ВВЕДЕНИЕ
Инсульт является второй по значимости причиной смерти во всем мире, при этом у 53,4% пациентов после острых нарушений мозгового кровообращения (ОНМК) развиваются постинсультные когнитивные нарушения (ПИКН) [1]. После перенесенной коронавирусной инфекции так же, как и после перенесенного ОНМК, у пациентов возникают когнитивные нарушения (КН) [2–4].
Если при инсульте зоны поражения головного мозга, определяющие вероятное развитие КН, установлены достаточно четко, равно как и заболевание, предрасполагающие к развитию когнитивных расстройств [5, 6], то механизм развития, морфология КН при COVID-19 в настоящее время проходит этап изучения [7–10]. Считается, что в формировании КН при COVID-19 играют роль нейротропность вируса SARS-CoV-2, системное воспаление, применение искусственной вентиляции легких, эндотелиальная дисфункция, гиперкоагуляция, приводящая к цереброваскулярной ишемии, острый респираторный дистресс-синдром в случае тяжелого течения инфекции [8]. Общеизвестен процесс определенного регресса неврологической симптоматики в остром периоде ишемического инсульта [11]. У определенной части пациентов регресс достигает значительной степени, у части пациентов тенденция к восстановлению когнитивных функций останавливается и формирует ПИКН [12, 13]. Динамика состояния когнитивных функций при коронавирусной инфекции полноценно не изучена. В настоящий момент исследование когнитивной дисфункции и ее динамика при COVID-19 и инсульте являются актуальными.
Цель исследования – оценить когнитивный статус и динамику КН у пациентов с коронавирусной инфекцией, осложненной пневмонией, и у пациентов в остром периоде ишемического инсульта.
МАТЕРИАЛ И МЕТОДЫ
Набор пациентов проводился в отделении пульмонологии базового инфекционного госпиталя и в неврологическом отделении для больных с ОНМК на базе КГБУЗ «Красноярская межрайонная клиническая больница № 20 им. И.С. Берзона» г. Красноярска. Пациентами было подписано информированное добровольное согласие на участие в исследовании. Данное исследование было одобрено локальным этическим комитетом ФГБОУ ВО «Красноярский государственный медицинский университет им. профессора В.Ф. Войно-Ясенецкого» Минздрава России.
Все пациенты были разделены на 3 группы. В группу 1 вошли 33 пациента с подтвержденной коронавирусной инфекцией в период наблюдения с декабря 2020 г. по март 2021 г., в группу 2 – 33 пациента с подтвержденной коронавирусной инфекцией в период наблюдения с ноябрь 2021 г. по январь 2022 г., в группу № 3 – 37 пациентов в остром периоде ишемического инсульта (период наблюдения – с декабря 2019 г. по ноябрь 2022 г.). В группах с коронавирусной инфекцией, осложненной пневмонией, объем поражения легочной ткани составлял до 50%, в группе с ОНМК применялась шкала тяжести инсульта NIHSS, медиана составила 6б. Возрастная медиана пациентов в группе 1 составила 50 лет, в группе 2 – 45 лет, в группе 3 – 63 лет. Пол пациентов в проводимом исследовании не учитывался.
Критерии включения для групп 1 и 2: пациенты с лабораторно подтвержденной инфекцией, вызванной SARS-CoV-2 и осложненной пневмонией (либо по данным эпидемиологического анамнеза); возраст 18–65 лет; температура тела ниже 37,0 °C после купирования интоксикационного синдрома; ясное сознание; отсутствие явлений дыхательной недостаточности (SpO2 >95%).
Критерий включения для группы 3: пациенты с подтвержденным полушарным ишемическим инсультом по данным нейровизуализации; возраст 30–75 лет; ясное сознание.
Для пациентов всех трех групп необходимым условием включения в исследование было наличие законченного среднего образования.
Критерии исключения для групп 1 и 2: органическое поражение центральной нервной системы до коронавирусной инфекции; наличие явлений дыхательной недостаточности (SpO2 <95%); наличие когнитивных нарушений или деменции до настоящего заболевания; гипертермия ≥37,0 °C; нарушение сознания; наличие коморбидных состояний (сердечно-сосудистой патологии, сахарного диабета 1-го и 2-го типа в стадии декомпенсации, алкоголизма, употребления наркотических препаратов до исследования).
Критерий исключения для группы 3: наличие соматического заболевания в стадии декомпенсации; наличие эпилепсии в анамнезе или возникший эпилептический припадок в стационаре; пациенты с повторным ишемическим инсультом; геморрагический инсульт; пациенты с афазией средней или тяжелой степени; наличие патологии зрения и слуха.
Тестирование когнитивных функций в трех группах проводилось в первые дни госпитализации и за 1–2 дня перед выпиской из стационара. Шкалы, применявшиеся в исследовании: тест рисования часов, MMSE (Mini-Mental State Examination), FAB (Frontal Assessment Battery), MoCA (Montreal Cognitive Assessment). С помощью шкалы HADS (Hospital Anxiety and Depression Scale – Госпитальная шкала тревоги и депрессии) выполнялась скрининговая оценка эмоционального состояния пациентов.
Статистический анализ осуществлялся с использованием программы IBM SPSS Statistics v.19. Нормальность распределения количественных данных оценивалась с помощью статистического критерия Шапиро–Уилка. Количественные данные оказались непараметрическими. Следующим этапом было проведено сравнение трех несвязанных групп при помощи критерия Краскела–Уоллиса, значения были p <0,05. Далее применялся критерий Манна–Уитни для попарного сравнения несвязанных групп. Оценка динамики когнитивных функций при поступлении и выписке в каждой группе выполнялась с применением статистического критерия Вилкоксона. Количественные данные представлены в виде медианы и квартилей – Me [P25; P75]. Различия между выборками считались статистически значимыми при значении p <0,05.
РЕЗУЛЬТАТЫ
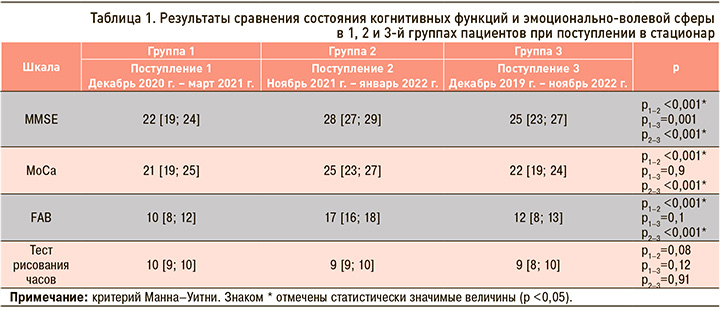
Сравнительные показатели состояния когнитивных функций пациентов в группах 1, 2 и 3 при поступлении в стационар представлены в таблице 1. Из представленных в ней данных видно, что при поступлении в стационар наиболее грубые когнитивные нарушения наблюдались в группе 1. При сравнении показателей достоверно худшие результаты в группе 1 по сравнению с группой 2 были установлены по шкалам MMSE (p <0,001), MoCA (p <0,001), FAB (p <0,001). Кроме того, в группе 1 отмечались достоверно худшие результаты по шкале MMSE в сопоставлении с группой 3 (p <0,001). При сравнении показателей в группах 2 и 3 установлены более грубые КН у пациентов в остром периоде инсульта (группа 3) – по MMSE (p <0,001), MoCA (p <0,001) и FAB (p <0,001). При оценке результатов теста рисования часов в исследуемых трех группах статистически значимых отличий не наблюдалось, что, вероятно, обусловлено сохранностью зрительно-пространственного гнозиса у исследованных пациентов при поступлении в стационар или малой чувствительностью шкалы.
В таблице 2 представлены результаты оценки состояния когнитивных функций у пациентов групп 1, 2 и 3 при выписке. Как следует из приведенных данных, в группе 2 при выписке из стационара показатели когнитивных функций были статистически значимо лучше, чем в группе 1, по шкалам MMSE (p <0,001), MoCA (p <0,001), FAB (p <0,001). В группе 3 (пациенты с ишемическим инсультом) отмечались лучшие показатели когнитивных функций по данным MMSE (p <0,001), MoCA (p=0,002), FAB (p <0,001), чем в группе 1. При сравнении показателей в группах 2 и 3 перед выпиской из стационара по большинству шкал принципиальных различий выявлено не было, за исключением результатов по шкалам FAB (p <0,001) и MMSE (p=0,005), которые были лучше в группе 2.

Также нами выполнялась оценка динамики КН в исследуемых группах. При сравнении результатов по шкалам MoCa, MMSE, FAB, теста рисования часов с использованием критерия Вилкоксона в группах 1 и 2 статистически значимой разницы между ними при поступлении и выписке обнаружено не было. В то же время в группе пациентов, перенесших ишемический инсульт (острый период) в соответствии с критерием Вилкоксона была установлена статистически значимая разница по шкалам MMSE (p <0,001), MoCa (p <0,001) и FAB (p <0,001) при поступлении и выписке. Это свидетельствует об улучшении когнитивных функций в группе 3 к моменту выписки из стационара.
ОБСУЖДЕНИЕ
КН были выявлены во всех трех исследуемых группах. Наиболее выраженные КН были в первую «волну» коронавирусной инфекции, осложненной пневмонией, как при поступлении в стационар, так и на момент выписки (группа 1, период наблюдения с декабря 2020 г. по март 2021 г.), несмотря на соматическое выздоровление пациентов. В период наблюдения в последующую «вспышку» инфекции (группа 2, с ноября 2021 г. по январь 2022 г.), у пациентов также наблюдались и сохранялись КН на момент выписки, но они не являлись столь же грубыми, как в группе 1. В исследуемой группе с ишемическим инсультом (группа 3) когнитивные расстройства были умеренными. При оценке тенденции к восстановлению когнитивных функций на момент выписки только в группе пациентов с ишемическим инсультом отслеживалась положительная динамика, тогда как в группах пациентов с COVID-19 такие изменения в нашем исследовании не отмечались. Динамика когнитивного улучшения после перенесенного ишемического инсульта подтверждается и другими авторами: за счет нейропластичности, уменьшения отека головного мозга, компенсаторных механизмов происходит тенденция к восстановлению когнитивных функций в первые 10 дней стационарного лечения пациентов [12, 13]. В исследовании О.В. Дементьевой с соавт. в котором проводилась оценка динамики КН в остром периоде ишемического инсульта, также было обнаружено, что к выписке на 19–21-й день происходило улучшение когнитивных функций [11]. Как уже указывалось выше, положительной динамики когнитивных функций в первые 10 дней пребывания в стационаре пациентов с COVID-19-ассоциированной пневмонией выявлено не было.
По всей вероятности, можно предположить, что значительная разница в состоянии когнитивного статуса у пациентов в остром периоде COVID-19 без явного поражения ЦНС в периоды 2020–2021 и 2021–2022 гг. обусловлена изменением активности вируса и иммунным состоянием больных. Эти периоды совпадают с пиками заболеваемости в Красноярском крае. С нашей точки зрения, вызывает интерес отсутствие положительной динамики КН при COVID-19-ассоциированной пневмонии через 7–10 дней заболевания, что актуализирует целенаправленную нейродиагностическую работу с пациентами, перенесшими коронавирусную инфекцию в 2020–2022 гг. [14]. Кроме того, в имеющейся литературе достаточно подробно обсуждаются механизмы развития поражения мозга при COVID-19, вызывающие конкретные неврологические расстройства в виде ишемического инсульта, миелита, острой геморрагической некротизирующей энцефалопатии, синдрома Гийена–Барре [14–16]. Механизм развития КН при COVID-19-ассоциированной пневмонии без явной неврологической симптоматики, с нашей точки зрения, до конца остается неясным. Также остается открытым вопрос о необходимости проведения нейровизуализации головного мозга в вышеназванной категории пациентов.
ЗАКЛЮЧЕНИЕ
Как при коронавирусной инфекции в остром периоде без явного поражения ЦНС, так и при ишемическом инсульте в первые дни заболевания наблюдаются когнитивные нарушения, сохраняющиеся к моменту выписки из стационара. При этом, в отличие от групп пациентов с коронавирусной инфекцией, осложненной вирусной пневмонией, у больных в остром периоде инсульта отмечается определенная тенденция к восстановлению когнитивных функций к выписке. Наиболее выраженные нарушения по всем нейропсихологическим шкалам наблюдались в группе пациентов, перенесших COVID-19 в 2020 г. Требуется дальнейшее изучение этой проблемы, наблюдение пациентов в восстановительном периоде, а при сохранении нарушений – их медикаментозная коррекция и применение реабилитационных методик.