Смертность от сердечно-сосудистых заболеваний остается одной из наиболее высоких в структуре общей смертности в нашей стране [1]. Одним из самых значимых факторов риска сердечно-сосудистых заболеваний является сахарный диабет (СД). По данным Российского регистра СД, распространенность стенокардии напряжения среди больных СД 1 типа составляет 12,9%, среди пациентов с СД 2 типа – 14,5%. Инфаркт миокарда в анамнезе имеют 2,8 и 3,8% зарегистрированных больных СД 1 и 2 типа соответственно. Распространенность СД в мире постоянно возрастает, в особенности это касается СД 2 типа [2].
Наиболее высокий риск неблагоприятных исходов приходится на долю больных, перенесших острый коронарный синдром (ОКС). Известно, что и у больных с ОКС наличие СД ухудшает прогноз, приводя к повышению риска развития неблагоприятных исходов [3, 4]. При этом ведение больных с СД и ОКС не всегда оказывается более интенсивным. Целью нашей работы было проанализировать особенности течения и исходов ОКС у больных с сахарным диабетом в реальной клинической практике.
МАТЕРИАЛ И МЕТОДЫ
В исследование включены пациенты, наблюдавшиеся в 2 многоцентровых исследованиях ОРАКУЛ I и II (ОбостРение ишемической болезни сердцА: логиКо-вероятностные пУти прогнозирования течения для оптимизации Лечения). В исследовании ОРАКУЛ I наблюдались 1193 больных, перенесших эпизод ОКС из 16 центров, 7 городов (Москва, Челябинск, Казань, Пермь, Ставрополь, Ростов-на-Дону, Санкт-Петербург). В исследование включали больных с нестабильной стенокардией (НС) и инфарктом миокарда (ИМ) с подъемом и без подъема сегмента ST. Наблюдение начиналось с 10 дня от момента острого коронарного события. Развитие рецидива ИМ или повторных ишемических эпизодов длительностью более 10 мин служило основанием для отсрочки включения больного в исследование еще на 10 дней. Подробно критерии включения в исследование описаны нами ранее [5]. Набор в исследование проводился в 2004–2007 гг.
В исследование ОРАКУЛ II включено 1655 больных ОКС, имевших показание к проведению чрескожных коронарных вмешательств (ЧКВ) в данную госпитализацию, вне зависимости, проведено ЧКВ или нет. Включение в исследование проводилось с 2014 по 2017 г. Подробно критерии включения описаны в предшествующих публикациях [6].
В представленный анализ вошли данные о 1502 больных, доступные для анализа на момент написания работы. Критериями исключения были отсутствие согласия больного на участие в исследовании или невозможность контакта с больным после выписки.
Все пациенты должны получали стандартную терапию на основании действующих рекомендаций.
Статистическая обработка данных проводилась при помощи программы SPSS 23.0. Для протяженных показателей был проведен анализ распределения и критериев его соответствия нормальному. Для протяженных переменных рассчитывали средние величины и величины стандартного отклонения (M±SD). Если распределение соответствовало нормальному, для анализа достоверности их различия применяли t-критерий Стьюдента, при отличии от нормального распределения применяли непараметрические методы расчета. Дискретные величины сравнивали по критерию c2 Пирсона. Отметим, что из 354 (23,6%) пациентов 7 имели СД 1 типа и 347 – СД 2 типа. Различия считали статистически значимыми при р <0,01.
Для оценки независимости влияния клинических факторов на риск неблагоприятного исхода использовали логистическую регрессию. Параметры, продемонстрировавшие статистическую значимость в ходе однофакторного анализа, были включены в многофакторный анализ.
Представленная работа является инициативным открытым наблюдательным многоцентровым исследованием, организованным кафедрой терапии, кардиологии и функциональной диагностики ФГБУ ДПО «Центральная государственная медицинская академия» Управления делами Президента РФ.
РЕЗУЛЬТАТЫ
Клиническая характеристика больных, включенных в исследования ОРАКУЛ I и ОРАКУЛ II, представлена в табл. 1. В исследовании ОРАКУЛ I было 175 больных с СД (14,7%) – 1 больной с СД 1 типа и 174 больных с СД 2 типа. В исследовании ОРАКУЛ II больных с СД было 354 (23,6%), 7 больных с СД 1 типа и 347 больных с СД 2 типа. Различия в частоте СД оказались статистически значимыми.

Больные в исследовании ОРАКУЛ II были достоверно старше (65,7 и 61,1 года соответственно). В когорте ОРАКУЛ II было больше больных с артериальной гипертензией (АГ), ишемической болезнью сердца (ИБС), инсультом и периферическим атеросклерозом в анамнезе. Эти различия могут быть следствием различия групп по возрасту. Частота ИМ в анамнезе и сердечной недостаточности (СН) в двух регистрах достоверно не отличались. В обоих регистрах у больных с СД выше была частота СН в анамнезе. Достоверных различий по полу не было, однако в обоих регистрах среди больных с СД преобладали женщины, а среди больных без СД – мужчины.
 Учитывая достоверные различия в возрасте больных, наблюдавшихся в регистрах ОРАКУЛ I и ОРАКУЛ II, был дополнительно проведен анализ частоты выявления сахарного диабета в разных возрастных группах (табл. 2). У больных всех возрастных групп, кроме пациентов старше 80 лет, частота встречаемости сахарного диабета была достоверно выше среди пациентов регистра, проведенного в 2014–2017 гг.
Учитывая достоверные различия в возрасте больных, наблюдавшихся в регистрах ОРАКУЛ I и ОРАКУЛ II, был дополнительно проведен анализ частоты выявления сахарного диабета в разных возрастных группах (табл. 2). У больных всех возрастных групп, кроме пациентов старше 80 лет, частота встречаемости сахарного диабета была достоверно выше среди пациентов регистра, проведенного в 2014–2017 гг.
В исследовании ОРАКУЛ I нет данных о внутригоспитальной летальности и частоте неблагоприятных исходов, которые регистрировались в первые 10 дней от момента госпитализации в связи с ОКС. Эти данные доступны для анализа только в исследовании ОРАКУЛ II (табл. 3). Достоверных различий в частотах неблагоприятных событий у больных с СД и без СД не зарегистрировано.

На рис. 1 представлены данные о проводившихся в стационаре внутрикоронарных вмешательствах.
У больных ОКС с подъемом сегмента ST (ОКСПST) коронароангиография (КАГ) была проведена у 90,3% больных, ЧКВ выполнены у 78,4% больных. При этом у больных с СД, по сравнению с пациентами без СД, значимо выше была частота многососудистого поражения (8,3 против 1,2%, р=0,020) и соответственно ниже частота выполненных ЧКВ. Среди больных ОКС без подъема сегмента ST (ОКСБПST) неотложная КАГ была проведена у 71,6% больных. ЧКВ выполнены у 49,3% больных, достоверных различий в частоте выполненных ЧКВ у больных с СД и без СД не выявлено.
Было проведено сравнение частоты неблагоприятных исходов, развившихся с 10-го дня от момента дестабилизации ОКС в течение года наблюдения. Пациенты, у которых в исследовании ОРАКУЛ II неблагоприятные исходы развились в первые 9 дней от индексного события, а также больные, у которых нет данных о наблюдении после выписки из стационара, из этого анализа были исключены. У всех больных был проведен анализ частоты развития неблагоприятных исходов как в группах в целом, так и в зависимости от наличия сахарного диабета (табл. 4).
У больных с сахарным диабетом, как в когорте ОРАКУЛ I, так и в когорте ОРАКУЛ II, была выше частота смертей от сердечно-сосудистых причин [ИМ, внезапная смерть, смерть от СН, тромбоэмболии легочной артерии (ТЭЛА)] и всех смертей. Частота смертей от инсульта и внесердечных причин в регистрах ОРАКУЛ I и ОРАКУЛ II существенно не различалась, как и смертность от любых причин.
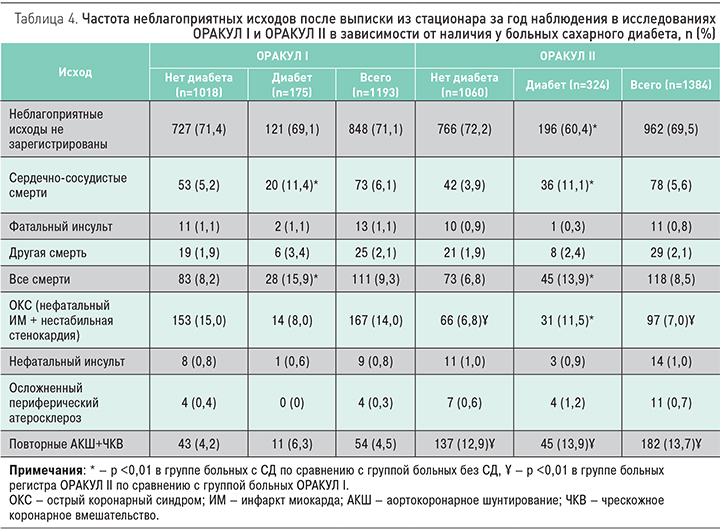
В регистре ОРАКУЛ II было зарегистрировано меньше повторных эпизодов ОКС – 7% по сравнению с 14% в ОРАКУЛ I. В исследовании ОРАКУЛ I у больных с СД было зарегистрировано меньше повторных эпизодов ОКС, в регистре ОРАКУЛ II – больше. Закономерно частота повторных хирургических реваскуляризаций в исследовании ОРАКУЛ II была существенно выше (13,7 и 4,5% соответственно), как у больных с диабетом, так и у больных без СД, что связано с изменением тактики ведения больных.
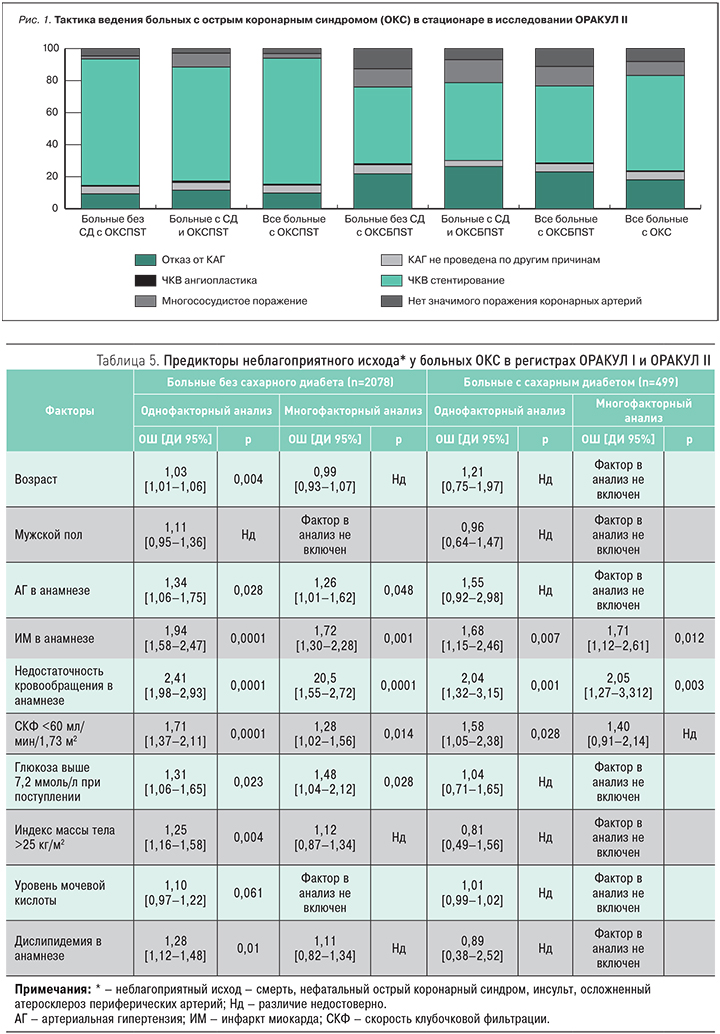
Мы проанализировали факторы, влияющие на риск развития неблагоприятного исхода (комбинированная конечная точка – смерть, нефатальный ОКС, инсульт, осложненный атеросклероз периферических артерий) у больных с сахарным диабетом и без него (табл. 5). У больных без СД с риском неблагоприятного исхода независимо ассоциировались наличие в анамнезе АГ, ИМ, СН, снижение СКФ и повышенная гликемия при поступлении в стационар. Избыточная масса тела, возраст, а также дислипидемия в анамнезе продемонстрировали ассоциацию с неблагоприятными исходами в однофакторном анализе, однако влияние не было независимым. У больных с СД однофакторный анализ показал ассоциацию с неблагоприятным исходом только для трех факторов: ИМ и СН в анамнезе и снижение СКФ. Нарушение функции почек в многофакторном регрессионном анализе утратило значимую ассоциацию с развитием неблагоприятного исхода.
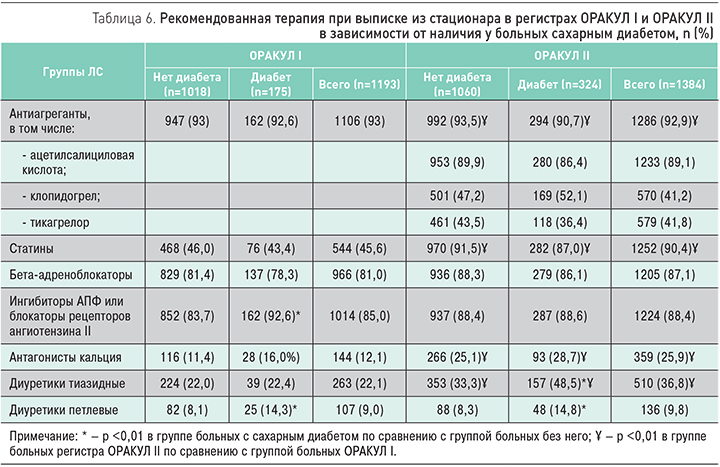
При анализе терапии, рекомендованной больным при выписке (табл. 6), было показано, что после выписки из стационара существенно возросла частота назначения статинов. Кроме того, чаще рекомендовались антагонисты кальция и тиазидные диуретики, что отражает различия в частоте и тяжести сопутствующей АГ в двух регистрах. При выписке из стационара большинству больных рекомендовалась антитромбоцитарная терапия (АТТ). Следует отметить, что в исследовании ОРАКУЛ II 41,8% больных в составе двойной терапии был рекомендован прием тикагрелора, 41% больных – клопидогрела, 7,2% больных при выписке получили только один антитромбоцитарный препарат (ацетилсалициловую кислоту или клопидогрел).
В исследовании ОРАКУЛ II у 1036 больных доступны данные о АТТ, проводившейся после выписки из стационара. 302 больных на протяжении года продолжили прием ацетилсалициловой кислоты (АСК) и клопидогрела (29,5%), 253 больных получали АКС и тикагрелор (24,4%), у 248 больных тикагрелор был заменен на клопидогрел (23,9%), 229 больных после выписки получали только один антитромбоцитарный препарат (АСК или клопидогрел) (22,1%). У больных с сахарным диабетом частота неблагоприятных исходов в течение года была существенно выше при терапии АСК и клопидогрелем, а также у больных, где АТТ была изменена. При терапии АСК и тикагрелором достоверных различий в частоте неблагоприятных событий не было (рис. 2).
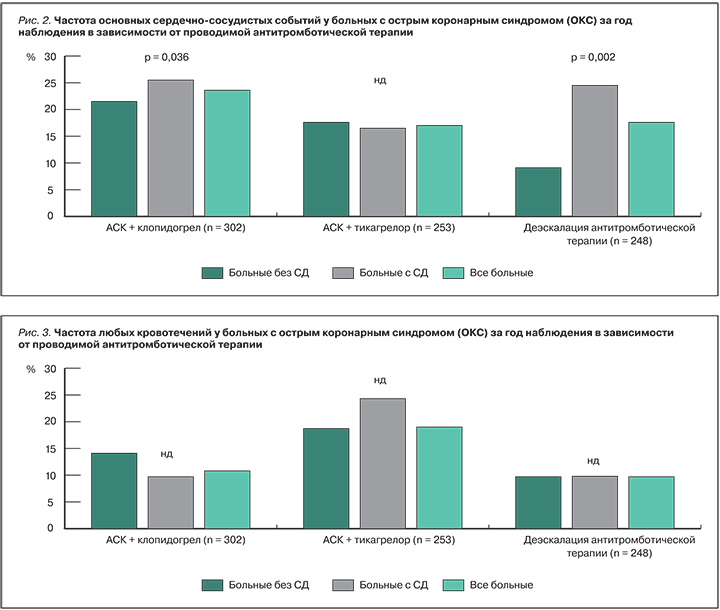
Частота кровотечений у больных с СД и без него существенно не отличалась (рис. 3).
ОБСУЖДЕНИЕ
По данным различных международных регистров, доля больных СД в когортах пациентов с ОКС колеблется от 22 до 34%. Например, в регистре GRAPE (GReek AntiPlatElet registry) частота сахарного диабета оказалась сопоставимой с частотой в регистре ОРАКУЛ II – 22,9% [7]. Существуют популяции со значительно большей распространенностью сахарного диабета. Так, в регистре больных с ОКС, проведенном в Омане, Кувейте, ОАЭ и Бахрейне (Gulf COAST Registry), больные с сахарным диабетом составили 47% от всех госпитализированных больных ОКС [8]. В индийском регистре молодых больных ОКС доля больных с сахарным диабетом составила 44% [9]. В Словакии в регистре больных ОКС SLOVAKS доля пациентов с диабетом составила 34% [10].
Нужно отметить, что в исследовании ОРАКУЛ I, проведенном в 2004–2007 гг., частота сахарного диабета была существенно ниже – 14%. В национальном Датском регистре больных ОКС, проведенном в те же годы (2005–2007), частота СД составила 11% [11].
Значимость сахарного диабета как фактора риска неблагоприятного исхода приобретает все большее значение в связи с увеличением заболеваемости сахарным диабетом. В нашем исследовании частота диагностированного сахарного диабета среди больных ОКС за 10 лет выросла с 14 до 24%, что может иллюстрировать как увеличение заболеваемости, так и улучшение диагностики сахарного диабета в реальной клинической практике нашей страны. Нужно отметить, что увеличение выявления диабета среди больных ОКС зарегистрировано во всех возрастных группах.
В обоих проведенных регистрах больные с СД были старше по возрасту. Аналогичные данные были получены в греческом регистре GRAPE (в среднем 60 лет в группе больных без диабета и 65 лет в группе больных с диабетом) [7].
В Итальянском многоцентровом регистре больных ОКС и сахарным диабетом средний возраст таких больных оказался 68 лет, что близко к данным нашего исследования. При анализе 10 крупных европейских регистров больных ОКС средний возраст больных с сахарным диабетом был от 64 до 71 года [12].
При анализе неблагоприятных исходов показано, что у больных с сахарным диабетом оказался выше уровень сердечно-сосудистой и общей смертности, что подтвердили данные регистров, как современного, так и проведенного 10 лет назад, до внедрения в практику здравоохранения сосудистых центров. Отсутствие значимых различий в частоте неблагоприятных исходов в регистрах ОРАКУЛ I и ОРАКУЛ II, несмотря на изменение тактики ведения больных, может быть связано с существенными различиями между обследованными когортами по возрасту.
Уровень внутригоспитальной летальности у больных с СД, по разным данным, составляет от 1,43% (MULTIPRAC) до 9,42% (Belgian STEMI). В нашем исследовании в регистре ОРАКУЛ II умерли в период первичной госпитализации 3,9% больных без СД и 5,0% больных с СД. Годовая летальность после выписки из стационара в Европейских регистрах составляла у больных с сахарным диабетом от 3,27% (MULTIPRAC) до 10,45% (SCAAR), в ОРАКУЛ II – 8,5%. В нашем регистре существенно более высокой оказалась частота проведения процедур реваскуляризации после выписки из стационара – 13,9%, в то время как в регистре SPUM-ACS она составила 7,89%.
В нашем исследовании экстренная реваскуляризация проведена у 56% больных с сахарным диабетом и у 60% больных без СД. Ангиография проводилась у 80% больных. Среди больных с сахарным диабетом существенно выше оказалась доля больных с многососудистым поражением (12,8 против 7,3% у больных без СД). В европейских регистрах ОКС у больных с сахарным диабетом КАГ проводилась в 70,4% в исследовании CZECH-2, в 81,3% – в регистре DIOCLES, в 85,5% – в AMIS Plus и в 100% случаев – в исследованиях MULTIPRAC, SCAAR, SPUM-ACS, AAPCI/ADAPT и ATACS. Частота проведения ЧКВ варьировала от 55,5% в регистре DIOCLES до 94,7% в протоколе SPUM-ACS. [13].
При анализе клинических предикторов неблагоприятных исходов было показано, что гипергликемия при поступлении является значимым предиктором неблагоприятного исхода у больных, не имеющих диагноза сахарного диабета. Наличие гипергликемии является показателем имеющихся нарушений углеводного обмена, преддиабета или недиагностированного диабета, что, как показывают наши данные, имеет существенное значение в определении прогноза больных. Повышенная гликемия ассоциируется с активацией внутрисосудситого воспаления, избытком катехоламинов, усилением протромботических сдвигов, что и приводит к повышению риска коронарных событий [14]. Аналогичные данные были получены в наблюдательном исследовании, проведенном в 2017 г. в Великобритании, где доля больных с выявленным повышением уровня глюкозы при ОКС достигала 48%, при этом только 20% больных имели диагноз СД. Выявленная повышенная гликемия оказалась одним из факторов неблагоприятного исхода, что заставило авторов статьи модифицировать диагностический алгоритм для СД [15]. В регистре ОКС, проведенном в Италии в 2015 г., повышенная гликемия при поступлении у пациентов с ОКС ассоциировалась с более высоким риском острой сердечной недостаточности и ранней смертности, что подчеркивает значимость выявления этих нарушений [16].
У больных без СД среди предикторов неблагоприятного исхода оказалось также нарушение функции почек, в то время как у пациентов с СД снижение СКФ было ассоциировано с риском неблагоприятных исходов только в однофакторном анализе, а при многофакторном утрачивало независимость. По-видимому, основное значение имеет сам диагноз СД, а поражение почек оказывается вторичным по отношению к основной патологии.
У всех больных, независимо от наличия СД, среди наиболее значимых клинических предикторов неблагоприятных исходов были наличие в анамнезе ИМ и СН. Роль этих факторов неоднократно была продемонстрирована в различных исследованиях, они входят и в различные шкалы оценки риска у больных ОКС [17, 18].
Современные рекомендации [19, 20] рассматривают назначение новых блокаторов P2Y12 рецепторов (тикагрелора и прасугреля) в составе двойной АТТ при ОКС как приоритетное, по сравнению с клопидогрелем. При этом в реальной практике частота назначения этих препаратов оказывается ниже, чем предусмотрено рекомендациями. Например, по данным Итальянского многоцентрового регистра больных с ОКС и сахарным диабетом, клопидогрел в составе двойной терапии назначали 51% больных ОКС и сахарным диабетом, 49% больных получали тикагрелор или прасугрель [12]. В нашем исследовании в целом клопидогрел и тикагрелор рекомендовались с одинаковой частотой, а среди пациентов с сахарным диабетом частота назначения была несколько ниже, чем в целом по группе, хотя эти больные и относятся к числу больных высокого риска. При этом только при терапии тикагрелором частота неблагоприятных исходов у больных с сахарным диабетом не отличалась от группы больных без диабета. Аналогичные данные были получены в регистре GRAPE [7]. При терапии клопидогрелем она была выше у больных с СД. Частота кровотечений на фоне терапии тикагрелором была выше, чем на фоне терапии клопидогрелем, не отличаясь существенно в зависимости от наличия у больных СД. Интересно отметить, что в американском регистре больных ОКС с участием 10 клиник отмечена даже меньшая частота кровотечений у больных с сахарным диабетом, получающих двойную антитромбоцитарную терапию по сравнению с больными без диабета [21].
Таким образом, значительная частота сочетания ОКС и сахарного диабета в реальной клинической практике и появление антидиабетических средств, улучшающих выживаемость больных с осложнениями атеросклероза, требует, по-видимому, разработки отдельных стандартов ведения и рекомендаций для таких больных.