ВВЕДЕНИЕ
Термин «спондилоартриты» (СпА) объединяет группу хронических воспалительных заболеваний, включающих анкилозирующий спондилит (АС), псориатический артрит, артрит/спондилит, связанный с воспалительными заболеваниями кишечника (ВЗК), реактивный артрит и характеризующихся общими клиническими, визуализационными и генетическими особенностями [1]. Поздняя диагностика СпА, обусловленная отсутствием патогномоничных клинических проявлений и лабораторных тестов, а также медленным развитием структурных изменений в осевом скелете, сопровождается отсрочкой лечения и, как следствие, увеличением структурных повреждений и выраженных функциональных нарушений, стойкой потерей трудоспособности лиц молодого возраста, возрастанием прямых и косвенных затрат на оказание медицинской помощи таким пациентам [2, 3].
Необходимость в раннем выявлении и лечении СпА привела к пересмотру их концепции и разработке новых классификационных критериев, в соответствии с которыми данные заболевания разделяют на преимущественно аксиальные и преимущественно периферические СпА. Кардинальным признаком аксиального СпА (аксСпА) является хроническая боль в спине, тогда как периферического СпА – артрит, энтезит и дактилит [4].
Спектр аксСпА охватывает пациентов с АС и нерентгенологическим аксСпА, основное отличие которых заключается в наличии или отсутствии рентгенологических признаков достоверного сакроилеита [5]. АксСпА представляет собой сложное заболевание с многообразными проявлениями, знание которых имеет решающее значение для своевременного выявления и направления больных к ревматологу.
КЛИНИЧЕСКИЕ ПРОЯВЛЕНИЯ АКСИАЛЬНОГО СПОНДИЛОАРТРИТА
Боль в пояснице – одна из распространенных проблем со здоровьем, которую в различные моменты своей жизни испытывают 50–80% взрослых [6]. Считается, что взрослые трудоспособного возраста наиболее уязвимы в отношении появления боли в нижней части спины, являющейся самой частой причиной инвалидности во всем мире [7]. Частота хронической боли в спине среди лиц 20–59 лет составляет 20%. Распространенность АС и в целом аксСпА оценивается в пределах 0,01–0,54 и 0,13–1,40% соответственно, а их встречаемость в первичном звене медико-санитарной помощи среди лиц с хронической болью в спине – в пределах 5–24% [3].
Боль в спине длительностью 3 и более мес с возрастом начала <45 лет – ключевой признак, необходимый для скрининга пациентов с подозрением на аксСпА, отражающий наличие воспаления в крестцово-подвздошных суставах и/или позвоночнике. В 75–85% случаев она выступает ведущим клиническим симптомом в дебюте этого заболевания [8, 9]. Для диагностики воспалительной боли в спине (ВБС) в настоящее время используют критерии экспертов ASAS [10], согласно которым боль в спине считается воспалительной, если присутствуют любые 4 из 5 параметров:
- начало в возрасте до 40 лет;
- постепенное начало;
- улучшение (уменьшение боли в спине) после физических упражнений;
- отсутствие улучшения после отдыха;
- ночная боль (с улучшением после пробуждения).
Выявление ВБС должно основываться на результатах целенаправленного опроса пациента и правильной интерпретации ее особенностей. Для нее характерно постепенное (в течение нескольких недель или месяцев) нарастание интенсивности боли в спине, часто без четкого указания на провоцирующие факторы. Отличительной чертой ВБС является уменьшение выраженности при обычной физической активности (это может быть лечебная гимнастика, ходьба), но не при отдыхе. Однако, как и при неспецифической боли в спине, усиление боли может происходить при чрезмерной физической нагрузке, а также длительных периодах обездвиживания, пребывании в статической позе. Наличие ночной боли с улучшением после пробуждения, которая чаще встречается у больных с высокой активностью заболевания, имеет большое значение для подтверждения ВБС: пациенты просыпаются из-за боли во второй половине ночи, преимущественно в ранние утренние часы, а когда начинают двигаться, выраженность этого симптома ослабевает [9, 11].
При описании клинических проявлений многие пациенты с аксСпА сообщают о боли в ягодицах, которая нередко иррадиирует в бедро до коленного сустава, возникает попеременно то с одной, то с другой стороны, со временем становится стойкой и двусторонней. Наличие этого признака отражает как процессы формирования сакроилеита, так и выраженные деструктивные изменения в крестцово-подвздошных суставах. Определение перемежающей боли в ягодицах особенно помогает при отсутствии симптомов ВБС, перечисленных в критериях экспертов ASAS [11].
Утренняя скованность, воспринимаемая пациентами как ощущение тугоподвижности в позвоночнике, не является диагностически значимой для ВБС, поскольку встречается практически с одинаковой частотой при неспецифической или механической боли в спине. Однако длительность утренней скованности имеет большое значение в оценке активности аксСпА: чем дольше она длится и больше выражена, тем активнее заболевание [11].
Обсуждая ВБС как критерий, позволяющий определять среди пациентов с хронической болью в спине тех, которые потенциально могут страдать аксСпА, следует обратить внимание на то, что ее выявление не эквивалентно установлению диагноза. Было показано, что только 70–80% больных аксСпА имеют типичные симптомы ВБС [3]. Поэтому при принятии окончательного решения, служит ли боль в спине проявлением ревматического заболевания или нет, надо учитывать и другие клинические признаки болезни, а также данные лабораторно-инструментальных методов обследования.
Помимо ВБС, к характерным клиническим чертам аксСпА относятся периферический артрит, энтезит и дактилит. Приблизительно у 30% пациентов наблюдается асимметричный олигоартрит, который в основном поражает суставы нижних конечностей. Однако нередко воспаление возникает в других суставах: грудино-ключичных, акромиально-ключичных, синхондрозе рукоятки грудины. Периферический артрит несколько чаще встречается у женщин [9].
Энтезит – воспаление мест прикрепления суставной капсулы, связок или сухожилий к кости, представляет собой одно из основных проявлений всей группы СпА, включая аксСпА. Клинически он выражается болью, возникающей при сопротивлении активному движению (напряжении) заинтересованной мышцы, локальной болезненностью в области энтезиса при пальпации. Наиболее часто поражаются энтезисы ахиллова сухожилия, подошвенного апоневроза, гребней и остей подвздошных костей, I и VII грудино-реберных сочленений.
Дактилит («палец-сосиска») характеризуется диффузным отеком пальцев кистей и/или стоп, который встречается примерно в 6% случаев аксСпА. Обычно он возникает в одном или нескольких пальцах одновременно. Диффузный отек или отечность всех пальцев конечности должны настораживать в отношении других причин их появления [9].
Пациенты с аксСпА часто имеют внескелетные проявления, такие как увеит, псориаз и ВЗК (язвенный колит или болезнь Крона). Воспаление радужной оболочки и цилиарного тела глазного яблока (иридоциклит), встречающееся в 25–35% случаев, может быть первым клиническим признаком аксСпА. Как правило, увеит возникает остро и при первой атаке носит односторонний, самоограниченный характер. Рецидивы происходят часто, нередко с вовлечение другого глаза. Клиническая картина увеита включает боль в глазах, покраснение, светобоязнь и ухудшение зрения. Симптоматические ВЗК обнаруживаются у 4–6% пациентов с аксСпА, тогда как бессимптомное воспаление слизистой оболочки кишки – у 50%. Псориаз наблюдается примерно у 10% больных аксСпА [9].
ЛАБОРАТОРНЫЕ И ИНСТРУМЕНТАЛЬНЫЕ МЕТОДЫ ДИАГНОСТИКИ
В клинической практике большинство врачей настороженно относятся к увеличению скорости оседания эритроцитов (СОЭ) и повышению уровня С-реактивного белка (СРБ), обоснованно считая их чувствительными маркерами воспалительного процесса [11]. Однако особенностью аксСпА служит отсутствие взаимосвязи между клиническими проявлениями болезни и уровнем СОЭ и СРБ. Более чем у 50% больных острофазовые показатели воспаления остаются в пределах нормальных величин или незначительно повышенными [3].
Несмотря на то что связь между аксСпА и HLAB27 – одна из самых сильных среди известных ассоциаций между аллелем HLA и болезнью [12], определение в крови этого антигена имеет вспомогательное значение и не является специфическим для диагностики заболевания. Анализ крови на HLAВ27 не может рассматриваться как рутинный скрининговый тест, подтверждающий или отрицающий диагноз у пациентов с болью в спине или артритом [11]. Его использование оправдано в тех случаях, когда после изучения жалоб, истории болезни и осмотра пациента предполагается наличие аксСпА, но результаты рентгенологического обследования не обнаруживают достоверного сакроилеита. В этой ситуации позитивный результат HLAВ27 будет в большей степени свидетельствовать в пользу диагноза. В то же время нельзя забывать о том, что часть больных аксСпА (до 20%) являются отрицательными по В27-антигену [3].
Согласно большинству клинических руководств, посвященных диагностике и лечению боли в спине, назначение инструментальных методов обследования (рентгенографии, магнитно-резонансной томографии и др.) оправдано при наличии веских подозрений на серьезную патологию – «знаков угрозы» (в англоязычной литературе как эквивалентный термин используется red flags – «красные флаги») или если их результаты могут изменить тактику лечения [11, 13]. К «красным флагам» следует причислить и ВБС.
Рентгенография – основной метод диагностики и определения скорости прогрессирования аксСпА. На полученных рентгенограммах в первую очередь оценивают состояние крестцово-подвздошных суставов с целью уточнения стадии сакроилеита, выявление которого необходимо для установления диагноза АС, а также необязательных, но характерных для АС рентгенографических признаков. Последние учитываются как дополнительные симптомы, согласующиеся с аксСпА: коксит (поражение тазобедренных суставов), симфизит (поражение лонного сочленения), поражение энтезисов в области седалищных, подвздошных костей, большого и малого вертела бедренных костей [14]. При рентгенологическом исследовании визуализируются хронические костные изменения, возникающие через несколько лет от появления боли в спине, поэтому оно малоинформативно при небольшой длительности заболевания.
В связи с этим больным с ВБС, у которых отсутствуют достоверные рентгенологические признаки сакроилеита (двусторонний II стадии и выше или односторонний III–IV стадии), необходимо назначать магнитно-резонансную томографию (МРТ) крестцово-подвздошных суставов, позволяющую обнаружить активное воспаление в прилежащих к суставу костях. Техническим условием проведения МРТ с целью обнаружения зон активного воспаления (остеита) является использование Т2-взвешенного режима с обязательным подавлением жировой ткани (STIR или T2-FatSat), тогда как для выявления поствоспалительных изменений (эрозий, склероза, анкилоза и жировой перестройки костной ткани) должен применяться T1-взвешенный режим [15].
КРИТЕРИИ ДИАГНОСТИКИ
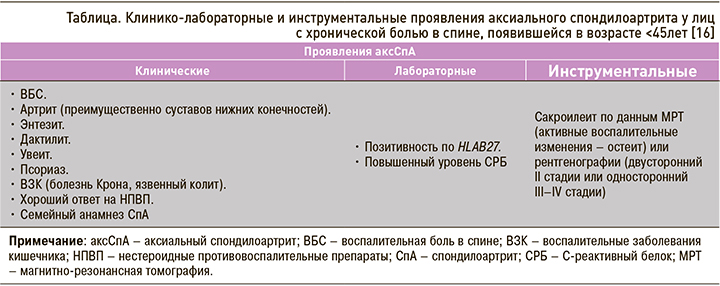
Таким образом, согласно критериям ASAS, пациенты, которые испытывают хроническую боль в спине, начавшуюся в возрасте до 45 лет, имеют аксСпА, если у них обнаруживаются визуальные признаки сакроилеита (по данным МРТ и/или рентгенографии) и 1 или более клинических признаков, характерных для группы СпА. В отсутствие сакроилеита у больного должен выявляться В27-антиген и два или более клинических признака СпА [16].
Поиск подходов к ранней диагностике аксСпА инициировал ряд соответствующих исследований. Их результаты стали основой для разработки алгоритмов скрининга и поддержки в принятии решения при направлении пациентов к ревматологу в случае подозрения на эту патологию. Было показано, что более сложные стратегии, включающие не только выявление ВБС, но и других признаков аксСпА, в сочетании с лабораторными и/или инструментальными методами обследования не были более эффективными, чем стратегии, которые требовали наличия только одного параметра аксСпА. Так, по данным Deodhar A. et al., эффективным способом скрининга пациентов с возможным аксСпА служит наличие хронической боли в спине >3 мес, начавшейся в возрасте до 45 лет, и одного из следующих признаков: ВБС, позитивности по HLA-B27 или сакроилеита [17].
Сходные результаты были получены в многонациональном многоцентровом рандомизированном исследовании RADAR (The Recognising and Diagnosing Ankylosing Spondylitis Reliably) [18]. В целом из 1049 пациентов, прошедших ревматологическое обследование, 397 (37,8%) был установлен диагноз аксСпА. При этом в 35,6% случаев это заболевание диагностировалось при использовании стратегии, включавшей 1 из 3 параметров: ВБС, позитивность по HLAВ27 или сакроилеит, подтвержденный любым методом визуализации. Выявляемость аксСпА незначительно (39,8%) увеличивалась при наличии любых 2 из следующих 6 критериев: ВБС, HLAB27, сакроилеита по данным визуализации, семейного анамнеза по СпА, хорошего ответа на лечение боли в спине нестероидными противовоспалительными препаратами (НПВП) или внескелетных проявлений (увеита, псориаза или ВЗК). Опыт отечественных ревматологов подтверждает, что внедрение образовательных программ для врачей-терапевтов, врачей общей практики, а также других специалистов, в которых большое внимание уделяется практическим аспектам выявления аксСпА среди лиц, страдающих хронической болью в спине, и своевременному направлению их к ревматологу, позволяет значительно сократить сроки диагностики этого заболевания [19].
ПОДХОДЫ К ЛЕЧЕНИЮ АКСИАЛЬНОГО СПОНДИЛОАРТРИТА
К целям лечения аксСпА относят облегчение и контроль признаков и симптомов заболевания, предотвращение структурных повреждений, нормализацию или сохранение функции, оптимизацию долгосрочного качества жизни, связанного со здоровьем, и социальную адаптацию пациентов [20]. Рекомендации по ведению больных аксСпА включают фармакологические и нефармакологические методы лечения. При этом среди нефармакологических методов терапии только образовательные программы и регулярные физические упражнения имеют наибольшую доказанную эффективность [21]. Было подтверждено положительное влияние на улучшение функции позвоночника и суставов регулярных физических упражнений как групповых, так и выполняемых в домашних условиях, а также комбинации их с физиотерапевтическими методами лечения [22].
Хороший клинический эффект от приема НПВП впервые был предложен Amor B. в качестве диагностического параметра, характеризующего СпА [23]. Под хорошим эффектом НПВП понимается отчетливое уменьшение болей после приема препаратов этого класса в течение 24–48 ч или возобновление болей в течение того же промежутка времени после их отмены. В соответствии с международными рекомендациями НПВП рассматриваются как первая линия терапии аксСпА [5, 24]. Эти лекарственные средства эффективно и быстро уменьшают боль и улучшают подвижность позвоночника и суставов, уменьшают выраженность и длительность утренней скованности. При этом их действие определяется в большей степени противовоспалительным, а не анальгетическим эффектом. В последнее время накапливается все больше клинических данных, подтверждающих способность НПВП не только купировать симптомы, но и замедлять развитие структурных повреждений при аксСпА [25]. Необходимо отметить, что эффективность НПВП является дозозависимой, поэтому они должны назначаться в полных терапевтических дозах, непрерывно, особенно при высокой активности аксСпА, с подбором наиболее оптимального препарата в каждом конкретном случае.
Внедрение генно-инженерных биологических (ингибиторов фактора некроза опухоли альфа и ингибиторов интерлейкина 17) и таргетных синтетических базисных противовоспалительных препаратов (ингибиторов янус киназ) стало прорывом в лечении аксСпА. Имеющиеся на сегодняшний момент данные подтверждают их эффективность и безопасность при этом заболевании. Показанием к назначению генно-инженерных биологических препаратов (ГИБП) служит сохраняющаяся высокая активность аксСпА на фоне последовательного применения НПВП в полной терапевтической дозе в течение 4 нед и более суммарно [26]. ГИБП хорошо подавляют воспаление в крестцово-подвздошных суставах и позвоночнике, выявляемое при МРТ на ранних стадиях. Более того, имеются данные о большей эффективности этих препаратов при небольшой длительности заболевания [26].
ЗАКЛЮЧЕНИЕ
Таким образом, ранняя диагностика аксСпА – один из значимых факторов, определяющих исходы заболевания. Повышение осведомленности об аксСпА (табл.) среди врачей, оказывающих первичную медико-социальную помощь, будет способствовать улучшению выявляемости этого заболевания и содействовать своевременному направлению пациентов к ревматологу с целью ранней диагностики и назначения эффективного лечения.



