ВВЕДЕНИЕ
Вирусные инфекции верхнего респираторного тракта – одна из наиболее частых причин нарушения вкуса и обоняния [1]. 11 марта 2020 г. Всемирная организация здравоохранения (ВОЗ) охарактеризовала распространение вируса SARS-CoV-2, вызывающего тяжелую острую респираторную инфекцию – COVID-19, как первую пандемию, связанную с коронавирусом. С увеличением числа зараженных стало поступать больше информации о том, что больные COVID-19 испытывают различные нарушения обоняния и вкуса, при этом подобные нарушения чаще выявлялись у пациентов с легкой формой заболевания [2]. Полагают, что механизм развития нарушений вкуса и обоняния у больных с COVID-19 отличен от того, который развивается при сезонных ОРВИ, и в первую очередь обусловлен поражением нервной системы [3]. В ряде исследований обнаружено, что различные степени обонятельной дисфункции встречаются в 9 из 10 случаев вне зависимости от наличия назальной обструкции [4]. Длительность симптомов имеет широкую вариабельность – от нескольких дней до нескольких месяцев и более.
Таким образом, обонятельная и вкусовая дисфункция – наиболее частые симптомы инфицирования SARS-CoV-2, наряду с классическими симптомами COVID-19 – лихорадкой, непродуктивным кашлем, одышкой [5].
Помимо данных об аносмии и гипосмии, растет число сообщений о паросмии у пациентов, перенесших инфекцию преимущественно в легкой или бессимптомной форме [6].
Цель исследования – оценить характер нарушений обоняния и вкуса, ассоциированных с COVID-19, и их связь с клиническими особенностями заболевания.
МАТЕРИАЛ И МЕТОДЫ
В период с 19.09.2020 по 01.03.2021 посредством онлайн-платформы Google Forms на условиях добровольного согласия был проведен опрос 10 348 пациентов по специально разработанной анкете, включающей 20 вопросов. Доступ к результатам исследования имели только авторы исследования, опрос проводился однократно.
Участникам было предложено пройти опрос без вознаграждения за участие. Данные проверены на повторяющиеся ответы, исключены потенциальные дубликаты и некорректно заполненные пункты, не поддающиеся обработке.
Критериями включения в исследование были наличие добровольного информированного согласия, диагноз COVID-19, верифицированный с помощью полимеразной цепной реакции (ПЦР), иммуноферментного анализа (ИФА) или иммунохроматографического метода и перенесенный более 1 мес назад, возникновение нарушений обоняния и вкуса.
К критериям невключения относились отсутствие добровольного информированного согласия, отсутствие верификации SARSnCOV2, наличие нарушений обоняния и вкуса до заболевания COVID-19.
Полученная выборка была разделена на 3 группы в зависимости от тяжести течения заболевания согласно 11 версии временных методических рекомендаций «Профилактика, диагностика и лечение новой коронавирусной инфекции (COVID-19)» от 07.05.2021, принятой Минздравом России [7]:
- группа 1 – легкое течение;
- группа 2 – среднетяжелое течение;
- группа 3 – тяжелое течение.
Статистическая обработка данных проводилась в среде Statistica 13.0 (№ лицензии JPZ904I805602ARCN25ACD-6). Данные представлены в виде медианы и 25÷75%. Значимость различий выборок оценивалась с помощью критерия Краскала–Уоллиса, различий частот – с помощью критерия χ2 Пирсона. Различия считали значимыми при значениях р <0,05.
Протокол исследования был одобрен локальным этическим комитетом ФГБОУ ВО «Уральский государственный медицинский университет» Минздрава России на заседании № 6 от 18.09.2020. Пациенты включались в исследование на условиях добровольного информированного согласия.
РЕЗУЛЬТАТЫ
В исследование вошло 10 348 пациентов – 7964 (77%) женщины и 2384 (23%) мужчины. Возраст женщин составил 29 (24÷36) лет, мужчин – 29 (24÷34) лет.
Легкую степень тяжести заболевания имели 8454 (81,6%) респондента, среднюю – 1486 (14,4%), еще 408 (4%) человек перенесли новую коронавирусную инфекцию, осложненную двухсторонним полисегментарным поражением легочной ткани.
Полное отсутствие вкуса и обоняния (аносмию и агевзию) имело место у 7225 (69,8%) респондентов, 2641 (25,5%) отмечали только полное отсутствие обоняния (аносмию), 78 (0,7%) – отсутствие вкусовых ощущений (агевзию) при сохранении обоняния.
Выявлены значимые различия частоты нарушений вкуса и обоняния у больных COVID-19 в зависимости от тяжести заболевания (χ2 =33,5; df=14; p=0,002), отраженные на рисунке 1.
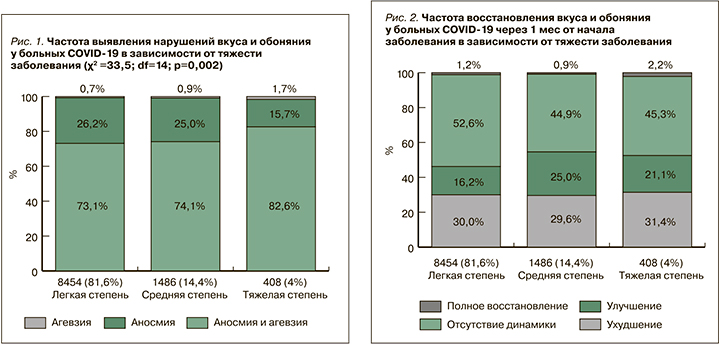
Спустя 1 мес от начала заболевания 3114 пациентов сообщили о прогрессирующем ухудшении обоняния и вкуса, 1736 пациентов – об улучшении обоняния, 5358 пациентов не отметили какой-либо динамики ощущений (рис. 2).
Выявлены значимые различия частоты восстановления вкуса и обоняния у больных COVID-19 в зависимости от тяжести заболевания (χ2 =39,33; df=14; p=0,001; см. рис. 2).
Не соблюдали меры самоизоляции и не использовали средства индивидуальной защиты (СИЗ) органов дыхания до заболевания 534 респондента, 1841 респондент работали в привычном режиме с использованием СИЗ, 7846 человек работали дистанционно и применяли СИЗ при посещении общественных мест. 122 пациента предпочли не отвечать на этот вопрос.
Установлены значимые различия в частоте восстановления вкуса и обоняния у больных COVID- 19 в зависимости от соблюдения мер предосторожности (χ2=6312,69; df=3246; p <0,001; рис. 3).

Значимые различия были обнаружены и при сравнении частоты восстановления вкуса и обоняния у больных COVID-19 в зависимости от тяжести заболевания (χ2=3584,37; df=42; p <0,001; рис. 4).
ОБСУЖДЕНИЕ
Полученные нами результаты в целом согласуются с наблюдениями в других популяциях и возрастных группах. Так, в когортном исследовании Женевского университета на протяжении 7–9 мес наблюдали 629 пациентов, среди которых аносмия и дисгевзия встречались в 16,8% случаев, являясь вторым по частоте обнаружения симптомом после общей слабости. Более чем у трети (37%) участников обсуждаемого исследования аносмия и ряд других симптомов сохранялись через 30–45 дней с начала заболевания, а у 19% процентов эти симптомы выявлялись и на 7–9-м месяце наблюдения. В метаанализе 15 исследований у 80% пациентов в возрасте от 17 до 87 лет в периоде реконвалесценции выявлялся как минимум 1 из следующих симптомов: утомляемость, нарушение обоняния и/или вкуса, нарушение внимания, выпадение волос и одышка.
Связь между потерей обоняния и заболеванием COVID-19 была установлена в когортном исследовании 10 069 человек через 4 нед после начала эпидемии COVID-19 [10].
Среди лиц молодого возраста (18–44 лет) аносмия в значительной части случаев является первым или единственным симптомом COVID-19 [11].
Также 86% из 417 пациентов с легкой и средней формой COVID-19 (верифицированного методом ПЦР) имели аносмию и 88% дисгевзию [12, 13].
В мультицентровом исследовании 417 пациентов с легкой и среднетяжелой формами COVID-19 наиболее часто отмечались следующие симптомы: кашель, миалгия и потеря аппетита. При этом 85,6 и 88,0% пациентов сообщили о дисфункции обоняния и вкуса соответственно. В 11,8% случаев обонятельная дисфункция была первым симптомом заболевания, у 44,0% обоняние восстановилось в первый месяц наблюдения. Обонятельная дисфункция среди женщин выявлялась статистически значимо чаще [4].
Согласно результатам многоцентрового исследования, в которое были включены 1363 пациента из 18 медицинских центров Европы, у 328 участников (24,1%) обоняние субъективно не восстановилось через 60 дней после начала дисфункции, а средняя продолжительность обонятельной дисфункции составила 21,6±17,9 дней. При использовании объективных исследований гипосмию/аносмию выявляли у 54,7% пациентов с легкой тяжестью COVID- 19 и 36,6% пациентов с легкой и средней тяжестью заболевания. Через 60 дней наблюдения обоняние не восстановилось у 15,3%, через 6 мес – у 4,7% пациентов с аносмией/гипосмией. Более высокая исходная тяжесть объективных обонятельных оценок в значительной степени предсказывала стойкую обонятельную дисфункцию [14].
В нашем исследовании достаточно большой массив данных позволил получить аргументы в пользу применения СИЗ, позволяющих снизить вероятность и массивность инфицирования воздушно-капельным путем [15].
Немало вопросов вызывает тактика ведения пациентов с обонятельной дисфункцией. Согласно систематическому обзору 20 публикаций, посвященных восстановлению обонятельной функции у перенесших COVID-19, комбинированное применение инъекции стероидов и введение назального спрея с глюкокортикоидами в носовую полость значительно улучшало обонятельную функцию у пациентов с поствирусной обонятельной дисфункцией [16]. В обзоре 36 исследований авторами сделан вывод о том, что краткосрочное использование системных и/или местных стероидов не оправданно; при этом они, однако, подчеркивают ограниченность информации [17, 18].
Продолжительное лечение, использование различных запахов и различных методик обонятельных тренировок, применение молекулярных запахов и разных концентраций одорантов увеличивают эффективность обонятельных тренировок. Максимальный эффект от вышеописанных методик достигался в период с 24-ю по 36-ю неделю [16, 19].
Добавление к обонятельным тренировкам топической или системной терапии низкими дозами глюкокортикоидов повышало эффективность терапии [16, 19].
При этом на сегодня большинство исследователей приходит к заключению, что прогноз по восстановлению обонятельной функции не коррелирует с клинико-лабораторными данными [17, 18]. Несмотря на относительно высокие показатели субъективного восстановления обоняния, необходимо проводить объективную оценку его восстановления.
Определенными ограничениями нашего исследования можно считать отсутствие прямого контакта исследователей с респондентами: из-за этого в соблюдение критериев включения и исключения было прерогативой самих респондентов, и отсутствовала возможность формирования группы контроля. Наряду с этим объективная стандартизированная оценка нарушенных функций в динамике также могла внести определенные коррективы в полученные результаты [14, 17, 18]. В то же время оценка исходов заболевания самими пациентами в настоящее время рассматривается как обязательный элемент определения эффективности и безопасности любых медицинских вмешательств, а также качества оказания медицинской помощи [20, 21]. Кроме того, возможность оперативного получения больших выборок однородных данных позволяет минимизировать влияние случайных ошибок на итоговую оценку результатов исследования и использовать их для оптимизации тактики профилактики, лечения и реабилитации пациентов с коронавирусной инфекцией [22].
ЗАКЛЮЧЕНИЕ
1. Развитие нарушений вкусовых и обонятельных ощущений у молодых пациентов с COVID- 19 ассоциировано с тяжестью заболевания: лица с тяжелым течением заболевания чаще отмечали одновременное нарушение вкуса и обоняния, пациенты с легкой и средней тяжестью чаще имели нарушение обоняния при сохраненном вкусе.
2. Через месяц от начала заболевания легкой степени у каждого второго пациента сохранялись аносмия и агевзия. Среди пациентов со средней и тяжелой формой COVID-19 чаще выявлялось восстановление вкуса и обоняния.
3. Темпы восстановления вкуса и обоняния у молодых пациентов с COVID-19 ассоциированы с тяжестью заболевания и соблюдением мер самоизоляции.


