Проблема распространенности коморбидной патологии среди пациентов приобретает все большую актуальность. Это связано с тем, что в условиях коморбидности многие заболевания приобретают атипичное течение, повышается риск осложнений, усугубляется проблема полипрагмазии, снижается приверженность пациентов к лечению. В конечном итоге это приводит к возникновению сложностей в процессе верификации диагноза и ведения таких пациентов. Коморбидность как сочетание двух и/или более синдромов или заболеваний, патогенетически взаимосвязанных или совпадающих по времени у одного пациента вне зависимости от активности каждого из них, широко представлена среди больных, госпитализированных в терапевтические стационары. На этапе первичной медицинской помощи пациенты с наличием одновременно нескольких заболеваний являются, скорее, правилом, чем исключением [1, 2].
В России ежегодно регистрируются более 1,5 млн случаев внебольничной пневмонии (ВП) [3, 4]. Распространенность пневмонии равна 3,86 на 1000 населения [5]. Согласно данным за 2016 г., в нашей стране заболеваемость острыми респираторными вирусными инфекциями (ОРВИ) достигла 21 658,26 случаев на 100 тыс. населения. Заболеваемость ВП в 2016 г. в России составила 418,02 случая на 100 тыс. населения, смертность от пневмонии – 30 716 случаев [6]. В настоящее время наблюдается увеличение пациентов с тяжелым течением заболевания, а также возрастает смертность от ВП [7].
К основным факторам, определяющим риск развития и прогноз при ВП, относят пожилой возраст, статус курения, прием некоторых лекарственных препаратов (глюкокортикоидов, атипичных нейролептиков, ингибиторов протонной помпы и др.), а также сопутствующие заболевания, такие как сахарный диабет (СД), цирроз печени, хроническая обструктивная болезнь легких (ХОБЛ), алкоголизм, острое нарушение мозгового кровообращения, хроническая почечная недостаточность (ХПН), ишемическая болезнь сердца (ИБС), острая и хроническая сердечная недостаточность (ХСН), фибрилляция предсердий (ФП). По данным многих исследований, при воздействии факторов риска существенно ухудшается прогноз и значительно увеличивается летальность при данном заболевании, достигающая 15–30% [8]. На фоне ОРВИ возможны осложнения со стороны верхних и нижних дыхательных путей у пациентов с хроническими заболеваниями [9]. Оценка особенностей течения ВП в период вспышек ОРВИ становится особенно актуальной в условиях пандемии новой коронавирусной инфекции (COVID-19).
Цель исследования – оценка особенностей коморбидной патологии у пациентов ВП, госпитализированных в стационар в период эпидемии ОРВИ.
МАТЕРИАЛ И МЕТОДЫ
В одномоментном исследовании были рассмотрены материалы 213 историй болезни пациентов, госпитализированных в терапевтический стационар МБУ «Центральная городская клиническая больница № 6» г. Екатеринбурга по поводу ВП в период с декабря 2018 г. по март 2019 г.
Проанализированы сроки первичного обращения за медицинской помощью, верификации диагноза и госпитализации, данные анамнеза заболевания, анамнеза жизни, результаты обследований, которые включали общий осмотр, измерение массы тела и роста с последующим вычислением индекса массы тела, измерение температуры тела, систолического (САД) и диастолического артериального давления (ДАД), частоты сердечных сокращений (ЧСС), частоты дыхания (ЧДД), сатурации крови (SpO2%), определенной методом пульсоксиметрии. При этом дыхательную недостаточность (ДН) классифицировали как ДН I степени при SpO2 более 90–94%, ДН II степени – 75–89%, ДН III степени – менее 75%.
Оценивались данные лабораторных исследований: развернутого общего анализа крови (диагноз «анемия» устанавливали при снижении гемоглобина <110 г/л) [11] и биохимического анализа крови (билирубина, мочевины, креатинина, глюкозы, аланинаминотрансферазы, аспартатаминотрансферазы, фибриногена, сывороточного железа, сывороточного уровня С-реактивного белка), посева мокроты на микрофлору и определения чувствительности к антибиотикам, вирусологического исследования мазков из полости носа и ротоглотки методом полимеразной цепной реакции.
Инструментальное обследование включало рентгенографию органов грудной клетки в передней прямой и боковой проекциях, электрокардиографию в стандартных отведениях.
Коморбидность оценивали с помощью индекса Чарлсон (ИЧ), представляющего собой балльную систему оценки наличия сопутствующих заболеваний. При расчете ИЧ суммируются баллы за наличие наиболее социально значимых хронических неинфекционных заболеваний, к которым относятся перенесенный инфаркт миокарда, сердечная недостаточность, поражение периферических сосудов, преходящее и острое нарушение мозгового кровообращения, деменция, бронхиальная астма (БА), ХОБЛ, диффузные болезни соединительной ткани, язвенная болезнь, цирроз печени, СД, злокачественные опухоли, синдром приобретенного иммунодефицита. К индексу добавляется по 1 баллу за каждые 10 лет жизни, начиная с сорока лет (т.е. 40–49 лет – 1 балл, 50–59 лет – 2 балла и т.д.). Десятилетняя выживаемость при сумме баллов 0 составляет 99%, 1 балл – 96%, 2 балла – 90%, 3 балла – 77%, 4 балла – 53%, 5 баллов – 21% [12].
В зависимости от значения ИЧ пациенты были разделены на две группы:
- 1-я группа – больные с умеренным уровнем коморбидности (≤2 баллов);
- 2-я группа – пациенты с высоким уровнем коморбидности (≥3 баллов).
Тяжесть ВП оценивали при помощи шкалы CRB-65, которая включает следующие параметры (1 параметр – 1 балл): наличие признаков нарушения сознания (С), частота дыхания ≥30 в минуту (R); САД <90 или ДАД ≤ 60 мм рт.ст. (B); возраст ≥65 лет (65). Оценка 0 баллов соответствует нетяжелому течению ВП, требующему амбулаторного лечения; при 1–2 баллах пациент нуждается в стационарном наблюдении и оценке; при 3–4 баллах необходима неотложная госпитализация в отделение реанимации и интенсивной терапии [7].
Статистическая обработка данных проводилась в среде Statistica 13.0 (№ лицензии JPZ904I805602ARCN25ACD-6). Характер распределения в полученных выборках оценивали с помощью критериев Колмогорова–Смирнова, Шапиро–Уилка. Данные представлены в виде медианы, 25 и 75%. Значимость различий выборок оценивали посредством U-критерия Манна–Уитни. Значимость различий частот определяли с помощью критерия χ2 Пирсона. Взаимосвязи признаков оценивали через коэффициент корреляции R-Спирмена. Различия и ассоциации признавали статистически значимыми при достижении уровня доверительной вероятности p <0,05. Данные в таблицах представлены в виде медиан, 25 и 75%.
РЕЗУЛЬТАТЫ
 В исследованной выборке из 213 человек медиана возраста пациентов составила 43 (31÷63) года.
В исследованной выборке из 213 человек медиана возраста пациентов составила 43 (31÷63) года.
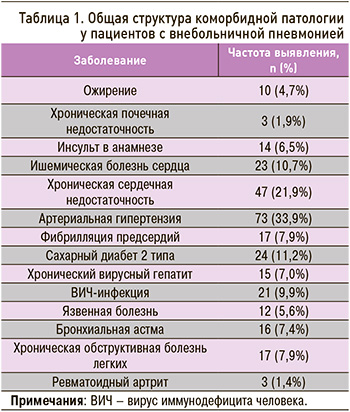
Было выявлено, что в общей структуре коморбидности первое место по распространенности занимала патология сердечно-сосудистой системы (74,4%), причем чаще встречались артериальная гипертензия (АГ) (33,9%) и ХСН (21,9%), второе – анемия (15%), третье – СД 2 типа (11,2%) и ВИЧ-инфекция (9,9%) (табл. 1).
При оценке коморбидности медиана ИЧ составила 2 (0÷6) балла. В группы пациентов с умеренной и высокой коморбидностью вошли 117 и 96 человек соответственно. Среди пациентов с высокой коморбидностью заболевания сердечно-сосудистой системы (АГ, ИБС, ФП, ХСН), СД 2 типа, ХОБЛ, ХПН, ревматоидный артрит встречались значимо чаще, чем у пациентов с умеренной коморбидностью. Все случаи аутоиммунных заболеваний, ВИЧ-инфекции и хронического вирусного гепатита С относились к группе высокоморбидных, при этом у пациентов с умеренной коморбидностью чаще имели место ранее перенесенные и текущие ОРВИ. Также необходимо отметить, что, помимо различий по частоте сопутствующих заболеваний, все пациенты с осложненным ассоциированным событиями течением сердечно-сосудистых заболеваний однозначно относились к группе высокой коморбидности. Также во всех случаях только к группе с высоким уровнем коморбидности могли быть отнесены пациенты, хронически употребляющие алкоголь и наркотические вещества (табл. 2).
Таким образом, наличие в анамнезе любого из указанных выше состояний может ассоциироваться с высокой коморбидностью, а значит, и с увеличением риска неблагоприятного исхода ВП [3].
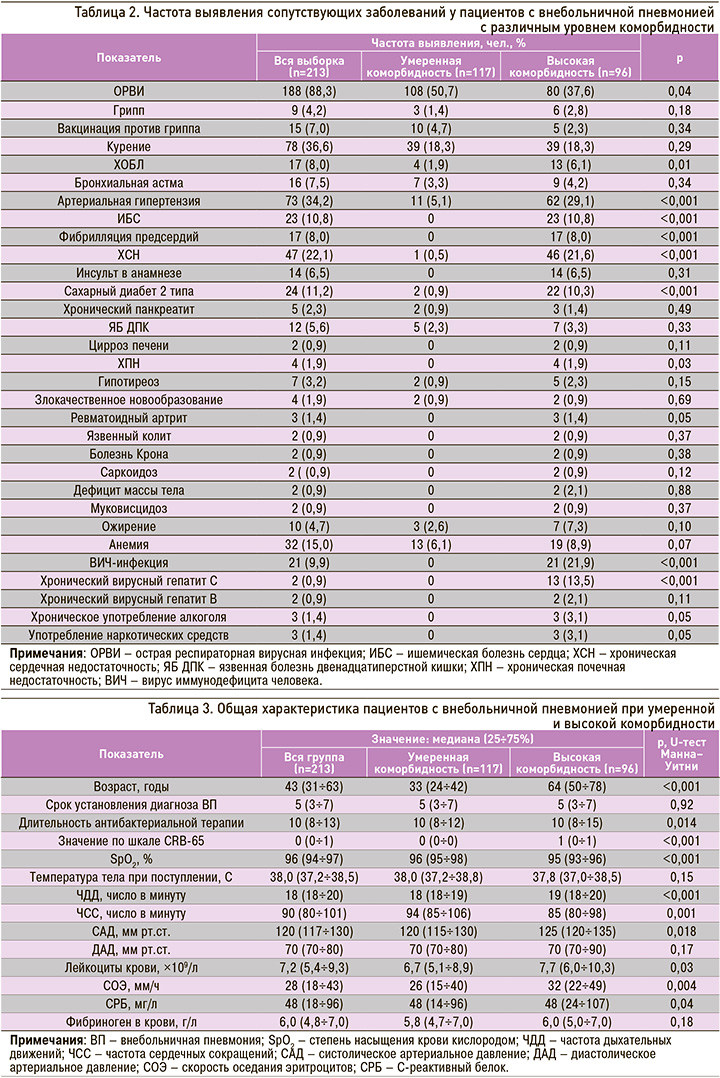
Пациенты с высокой коморбидностью ожидаемо были значительно старше пациентов с умеренной коморбидностью, имели более низкие показатели сатурации и более высокие значения ЧДД, САД, уровней лейкоцитов, скорости оседания эритроцитов и C-реактивного белка (СРБ) в крови. У пациентов с умеренной коморбидностью чаще наблюдалась тахикардия при госпитализации, но длительность антибактериальной терапии была меньше (табл. 3).
При оценке по шкале CRB-65 141 (66,2%) госпитализированный набрали 0 баллов, 56 (26,3%) – 1 балл, 14 (6,6%) – 2 балла, 2 (0,9%) – 3 балла. Таким образом, большинство пациентов (92,5%) соответствовало нетяжелому течению пневмонии (0–1 балл), при котором возможно лечение в амбулаторных условиях. Однако среди набравших 0 баллов по шкале CRB-65 было 102 человека с умеренным и 39 человек с высоким уровнем коморбидности; среди тех, кто набрал 1 балл, – 14 и 42 пациента соответственно, 2 балла – 13 пациентов с высоким уровнем коморбидности и только один с умеренной коморбидностью, 3 балла – 2 пациента с высокой коморбидностью.
При бактериологическом исследовании мокроты возбудитель выделен только у 58 (27,2%) пациентов. Как видно из рисунка, у пациентов с ВП и высокой коморбидностью, в отличие от пациентов с умеренной коморбидностью, наряду с другими возбудителями встречались резистентные стафилококки (MRSA, MRSE) и грибы рода Candida.

ОБСУЖДЕНИЕ
Наличие коморбидности – один из неблагоприятных факторов, влияющих на течение и прогноз пневмонии [3]. Основными особенностями течения заболевания, создающими трудности ведения этой категории пациентов, являются частая декомпенсация сопутствующей патологии на фоне пневмонии, риск плохого ответа на антибактериальную терапию, вероятность антибиотикорезистентности, нарушенная фармакокинетика антибактериальных препаратов (АБП), риск лекарственных взаимодействий, частота побочных эффектов. Кроме того, сопутствующая патология с функциональными нарушениями со стороны печени и почек создает определенные сложности и может становиться источником ошибок в выборе АБП, его дозировках, путях введения, длительности антибактериальной терапии и т.д. При этом в основе ошибок может лежать либо недиагностированная сопутствующая патология, либо недостаточная оценка риска токсического эффекта АБП, либо недостаточное знание фармакокинетических особенностей назначаемого АБП [13].
В нашем исследовании выявлено, что длительность антибактериальной терапии была выше у пациентов с высокой коморбидностью. При этом в других исследованиях было показано, что короткие курсы антимикробной терапии при высоком уровне клинической эффективности обладают рядом преимуществ, к числу которых относятся повышение комплаентности терапии и, как следствие этого, высокая клиническая эффективность; снижение общей стоимости лечения за счет уменьшения расходов на антибиотик и его введение, возможности более ранней выписки из стационара; уменьшение частоты развития нежелательных явлений; снижение риска возникновения антибиотикорезистентных штаммов микроорганизмов [14].
В представленном исследовании у госпитализированных по поводу ВП и в большей степени у пациентов с высокой коморбидностью наиболее часто встречались заболевания сердечно-сосудистой системы. Сочетание ХСН и ВП выступает крайне неблагоприятным фактором, взаимно отягощающим течение обоих заболеваний, особенно у пациентов старших возрастных групп. ХСН – независимый предиктор летального исхода при ВП [15, 16].
Смертность от ВП выше у пожилых пациентов с отягощенным преморбидным фоном (истощение, курение, злоупотребление алкоголем) и тяжелой сопутствующей патологией (ХОБЛ, ХСН, ХБП, СД, онкологические заболевания и др.) [17]. ХСН повышает риск летального исхода ВП в течение 30 дней, причем этот риск прямо коррелирует со степенью тяжести ХСН. В ряде исследований у больных ХСН вероятность госпитализации по поводу ВП была в 2 раза выше, чем у участников без подобной коморбидности. Кроме того, у лиц с хроническими нарушениями легочной функции и/ или сердечно-сосудистыми заболеваниями выявлена угроза респираторных и сердечно-сосудистых осложнений ВП, причем оба эти фактора связаны с повышенной смертностью [18].
Нами отмечена высокая частота анемии у пациентов с ВП, что не противоречит данным других исследований. В последнее время исследователи все чаще подчеркивают ассоциацию ВП с анемией, которая вносит вклад в тяжесть течения ВП и летальность от этого заболевания [19, 20]. Согласно данным исследований, до 30% заболевших ВП страдали анемией, что влияет на неблагоприятный прогноз, повышая смертность среди таких пациентов [20]. Также анемии при ВП на фоне ХОБЛ, ХСН или хронической болезни почек (ХБП) ухудшают прогноз и требуют лечения в стационаре [17]. В исследованиях было показано, что среди пациентов без сопутствующих заболеваний, а также у больных с нетяжелым течением ВП анемия в течение периода госпитализации встречалась довольно часто (около 55% пациентов) [19]. По данным Doshi S. et al., из 347 больных ВП анемия с уровнем гемоглобина ниже 100 г/л была выявлена у 10,1%; при этом 125 больных страдали ХОБЛ. Средний уровень гемоглобина у больных ВП без наличия ХОБЛ был выше и составлял около 124 г/л [17, 20].
На третьем месте по частоте коморбидных заболеваний у пациентов с ВП в нашем исследовании оказался СД 2 типа, причем чаще он встречался при высокой коморбидности. По результатам исследований, ВП у пациентов с СД 2 типа относятся к числу наиболее распространенных острых инфекционных заболеваний, причем в этом случае наблюдается более тяжелое течение пневмонии, частое развитие осложнений и высокие показатели летальности [21]. Наличие ХОБЛ и СД является значимым предиктором госпитализации пациентов с ВП [18]
По нашим данным, наличие ВИЧ-инфекции было характерно только для пациентов с высоким уровнем коморбидности. Согласно исследованиям, заболеваемость бактериальной пневмонией у инфицированных ВИЧ в 5–10 раз превышает показатель в популяции. Наиболее значимыми факторами риска развития ВП признаны употребление наркотиков, табакокурение, ВИЧ-ассоциированная иммуносупрессия, цирроз печени и отсутствие антиретровирусной терапии или перерывы в лечении. Развитие тяжелых, осложненных и инвазивных форм ВП и, как следствие, риск неблагоприятного исхода у больных с ВИЧ-инфекцией встречаются значительно чаще, чем среди населения в целом [22].
Как следует из ряда эпидемиологических исследований, ХОБЛ наиболее часто ассоциируется с пневмонией, что опять же не противоречит результатам нашего исследования. Заболеваемость ВП у больных с обострением ХОБЛ в 2 раза выше, чем у пациентов в общей популяции, а общее число случаев ВП составляет 55,5 на 1000 человеко-лет. Среди факторов риска развития ВП у больных ХОБЛ в первую очередь выделяют курение, оказывающее угнетающее влияние на различные звенья местной защиты легких (мукоцилиарный клиренс, клеточное и гуморальное звенья) [23]. В нашем исследования факт курения был установлен у трети пациентов с ВП. При этом вероятность развития ВП возрастает с увеличением стажа курения. В среднем курильщики имеют в 3,7 раза больше шансов заболеть ВП, чем некурящие. Так, по данным исследований, курящие пациенты, госпитализированные с ВП, имели 5-кратное увеличение риска смерти от пневмококковой ВП в течение 30 дней по сравнению с некурящими или отказавшимися от потребления табака больными [18].
В настоящем исследовании пациенты в группе высокой коморбидности имели более высокие значения СРБ. Многочисленные исследования подтверждают большую диагностическую значимость СРБ у больных с подозрением на ВП. Оценка этого показателя позволяет провести дифференциальный диагноз, оценку тяжести состояния и прогноза ранних и отдаленных осложнений, а также мониторировать, адекватность и эффективность проводимой антибактериальной терапии [24]. Пороговым значением концентрации СРБ, позволяющим отделить больных ВП от пациентов с обострением ХОБЛ, считают 33 мг/л (большее значение свидетельствует о пневмонии). У пациентов с БА при повышении уровня СРБ до 48 мг/л и более в сыворотке крови также с высокой вероятностью можно прогнозировать наличие ВП [25].
Нами было установлено, что пациенты с более тяжелой ВП (по оценке CRB-65) значимо чаще имели высокий уровень коморбидности, но среди лиц с легким течением большинство имели сопутствующую патологию, послужившую причиной госпитализации в стационар.
В ходе бактериологического исследования мокроты у пациентов с ВП были выявлены как грамположительные, так и грамотрицательные возбудители, а также резистентные штаммы в группе высокой коморбидности. Наиболее частым возбудителем ВП был S. pneumonia; по данным других авторов, на его долю приходится до 30–50% случаев ВП установленной этиологии [26, 27]. Коморбидные пациенты относятся к группам высокого риска инвазивных пневмококковых инфекций [28]. В соответствии с данными исследований, этиологическая структура ВП у лиц с сопутствующими заболеваниями, которые оказывают влияние на ее этиологию, а также служат факторами риска неблагоприятного прогноза, отличается большим разнообразием. У больных нетяжелой ВП, принимавших в последние 3 мес антибактериальные препараты и/или имеющих сопутствующую патологию (ХОБЛ, СД, ХСН, ХПН, заболевания печени, алкоголизм, наркомания, дефицит массы тела), помимо S. pneumoniae и Chlamydia pneumoniae, возрастает роль таких возбудителей, как Hemophilus influenzae, S. aureus и K. pneumoniae, в том числе штаммов, обладающих механизмами антибиотикорезистентности. У пациентов с ВП тяжелого течения в этиологии заболевания основное место занимают пневмококки, S. aureus, Hemophilus influenzae, грамотрицательные энтеробактерии и Legionella species (spp.). Исследования, проведенные в Европе, свидетельствуют, что в 4–7% случаев при тяжелой ВП обнаруживают P. aeruginosa, Coxiella burnetii и в 3% – респираторные вирусы [29].
Ранее было показано, что развитие ВП у лиц с хроническим бронхитом ассоциировалось с выявлением следующих сочетаний микробных агентов: Streptococcus pyogenes (S. pyogenes) + Candida spp.; S. pyogenes + K. pneumoniae; S. pyogenes + Enterobacter, S. pyogenes + P. aeruginosa, S. pyogenes + Acinetobacter, S. pyogenes + S. aureus, S. pneumoniae + S. aureus. При наличии у пациентов наркотической зависимости обнаружено сочетание S. pyogenes + P. aeruginosa. У лиц с ВП, злоупотребляющих алкоголем, встречаются следующие микробные ассоциации: S. pyogenes + Enterobacter spp., S. pyogenes + K. pneumoniae, E. coli + Candida spp., S. pneumoniae + P. aeruginosa, S. pyogenes + S. aureus, S. pneumoniae + S. aureus + Candida spp. На фоне ВИЧ-инфекции при ВП чаще, чем при нормальном иммунитете, выделяются S. aureus, M. catarrhalis, а на поздних стадиях еще и Pseudomonas spp. [30]. Этиология ВП у больных ХОБЛ чаще ассоциируется с S. pneumoniae, атипичными возбудителями, реже с грамотрицательными энтеробактериями. У этой группы пациентов выше вероятность выделения P. aeruginosa, чем у лиц без ХОБЛ [23].
В исследованиях больных ВП средней и легкой степени тяжести были выделены следующие ассоциации возбудителей: S. pyogenes + Candida spp., S. pyogenes + K. pneumoniae; E. coli + S. pyogenes; Streptococcus haemolyticus и E. coli + Candida spp.; S. pyogenes + P. aeruginosa; S. pneumoniae + Candida spp.; S. pneumoniae + P. aeruginosa, S. pyogenes + Acinetobacter spp.; S. pneumoniae + S. aureus + Candida spp.; при тяжелом течении ВП: S. pyogenes + S. aureus; S. pyogenes + S. aureus + E. coli; S. pyogenes + Kl. pneumoniae; S. pneumoniae + Citrobacter; S. pyogenes + Enterobacter spp.; S. haemolyticus [30]. Представленные данные говорят о необходимости учитывать особенности ВП с сочетанной патологией при назначении антибактериального лечения и проведении профилактических и противоэпидемических мероприятий.
Таким образом, ВП – патология, обладающая множеством системных эффектов, и коморбидный фон таких пациентов крайне отягощен. Наличие коморбидных состояний является фактором возникновения ВП и ее тяжелого течения, особенно у пожилых пациентов и в период эпидемии ОРВИ. С учетом частой коморбидности важно своевременное выявление и адекватная коррекция декомпенсации сопутствующей патологии, поскольку летальность у этой категории пациентов нередко обусловлена именно декомпенсацией коморбидных состояний.
ЗАКЛЮЧЕНИЕ
1. Заболевания сердечно-сосудистой системы, анемия, СД 2 типа и ВИЧ-инфекция преобладали в общей структуре коморбидности пациентов, госпитализированных в стационар в период эпидемии ОРВИ по поводу ВП.
2. Среди пациентов с ВП и высокой коморбидностью чаще встречались заболевания сердечно-сосудистой системы, а также СД 2 типа, ХОБЛ, ХПН, ревматоидный артрит, ВИЧ-инфекция и хронический вирусный гепатит С.
3. Пациенты с тяжелой ВП (по оценке CRB-65) значимо чаще имели высокий уровень коморбидности, но при этом подавляющее большинство пациентов с легким течением ВП страдало сопутствующей патологией, которая обусловила необходимость госпитализации в стационар круглосуточного пребывания.
4. В мокроте пациентов с ВП и высокой коморбидностью чаще выявлялись резистентные стафилококки и грибы рода Candida.



