Желчнокаменная болезнь (ЖКБ), являясь широко распространенным заболеванием, часто вызывающим временную нетрудоспособность и приводящим к оперативным вмешательствам, ложится тяжелым бременем на систему общественного здравоохранения. Так, в экономически развитых странах конкременты в желчном пузыре определяются у 10–20% взрослого населения [1, 2]. Только в США ежегодно производится более 750 000 холецистэктомий с прямыми и косвенными расходами более 6,55 млрд долл. в год и частотой фатального исхода 0,12% от всех смертей за указанный период времени [3].
Благодаря идентификации факторов риска развития ЖКБ, представляется возможным раннее прогнозирование развития болезни и принятие мер, направленных на медикаментозный лизис конкрементов. В клинических исследованиях к факторам риска ЖКБ относят женский пол, средний возраст, беременность, определенную этническую принадлежность, наследственную предрасположенность, избыточную массу тела и низкую физическую активность [4, 5]. В последние годы опубликовано достаточно большое число исследований, которые направлены на изучение влияния метаболических нарушений, участвующих в формировании желчных камней. Это тем более важно, что распространенность ЖКБ и ее исходы ассоциируются с метаболическими нарушениями, поскольку существует тесная патогенетическая взаимосвязь между камнеобразованием и компонентами метаболического синдрома (МС) [6, 7], к которым относятся нарушения углеводного и липидного обмена, повышенное артериальное давление (АД) и избыточная масса тела. В связи с этим часть авторов рассматривает ЖКБ как составную часть МС [8, 9].
Известно, что чем больше компонентов МС, тем выше риск развития ЖКБ [10]. Наличие 4 или 5 компонентов МС увеличивает вероятность образования желчных камней в 3 раза [11]. Сочетание метаболических нарушений и камнеобразования нередко приводит к осложненному течению ЖКБ. Полученные данные говорят о том, что среди пациентов с МС частота осложненного течения ЖКБ выше, чем у лиц без метаболических нарушений [12]. Несмотря на доказанное влияние избыточной массы тела, артериальной гипертензии (АГ), сахарного диабета (СД) и дислипидемии на формирование желчных камней [8, 13], вопрос о динамике роста конкрементов у пациентов с метаболическими нарушениями остается неясным.
Целью настоящего исследования стало определение связи между выраженностью метаболических нарушений и диаметром конкрементов в желчном пузыре.
МАТЕРИАЛ И МЕТОДЫ
Обследовано 60 пациентов с разной степенью метаболических нарушений в возрасте от 42 до 65 лет. В первую группу вошло 30 пациентов с конкрементами в желчном пузыре диаметром менее 10 мм, во вторую – 30 пациентов с диаметром конкрементов в желчном пузыре от 10 до 15 мм. Группа сравнения была представлена 30 пациентами с различными проявлениями метаболических нарушений в возрасте от 41 до 63 лет без камней в желчном пузыре.
Все пациенты были обследованы в соответствии с целью и задачами настоящей работы с анализом клинико-инструментальных и лабораторных данных:
- Антропометрические показатели: объем талии (ОТ), индекс массы тела (ИМТ). Масса тела измерялась в легкой одежде и без обуви с точностью до 0,10 кг. Рост пациента фиксировался с точностью до 0,5 см. ИМТ был рассчитан как вес (кг), разделенный на высоту в квадрате (м2). ОТ (с точностью до 0,1 см) измерялся в средней точке между нижней границей ребра и подвздошным гребнем. Показания АД были получены после того, как испытуемые отдыхали сидя в течение 10 мин.
- Биохимические данные: уровень холестерина (ХС), ХС липопротеидов высокой плотности (ХС-ЛПВП), ХС липопротеидов низкой плотности (ХС-ЛПНП), триглицеридов (ТГ), глюкозы.
- Инструментальные: ультразвуковое исследование (УЗИ) органов брюшной полости.
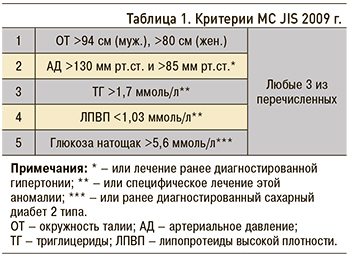
- Метаболические: верификация метаболических нарушений осуществлялась на основании критериев МС JIS (2009 г) (табл. 1).
Статистический анализ: для оценки нормальности распределения переменных использовался тест Шапиро–Уилка, проверка гипотез о равенстве генеральных дисперсий с помощью критерия Левене. Для показателей, не прошедших проверку на нормальность, использовался тест Краскела–Уоллиса, для оценки межгрупповых связей использовался тест Манна–Уитни. Сравнение качественных данных двух групп проводилось с помощью таблиц сопряженности с определением точного критерия Фишера. Для проведения статистического анализа использовалась программа SPSS 22.0 (SPSS Inc, США) для Windows (Microsoft Corporation, США), причем p <0,05 считался статистически значимым.
 РЕЗУЛЬТАТЫ И ОБСУЖДЕНИЕ
РЕЗУЛЬТАТЫ И ОБСУЖДЕНИЕ
Анализ полученных данных базировался на оценке факторов, влияющих на образование конкрементов и увеличение их диаметра. Так, при анализе качественных данных, установленных на основании критериев МС JIS (2009) (см. табл. 1), выявлено, что на образование конкрементов в желчном пузыре оказывают влияние:
- ОТ >94 см (муж.), >80 см (жен.) (р <0,05 между 1 и 3 группами);
- систолическое АД >130 мм рт.ст. и диастолическое АД >85 мм рт.ст., диагностированная ранее АГ (р <0,05 между 1 и 3 группами);
- уровень глюкозы натощак >5,6 ммоль/л или ранее диагностированный СД 2 типа (р <0,05 между 1 и 3 группами).
При оценке межгрупповых связей количественных данных (табл. 2; рис.) было установлено, что увеличение ОТ (р <0,05 между 1 и 3 группами), ИМТ (р <0,05 между 1 и 3 группами) и глюкозы (р <0,05 между 1 и 3 группами) оказывают существенное влияние на образование конкрементов в желчном пузыре.
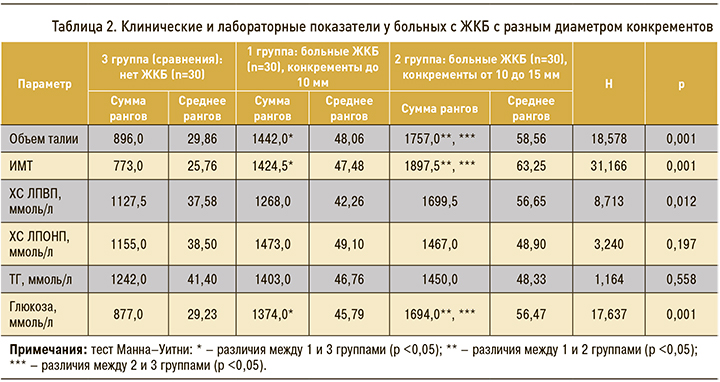
Особый интерес представляют данные по определению факторов, влияющих на увеличение диаметра конкрементов в желчном пузыре. Анализ качественных данных, установленных на основании критериев МС, показал, что на увеличение диаметра конкрементов влияют ОТ >94 см (муж.), >80 см (жен.) (р <0,05 между 1 и 2 группами) и увеличение уровня глюкозы натощак >5,6 ммоль/л или ранее диагностированный СД 2 типа (р <0,05 между 1 и 2 группами). При анализе межгрупповых связей количественных данных установлено влияние ОТ (р <0,05 между 1 и 2 группами), ИМТ (р <0,05 между 2 и 3 группами) и глюкозы (р <0,05 между 1 и 2 группами) на диаметр конкрементов (см. рис.).
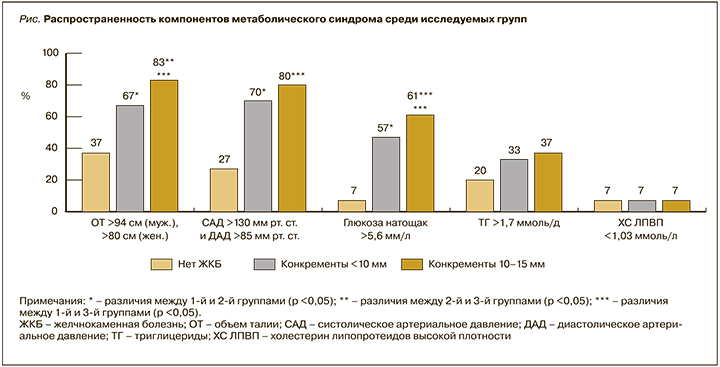
Следует подчеркнуть наличие прямой корреляционной связи между метаболическими нарушениями и размером конкремента в желчном пузыре: при увеличении степени метаболических нарушений увеличивается и диаметр камней (см. рис.). При сравнении клинических и биохимических показателей крови прослеживается тенденция к увеличению диаметра конкрементов по мере возрастания значений ОТ, ИМТ, уровня глюкозы натощак (см. табл. 2).
В последние годы особый интерес вызывает взаимосвязь метаболических нарушений и ЖКБ. Mendez-Sanchez et al. приводят данные о том, что ЖКБ тесно связана с МС [8]. Научно-исследовательская работа, выполненная Y. Chang et al., свидетельствует о высокой частоте встречаемости ожирения и МС у пациентов с ЖКБ [14]. В настоящее время уже установлены особенности влияния метаболических нарушений на течение ЖКБ [12].
ЗАКЛЮЧЕНИЕ
Проведенное сравнительное клиническое исследование в параллельных группах свидетельствует о взаимном влиянии ОТ, ИМТ, АД и уровня глюкозы крови на формирование ЖКБ посредством имеющихся единых звеньев патогенеза. Прогрессивный рост камней связан с увеличением ОТ, ИМТ и изменением параметров липидного и углеводного обмена. Это тем более важно, что, по данным ряда источников, у пациентов с большим диаметром конкрементов, МС и СД отмечается статистически значимое увеличение числа осложненных вариантов течения ЖКБ [15, 16]. Полученные данные демонстрируют важную роль метаболических нарушений в развитии ЖКБ и прогрессировании роста конкрементов в желчном пузыре.


