Длительное прогрессирующее течение хронической сердечной недостаточности (ХСН), частые обострения и развитие осложнений нередко приводят к госпитализациям пациентов в стационарные лечебные учреждения. ХСН становится причиной более чем 1 млн госпитализаций ежегодно [1], несмотря на достижения в области фармакологии по созданию лекарственных препаратов, улучшающих клиническое состояние, качество жизни и замедляющих прогрессирование заболевания.
К сожалению, уровень смертности в результате ХСН, возникшей на этапе госпитализации пациентов, со временем не меняется: до 50% летальных исходов по-прежнему регистрируется на госпитальном этапе, несмотря на то что за период 1987–2008 гг. стандартизированный по возрасту коэффициент смертности снизился на 40% (с 54,2 до 32,6%), а средний возраст смерти увеличился с 80,0 до 82,7 лет [2].
Последние рекомендации мировых научных сообществ по ведению пациентов с сердечной недостаточностью, изложенная позиция экспертов фокусируют внимание на необходимости снижения бремени госпитализаций и повторных госпитализаций как одной из принципиальных задач в лечении пациентов с ХСН. Это обусловлено высоким уровнем летальности в ранний период после выписки из стационара (ранний постгоспитальный период) и повторных госпитализаций [3].
В связи с этим актуальным остается поиск факторов, ассоциированных с высоким риском госпитализаций пациентов пожилого возраста, имеющих в большинстве случаев сочетанную патологию и низкий уровень приверженности к назначениям лечащего врача.
Цель исследования – изучить факторы, связанные с госпитализацией по сердечно-сосудистым причинам больных ХСН в возрасте 60 лет и старше.
МАТЕРИАЛ И МЕТОДЫ
В открытое сравнительное нерандомизированное проспективное исследование было скринировано 310 пациентов с сердечно-сосудистой патологией. В исследовании приняли участие 80 пациентов в возрасте от 60 до 89 лет, у которых по результатам обследования была диагностирована ХСН.
Критерии включения:
- амбулаторные пациенты (мужчины и женщины);
- возраст 60 лет и старше;
- ХСН II–IV функционального класса (ФК) по классификации Нью-Йоркской ассоциации сердца, вследствие ишемической болезни сердца (ИБС) и/или артериальной гипертонии (АГ), диагностированная не менее 3 мес перед включением в исследование;
- отсутствие госпитализаций по поводу декомпенсации ХСН в течение предшествующих 3 мес.
Критерии исключения: острое нарушение мозгового кровообращения или острый инфаркт миокарда в течение последних 3 мес перед исследованием, гемодинамически значимые пороки клапанов сердца, гипертрофическая или дилатационная кардиомиопатия, инфекционный эндокардит.
Пациенты осматривались каждые 3–5 дней при подборе медикаментозной терапии, затем с частотой 1 раз в месяц в течение первых трех месяцев, 1 раз в 3 месяца на протяжении всего последующего периода наблюдения. После выписки из стационара в случае госпитализации пациенты наблюдались 2 раза в неделю в рамках очного приема или телефонного контакта. Лечение проводилось на фоне соблюдения пациентами водно-солевого режима, рекомендованного при ХСН.
Каждый пациент подписал информированное согласие на добровольное участие в исследовании. Исследование было принято к сведению Этическим комитетом при РНИМУ им. Н.И. Пирогова.
Диагноз ХСН подтверждался симптомами и/ или клиническими признаками (в покое или при физической нагрузке), объективными признаками дисфункции сердца (в покое), положительным ответом на терапию [4]. Функциональный статус пациентов оценивался с помощью классификации Нью-Йоркской ассоциации сердца. В качестве негативной конечной точки оценивались госпитализация по сердечно-сосудистым причинам (декомпенсация сердечной недостаточности, гипертонический криз, тромбоэмболия ветвей легочной артерии) и летальный исход.
Включение пациентов в исследование проводилось в период с сентября 2014 г. по декабрь 2017 г. в Диагностическом клиническом центре № 1 Департамента здравоохранения г. Москвы. Продолжительность наблюдения за пациентами составила 24,1±13,0 мес.
Ожирение определяли в соответствии с классификацией индекса массы тела (ИМТ) по ВОЗ: ИМТ 25–29,9 кг/м2 характеризовал избыточную массу тела, 30 кг/м2 и более – ожирение [5].
Минеральная плотность кости (МПК) определялась методом двухэнергетической рентгеновской абсорбциометрии (ДРА) на аппарате LunarProdigy (GeneralElectric, США). МПК исследовали в поясничном отделе позвоночника (L2–L4) и шейке бедренной кости. Костную массу оценивали по содержанию минералов на единицу площади костной ткани (г/см2), а также от среднего показателя пиковой костной массы молодых женщин (Т-критерий) в стандартных отклонениях (СО). Т-критерий –2,5 и ниже расценивали как остеопороз. При постановке диагноза «остеопороз» учитывались анамнестические данные и сопутствующие заболевания, способные влиять на показатели МПК [6].
Критерием анемии считали снижение уровня гемоглобина менее 130 г/л у мужчин и менее 120 г/л у женщин [7].
Скорость клубочковой фильтрации (СКФ) рассчитывалаcь по формуле CKD-EPI. Хроническую болезнь почек (ХБП) в соответствии с рекомендациями KDIGO-2012 диагностировали при уровне СКФ ниже 60 мл/мин/1,73 м2, который сохранялся на протяжении 3 мес и более даже в отсутствие других маркеров повреждения почек [8].
Биохимические показатели определяли на автоматическом биохимическом анализаторе Olympus 5800 (JP, Olympus Corporation, США) по стандартным методикам с использованием реагентов производителя на базе клинико-диагностической лаборатории Диагностического клинического центра № 1 Департамента здравоохранения г. Москвы. Концентрация N-концевого фрагмента мозгового натрийуретического пептида (NT-proBNP) в сыворотке крови оценивалась посредством электрохемилюминесцентного анализа с использованием специализированной тест-сиcтемы Roche (Германия) pro-BNP II Elecsys СobaseE.
Эхокардиографию (ЭхоКГ) проводили в двухмерном (В-режиме) и допплеровских режимах (импульсно-волновом и постоянно-волновом) на аппарате Vivid-3 (General Electric, США). При ЭхоКГ исследовании придерживались рекомендаций, предложенных Американской ассоциацией эхокардиографистов [9].
Статистическая обработка данных выполнялась с использованием пакетов программ SPSS 21.0 и Stata 15. Описательная статистика качественных переменных представлена в виде частот и процентов, непрерывных количественных данных – в виде среднего значения ± стандартного отклонения, при ненормальном распределении – в виде медианы и 25-й и 75-й перцентилей распределения значений показателя (межквартильный размах). Сравнение количественных признаков проводили по ранговому U-критерию Манна–Уитни, качественных – с применением таблиц сопряженности по критерию χ2 Пирсона с поправкой Йетса и точному критерию Фишера. Анализ выживаемости осуществлялся с помощью логарифмического рангового критерия для категориальных переменных и однофакторной регрессии Кокса для непрерывных переменных. По результатам однофакторного анализа разработана модель пропорциональных рисков (регрессия Кокса). Результаты представлены в виде отношений рисков (ОР; отношение моментных рисков). Визуализация модели выполнена с использованием кривых выживаемости. Различия считали статистически значимыми при значениях двустороннего p <0,05.
РЕЗУЛЬТАТЫ
За 24,1±13,0 мес наблюдения по сердечно-сосудистым причинам было госпитализировано 49 из 80 (61,3%) пациентов, которые составили основную группу. Повторные госпитализации произошли у 32 из 49 (65,3%) пациентов с ХСН. II ФК ХСН имелся у 23 (47%), III ФК – у 24 (49%), IVФК – у 2 (4%) больных. Пациенты, которым не потребовалась госпитализация (n=31), составили группу сравнения. II ФК ХСН был установлен у 28 (90%), III ФК – у 3 (10%) человек, при этом IV ФК отсутствовал в этой группе.
Среди госпитализированных пациентов чаще встречались пациенты с III ФК (р <0,001), среди не госпитализированных – II ФК (р <0,001). В основной группе фракция выброса левого желудочка (ФВ ЛЖ) менее 40%, по данным ЭхоКГ, отмечалась у 12 (25%), 40–49% – у 6 (12%), 50% и более – у 31 (63%) пациентов. В группе сравнения аналогичные показатели ФВ ЛЖ наблюдались у 2 (6%), 3 (9%) и 26 (85%) пациентов соответственно.
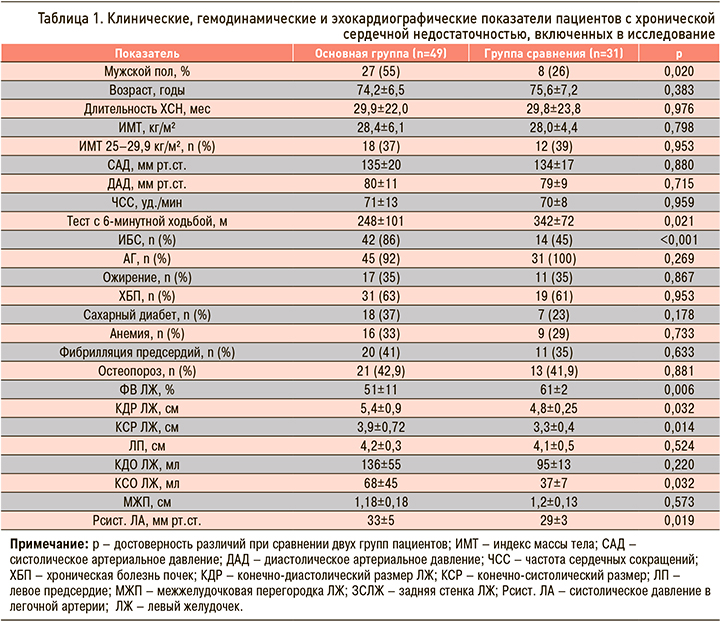
Среди 49 госпитализированных пациентов с ХСН сопутствующей патологией страдали 47 (96%), в группе сравнения – 27 (87%) пациентов. Среди сопутствующих заболеваний превалировали ХБП, ожирение и сахарный диабет (табл. 1).
Лабораторные показатели пациентов с ХСН и группы сравнения представлены в таблице 2.
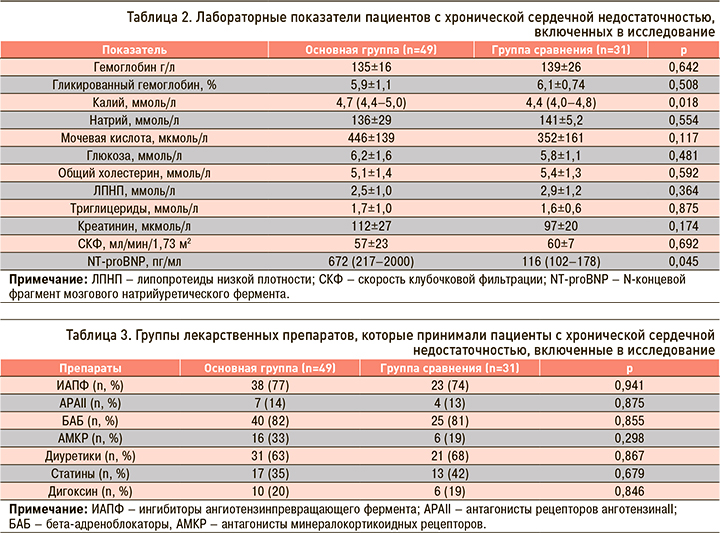
Пациенты двух групп исследования были сопоставимы по рекомендованному медикаментозному лечению (табл. 3).
При однофакторном анализе (регрессия Кокса) установлено, что риск госпитализаций при ХСН выше у мужчин (ОР 3,28; 95% ДИ 1,08–9,86; р=0,035), при результате теста с 6-минутной ходьбой 258 м и ниже (ОР 2,98; 95% ДИ 1,2–7,6; p=0,022) и ФВ ЛЖ 39% и ниже (ОР 0,9; 95%ДИ 0,88–0,98; p=0,007).
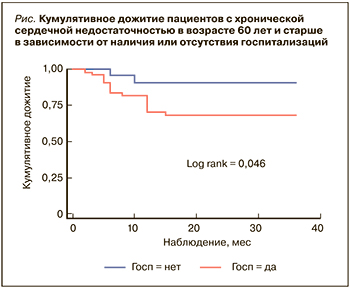 Наблюдалась худшая выживаемость пациентов с ХСН, которым потребовалась госпитализация за период наблюдения, по сравнению с пациентами, не госпитализированными в клиники (рис.).
Наблюдалась худшая выживаемость пациентов с ХСН, которым потребовалась госпитализация за период наблюдения, по сравнению с пациентами, не госпитализированными в клиники (рис.).
В группе пациентов с ХСН, имевших госпитализации, умерло 17 (34%), без госпитализаций – 2 (6%) пациентов (р=0,009). У всех больных причинами летального исхода оказались сердечно-сосудистые заболевания (инфаркт миокарда, тромбоэмболия легочной артерии, острая сердечная недостаточность). Госпитализации по сердечно-сосудистым причинам тесно ассоциировались с высокой летальностью пациентов (ОР 7,7; 95% ДИ 1,6–36,3; p=0,010).
ОБСУЖДЕНИЕ
В последние годы проводится множество исследований, изучающих особенности течения ХСН у лиц старшего возраста и факторы, связанные с госпитализациями пациентов. Это и стало предпосылкой для проведения исследования в реальной амбулаторной практике с целью идентификации пациентов с высоким риском госпитализаций.
Данные крупнейших мировых регистров подтверждают, что встречаемость ХСН нарастает по мере старения, а средний возраст пациентов с ХСН составляет около 70–75 лет [10]. Помимо этого, существует достаточно доказательств в пользу того, что старший возраст служит независимым предиктором неблагоприятного прогноза пациентов с ХСН [11].
Малосимптомное течение ХСН и сопутствующая патология в старшем возрасте скрывают основные проявления заболевания, включая симптомы, свидетельствующие о его прогрессировании. В связи с этим крайне необходимо раннее выявление лиц с высоким риском госпитализации. В этом контексте нельзя не сослаться на слова G. Rose [12], призывающего врачей ответственно и эффективно решать задачу выявления факторов риска.
Согласно полученным нами данным, в среднем за 2 года наблюдения были госпитализированы 61,3% пациентов с ХСН в возрасте 74 лет в связи с сердечно-сосудистыми причинами. В основном это были пациенты, имевшие ИБС, III–IV ФК ХСН, у каждого четвертого больного была низкая ФВ ЛЖ, у более чем половины (63%) – сохраненная ФВ ЛЖ. Госпитализированные пациенты имели более высокий уровень NT-proBNP, низкий уровень физической активности, более низкую ФВ ЛЖ и увеличенные размеры и объемы камер сердца по сравнению с пациентами, которые не нуждались в госпитализации. 96% госпитализированных страдали сопутствующими заболеваниями, у большинства негоспитализированных пациентов (87%) также наблюдалась мультиморбидность, при этом ее структура была сопоставима в обеих группах.
Наши результаты согласуются с данными других исследователей, согласно которым в стационар в основном поступают пациенты c ХСН, имеющие средний возраст 69 лет и более [13]. В основном это мужчины [14, 15], а сопутствующая патология предопределяет увеличение числа пациентов с более тяжелым течением ХСН [16, 17].
Благодаря существенным достижениям медицинской науки, постоянно пересматриваются и дополняются маркеры, ассоциированные с неблагоприятным прогнозом у пациентов с ХСН. Все больше внимания уделяется сопутствующей патологии как сердечно-сосудистого, так и не сердечно-сосудистого происхождения, госпитализациям, обусловленным декомпенсацией сердечной деятельности, а также биомаркерам [18]. В соответствии с нашими данными, риск госпитализаций при ХСН оказался выше у мужчин (ОР 3,28; р=0,035), при прохождении за 6 мин дистанции 258 метров и ниже (ОР 2,98; p=0,022), при ФВ ЛЖ 39% и ниже (ОР 0,9; p=0,007). При этом худшая выживаемость была отмечена среди лиц, которым потребовалась госпитализация за период наблюдения.
Польские исследователи, проанализировав причины высокой внутригоспитальной общей летальности, также выделили уязвимую категорию, к которой отнесли лиц мужского пола и старшего возраста. Cогласно полученным данным, средний уровень внутригоспитальной летальности составил 4,1%, летальность среди женщин – 3,62%, среди мужчин – 4,74%. Женский пол ассоциировался с более низким уровнем летальности по сравнению с мужским (OР 0,79; р <0,001) [19].
Ретроспективный наблюдательный анализ 718 пациентов, госпитализированных в связи с декомпенсацией ХСН, показал, что через 4 года наблюдения общая смертность в группе мужчин составила 65,5%, в группе женщин – 48,1%, а медианы дожития – 720 и 1168 дней соответственно. Старший возраст оказался предиктором неблагоприятного прогноза и у мужчин, и у женщин (ОР 1,04; p <0,001) [20].
Риск летального исхода пациентов зависит не только от числа госпитализаций, но и от повторных госпитализаций, что подтверждено многими исследователями [13], в том числе и нашим наблюдением: 65,3% пациентов старшего возраста с ХСН неоднократно госпитализировались в клиники, а госпитализации по сердечно-сосудистым причинам тесно ассоциировались с высокой летальностью пациентов (ОР 7,7; p=0,010).
Уязвимая фаза начинается с момента выписки пациента из стационара, когда риск возникновения смерти или повторной госпитализации максимальный и длится от нескольких дней до нескольких недель [21, 22].
Rossello X. et al. рассматривают в качестве уязвимой группы пациентов в возрасте 85 лет и старше лиц, имеющих гериатрические синдромы, а также пациентов, которые были выписаны из стационара в течение 2 предшествующих недель [23].
В последнее время предложено выделять 3 фазы в течении ХСН: фаза инициации, фаза плато и фаза паллиативного ухода, что обусловлено необходимостью своевременной разработки тактики лечения и наблюдения за пациентами с целью снижения риска госпитализаций, в том числе и повторных, и связанной с ней летальностью. Истинная природа сердечной недостаточности представляет собой хронологическую прогрессию ремоделирования ЛЖ, что проявляется клиническими симптомами, физическими страданиями и нередко преждевременной смертью. Госпитализации при ХСН негативно влияют именно на фазу инициации и паллиативную фазу. Переход к более выраженной фазе зависит от уровня восстановления (увеличение ФВ ЛЖ от 5 до 15%) и нормализации функции ЛЖ (ФВ ЛЖ ≥50%), а также качества скрининга пациентов с ХСН, начала лечения и исходного клинического состояния пациента [24]. Следовательно, для снижения риска летальности жизненно необходимым является не только выявление факторов риска госпитализаций, но и пристальное наблюдение за пациентами на протяжении 1–2 нед после выписки из стационара [25].
ЗАКЛЮЧЕНИЕ
За двухлетний период наблюдения было госпитализировано 61,3% амбулаторных пациентов с ХСН, средний возраст которых составил 74 года. В основном это были пациенты с III–IV ФК ХСН, у каждого четвертого отмечалась низкая ФВ ЛЖ, у 63% – сохраненная ФВ ЛЖ. Среди госпитализированных пациентов превалировали лица мужского пола. Госпитализированные пациенты имели более высокий уровень NT-proBNP, низкий уровень физической активности, более низкую ФВ ЛЖ и увеличенные размеры и объемы камер сердца по сравнению с пациентами, которые не нуждались в госпитализации. У 96% госпитализированных больных выявлена сопутствующая патология сердечно-сосудистого и иного происхождения. Мужской пол, дистанция, равная 258 м и менее, пройденная за 6 мин, низкая ФВ ЛЖ оказались факторами, ассоциированными с высоким риском госпитализаций. Полученные нами данные подтвердили, что 65,3% амбулаторных пациентов старшего возраста с ХСН повторно госпитализируются в клиники, а госпитализации по сердечно-сосудистым причинам тесно ассоциированы с высокой летальностью пациентов.
Результаты исследования подтверждают необходимость пристального контроля за клиническим состоянием и наблюдением за пациентами на протяжении первых недель после выписки из стационара, особенно имеющими высокий ФК ХСН, низкую ФВ ЛЖ и сниженную переносимость физических нагрузок.