Хроническая сердечная недостаточность (ХСН) часто сопровождается одним или несколькими сопутствующими несердечными заболеваниями, что усложняет диагностику и ведение больных. Недавние данные Medicare Services показывают, что у 55% пациентов с ХСН есть 5 или более хронических сопутствующих болезней [1]. Результаты экспериментального исследования показали, что у большинства больных (74%) ХСН была как минимум одна коморбидная патология, причем наиболее часто заболевания почек, анемия и сахарный диабет (СД) [2]. Эти сопутствующие заболевания нередко ассоциированы с худшими исходами и более высокой частотой госпитализаций [3, 4].
Более четверти пациентов с ХСН имеют коморбидную патологию легких или почек, что связано с повышенной заболеваемостью и смертностью в общей популяции сердечной недостаточности [2, 5]. Точные механизмы, лежащие в основе повышенного риска смертности пациентов с ХСН и множественными сопутствующими заболеваниями, до сих пор не ясны, однако можно назвать несколько факторов такого риска. Прежде всего ХСН может приводить к увеличению коморбидности; например, из-за усталости и одышки снижается активность пациентов, что играет определенную роль в развитии таких болезней, как СД и ожирение. Кроме того, пациенты с сопутствующими заболеваниями часто имеют более тяжелую ХСН с более высокой вероятностью смертности и госпитализации. Наконец, сопутствующие заболевания могут вызывать ухудшение течения и исхода ХСН из-за приема лекарств, используемых для их лечения [6].
Хотя наличие сопутствующих заболеваний высоко распространено в клинической практике, этот вопрос мало обсуждается в рекомендациях по ведению пациентов с ХСН, а доказательная база скудна и в большинстве случаев носит наблюдательный характер. Так, в клинические исследования, посвященные этому заболеванию, не включались пациенты с сопутствующими некардиологическими болезнями. В то же время тщательное внимание к диагностике и лечению сопутствующих заболеваний у больных ХСН может улучшить результаты лечения. Это определяет необходимость дальнейших исследований в области некардиальной коморбидности в популяции пациентов с ХСН.
Цель исследования – оценить влияние некардиальной коморбидной патологии на качество жизни, психосоциальные факторы и приверженность к терапии у пациентов с ХСН.
МАТЕРИАЛ И МЕТОДЫ
В рамках амбулаторного регистра пациентов с ХСН методом сплошной выборки обследованы 87 больных (27 женщин (31,0%) и 60 мужчин (69,0%), средний возраст 64,1±9,8 лет) ХСН I–III функционального класса (ФК).
75 обследованных больных (86,2%) наряду с ХСН страдали артериальной гипертонией, 68 (78,2%) – ишемической болезнью сердца (включая 57 больных (65,5%) с перенесенным инфарктом миокарда), 20 (22,9%) – кардиомиопатией, 21 (24,1%) – фибрилляцией предсердий.
Все пациенты были информированы о целях и задачах регистра и подписали информированное согласие на участие в исследовании. ХСН диагностировали и оценивали в соответствии с Клиническими рекомендациями ОССН – РКО – РНМОТ «Сердечная недостаточность: хроническая (ХСН) и острая декомпенсированная (ОДСН). Диагностика, профилактика и лечение» (2018) [7]. С целью оценки выраженности клинических признаков ХСН использовалась Шкала оценки клинического состояния больных (ШОКС) для больных ХСН (модификация В.Ю. Мареева, 2000).
Коморбидность больных оценивали с помощью индекса коморбидности (ИК) Чарлсона [8]. Этот индекс представляет собой балльную систему оценки (от 0 до 40) наличия определенных сопутствующих заболеваний и используется для прогноза летальности. При его расчете суммируются баллы, соответствующие сопутствующим заболеваниям, а также добавляется один балл на каждые десять лет жизни при превышении пациентом 40-летнего возраста.
Всем больным было проведено общеклиническое и лабораторное обследование, ЭКГ в 12 общепринятых отведениях, ЭхоКГ. Диагноз ХСН подтверждался по данным ЭхоКГ, натрийуретические пептиды оценены не были. Скорость клубочковой фильтрации (СКФ) определяли, используя уравнение CKD-EPI (Chronic Kidney Desease Epidemiology Collaboration). Качество жизни больных ХСН определяли с помощью опросника Kansas City Cardiomyopathy Questionnaire (KCCQ): в нем баллы варьируются от 0 до 100, и чем выше балл, тем лучше качество жизни. Для оценки когнитивных функций больных использовали Монреальскую шкалу когнитивных функций («Мокатест») с вычислением суммарного балла до возможного максимума 30 баллов. Окончательный общий балл 26 и более считается нормальным. Для оценки психосоциальных факторов использовался валидный скрининговый метод оценки уровня депрессии и тревоги – Госпитальная шкала тревоги и депрессии (Hospital Anxiety and Depression Scale-HADS). Сумма баллов по какой-либо из частей этой шкалы ≥8 соответствует субклинически значимым изменениям.
Способность к самопомощи у больных ХСН оценивалась посредством соответствующей Европейской шкалы [9]. Для оценки приверженности пациентов к лечению использовался тест Мориски–Грина (MMAS-4), который применяется при стандартном обследовании пациентов с различными хроническими заболеваниями для выявления потенциально не приверженных лечению больных, требующих большего врачебного внимания. Пациенты, набравшие 4 балла, считаются приверженными к терапии, 1–2 балла – неприверженными, 3 балла – недостаточно приверженными с риском перехода в группу неприверженных к лечению.
Статистический анализ осуществлялся с помощью пакета встроенных функций программы Microsoft Exel 2010, программы Statistica 10.0 Trial (Statsoft Inc.). Для количественных признаков, имеющих нормальное распределение по Колмогорову–Смирнову, определяли среднее значение признака (М) и среднеквадратичное отклонение (sd). Сравнение показателей проводили с использованием критерия Стьюдента для связанных и несвязанных групп (t). Сравнение качественных переменных выполнялось с использованием критерия χ2. Корреляция определялась методом Пирсона.
РЕЗУЛЬТАТЫ И ОБСУЖДЕНИЕ
Большинство обследованных имело ХСН I–II ФК по шкале ШОКС (74 пациента, 85,1%), остальные 13 пациентов (14,9%) – ХСН III ФК. По результатам ЭхоКГ исследуемые были распределены в следующие группы:
- ХСН с сохраненной фракцией выброса (ФВ >50%) – 60,9% больных;
- ХСН с умеренной систолической дисфункцией (ФВ 40–49%) – 24,1% пациентов;
- систолическая ХСН с ФВ <40% – 14,9% обследованных.
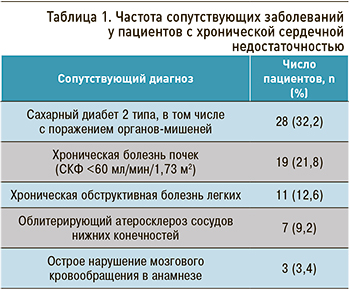 При оценке числа сопутствующих некардиологических заболеваний выявлено, что 49 (56,3%) больных имели низкую коморбидность (ИК ≤3 баллов), 38 (43,7%) – повышенную коморбидность (ИК >3 баллов). Характеристика сопутствующих заболеваний представлена в таблице 1. СД страдали 32,2% пациентов, второй по частоте коморбидной патологией была хроническая болезнь почек (21,8%). Эти результаты совпадают с предыдущими исследованиями, где распространенность хронической болезни почек у разных групп пациентов с ХСН наблюдалась в пределах от 28 до 55% [10], а частота СД – от 22 до 45% [11].
При оценке числа сопутствующих некардиологических заболеваний выявлено, что 49 (56,3%) больных имели низкую коморбидность (ИК ≤3 баллов), 38 (43,7%) – повышенную коморбидность (ИК >3 баллов). Характеристика сопутствующих заболеваний представлена в таблице 1. СД страдали 32,2% пациентов, второй по частоте коморбидной патологией была хроническая болезнь почек (21,8%). Эти результаты совпадают с предыдущими исследованиями, где распространенность хронической болезни почек у разных групп пациентов с ХСН наблюдалась в пределах от 28 до 55% [10], а частота СД – от 22 до 45% [11].
Полученные нами данные свидетельствуют, что пациенты с повышенной коморбидностью (ИК >3 баллов) на 28,7% чаще, по сравнению с больными с низкой коморбидностью, имеют нормальную ФВ (73,4 и 44,7% соответственно; χ2=14,17, р=0,002). Тяжесть ХСН у пациентов с низкой и высокой коморбидностью была сопоставимой.
Ранее было показано, что больные с сохранной ФВ, в отличие от пациентов со сниженной ФВ, имеют повышенную частоту хронической обструктивной болезни легких (ХОБЛ), СД и анемии, которые связаны с неблагоприятным прогнозом [6]. Поскольку современные исследования у больных с сохранной ФВ не смогли продемонстрировать улучшение прогноза под влиянием стандартной терапии ХСН, мы предлагаем уделить внимание лечению коморбидности. Такой подход может быть особенно актуален для пациентов с сохраненной ФВ, когда нет доказанных методов лечения, позволяющих снизить смертность. Учитывая, что многие из сопутствующих заболеваний тесно взаимосвязаны и могут усиливать друг друга, их оценка и коррекция может служить важным элементом комплексного ведения пациентов с ХСН. Коморбидные патологии могут влиять на прогноз и качество жизни несколькими способами [12]. Большинство из несердечных сопутствующих заболеваний требуют применения лекарств, а полипрагмазия, с одной стороны, связана со снижением функционального состояния пациента, с другой ‒ определяет низкую приверженность к лечению. При изучении комплаентности пациентов выявлено, что средний балл по шкале комплаентности составил у них 7,7±1,8. При этом в группе пациентов с низкой коморбидностью этот показатель был 8,6±1,9, а у пациентов с высокой коморбидностью – 6,4±1,4. Число больных с низкой комплаентностью к лечению было больше на 18,2% при высокой коморбидности (8,1% при низкой коморбидности против 26,3% при высокой; χ2=5,22, р=0,02).
Для больных ХСН развитие навыков к самопомощи приобретает принципиальное значение. Исходя из современных рекомендаций по ведению пациентов с этим заболеванием, оптимизация их способности к самопомощи выступает одной из главных задач, решение которой способно улучшить прогноз ХСН, качество жизни и предотвратить повторные госпитализации. В нашем исследовании пациенты продемонстрировали низкий уровень готовности к самопомощи (24,2±1,3 балла из 45 возможных по европейской Шкале самопомощи). У больных с высокой коморбидностью этот показатель составил 22,9±1,5 балла, с низкой – 24,6±1,9 (p=0,08). Наблюдалась обратная корреляционная связь ИК и показателя самопомощи (r=0,25; F=5,1; p=0,03).
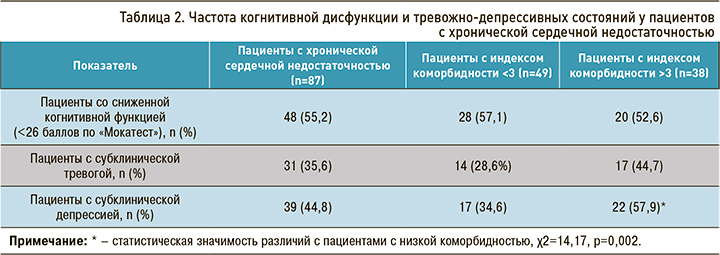
К факторам, которые потенциально могут определять влияние сопутствующей патологии на течение и прогноз ХСН, относятся психосоциальные аспекты и когнитивный дефицит. В таблице 2 представлены результаты оценки когнитивной функции по Монреальской шкале когнитивных функций и уровня депрессии и тревоги по Госпитальной шкале тревоги и депрессии. Около половины обследованных пациентов (55,2%) получили менее 26 баллов по шкале когнитивных функций, что говорит о возможном когнитивном дефиците и требует более внимательной оценки. Согласно полученным нами данным, число сопутствующих заболеваний не оказало влияния на уровень когнитивной функции. Среди пациентов с ХСН 35,6 и 44,8% имели субклиническую тревогу и депрессию, соответственно признаков клинически выраженной тревоги и депрессии выявлено не было. Обращает на себя внимание, что пациенты с высокой коморбидностью на 23,3% чаще (χ2=14,17; р=0,002) имели субклиническую депрессию относительно больных с низкой коморбидностью.
Большинство сопутствующих заболеваний сопровождается различными (физическими) симптомами, такими как усталость, снижение общего состояния и/или одышка. Эти факторы не только ограничивают пациентов в функциональном статусе, но также могут влиять на их социальный статус и тем самым еще больше снижать качество жизни. При оценке с помощью опросника KCCQ выявлены наиболее важные факторы, определяющие снижение качества жизни (рис.). Наибольшее значение пациенты придавали ухудшению качества жизни, физическим ограничениям и симптомам. Обсуждаемые показатели были сопоставимы у пациентов с низкой и высокой коморбидностью, однако имелась тенденция к большему ограничению повседневной активности, выраженности одышки и утомляемости у пациентов с ИК >3.
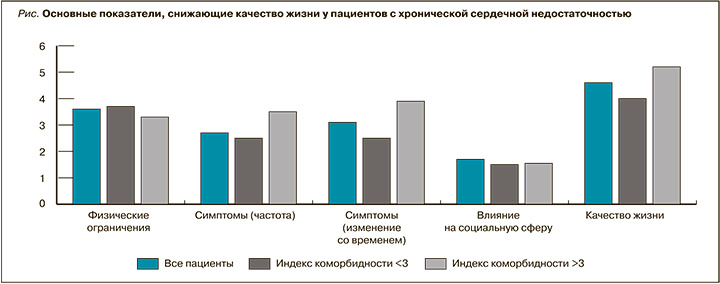
В предыдущих исследованиях большинство сопутствующих заболеваний было связано со значительным снижением среднего балла качества жизни, но снижение качества жизни было более выражено в группе ХОБЛ [13]. В нашем исследовании таких пациентов было около 10%; возможно, именно этим можно объяснить полученные результаты. Нами обнаружена прямая корреляционная связь между индексом коморбидности и выраженностью одышки, оцененной по Канзасскому опроснику (r=0,3; F=3,95; p=0,05).
ЗАКЛЮЧЕНИЕ
- Частота высокой несердечной коморбидности у больных ХСН составляет 43,7%.
- Пациенты с повышенной коморбидностью (ИК >3 баллов) чаще имеют нормальную ФВ левого желудочка и низкую комплаентность к лечению.
- Больные с ХСН и высокой коморбидностью чаще имеют субклиническую депрессию, достоверного влияния ИК Чарлсона на тревогу и качество жизни выявлено не было.


