
4) Зарегистрирован 1 случай манифестации ОНМК по ишемическому типу в бассейне правой верхней мозжечковой артерии, что вкупе с мировыми и отечественными данными подтверждает наличие васкулопатии артерий среднего и мелкого калибра как одного из звеньев патологического процесса новой коронавирусной инфекции.
5) Зарегистрирован 1 случай идиопатической миодистрофии, клинико-патоморфологически отличающейся от типичного течения полимиозита недостаточно выраженной клинико-лабораторной воспалительной активностью.
ЗАКЛЮЧЕНИЕ
Таким образом, результаты нашего анализа не показали достоверных отличий от соответствующих данных зарубежных и отечественных коллег. Частота неврологических вариантов ПКС на настоящий момент остается точно не известной, однако наблюдается тенденция к тому, что пациенты с тяжелой формой COVID-19 в анамнезе более предрасположены к их развитию после перенесенной инфекции в периоде до 6 мес. При этом наблюдаются единичные атипичные клинические варианты ПКС, в том числе у молодых пациентов, перенесших новую коронавирусную инфекцию в легкой форме, которые в целом не влияют на статистические данные, но требуют дальнейшего изучения.