Abstract. Cardiovascular disease remains the leading cause of death worldwide. The measurement of biological markers has revolutionized the diagnosis and monitoring of the effectiveness of the treatment of cardiac patients. The review article presented by us is devoted to a new promising biological marker, the transcription-modulating factor Jun 2 dimerization protein (JDP2). JDP2 is a bZip-type transcription factor that belongs to the activator protein-1 family. There are studies that allow us to consider the role of this marker in the diagnosis and evaluation of prognosis in patients with a cardiac profile. Studies on transgenic rodents and a number of clinical studies have shown that JDP2 is involved in the development of atrial fibrillation and heart failure.
ВВЕДЕНИЕ
Сердечно-сосудистые заболевания (ССЗ) остаются ведущей причиной смерти во всем мире [1, 2]. Измерение биологических маркеров произвело революцию в диагностике и контроле за эффективностью проводимого лечения пациентов с CCЗ. К наиболее широко используемым современным биомаркерам относятся натрийуретические пептиды и сердечные тропонины. Было выявлено и множество других биомаркеров, но лишь немногие из них нашли применение в реальной клинической практике [3, 4].
Представленные нами данные посвящены транскрипционно-модулирующему фактору Jun dimerization protein 2 (JDP2) и его роли при кардиоваскулярной патологии.
МЕТОДОЛОГИЯ ПОИСКА ИСТОЧНИКОВ
В статье представлен обзор актуальных публикаций, посвященных изучению JDP2. Анализ источников литературы проводился в базах данных PubMed, РИНЦ, MedLine, Google Scholar, Science Direct. Рассматривались зарубежные и отечественные публикации. Поиск выполнялся соответственно по следующим ключевым словам: JDP2, «биологические маркеры», «сердечно-сосудистые заболевания», biological markers, cardiovascular disease. Результаты различных исследований свидетельствуют, что существует научный интерес к изучению диагностической и прогностической ценности JDP2 при кардиоваскулярных заболеваниях.
БИОЛОГИЧЕСКИЕ АСПЕКТЫ JDP2
Белок димеризации JDP2 представляет собой фактор транскрипции bZip-типа, который принадлежит к семейству активаторных белков-1 (AP-1) [5, 6]. JDP2 первоначально был описан как репрессор AP-1 [5]. Он угнетает 12-O-тетрадеканоилфорбол-13-ацета-зависимую транскрипцию или аденозинмонофосфат зависимую транскрипцию путем гетеродимеризации с белками семейства Jun (Jun-C и Jun-B) [7]. JDP2 эпигенетически подавляет экспрессию генов за счет рекрутирования гистоновых деацетилаз, таких как, например, гистондеацетилаза-3 [8].
В 2013 г. Tanigawa S. et al. доказали, что JDP2 выступает в роли коактиватора рецептора прогестерона и фактора 2, связанного с транскрипционным фактором NF-E2 (Nrf2) [9]. У мышей с нокаутом JDP2 обнаружена аномальная дифференцировка остеокластов и нейтрофилов [10]. Nakade K. et al. опубликовали данные о том, что JDP2 подавляет дифференцировку адипоцитов [11]. Было показано, что активация фактора транскрипции 4 (ATF4) регулирует экспрессию гена JDP2 [12, 13]. Однако точный механизм, с помощью которого ATF4 активирует экспрессию JDP2, остается неизвестным [14].
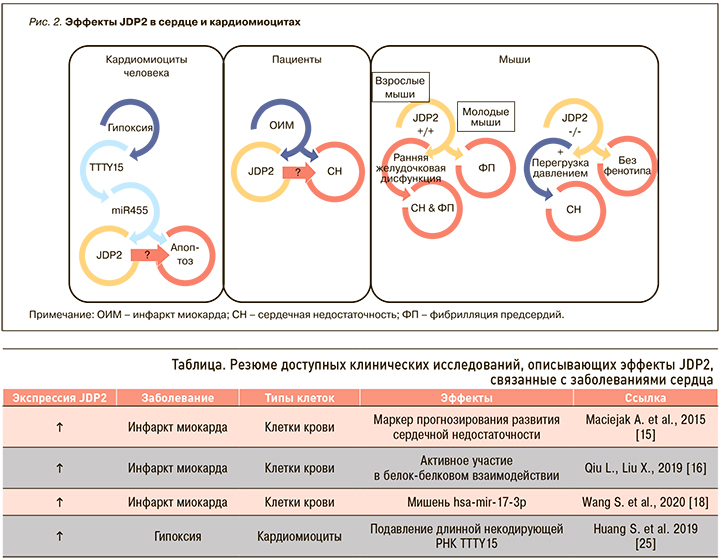
Совсем недавно повышенная регуляция длинной некодирующей рибонуклеиновой кислоты (РНК) TTTY15 была обнаружена при инфаркте миокарда (ИМ) в кардиомиоцитах человека в условиях гипоксии [5]. TTTY15 нацелен на микроРНК-455, которая регулирует экспрессию JDP2. Таким образом, существуют доказательства индукции JDP2 в условиях гипоксии в кардиомиоцитах человека [5].
JDP2 И СЕРДЕЧНО-СОСУДИСТАЯ ПАТОЛОГИЯ
Первый отчет о связи повышенной экспрессии JDP2 после острого ИМ (ОИМ) с прогрессированием сердечной недостаточности (СН) был опубликован Maciejak A. et al. в 2015 г. [15]. Ученые собрали образцы периферической крови у 111 пациентов с ИМ с подъемом сегмента ST (ИМпST); контрольную группу составил 41 пациент со стабильной ишемической болезнью сердца (ИБС) и без ИМ в анамнезе. На основании уровня N-концевого фрагмента мозгового натрийуретического гормона В-типа (NT-proBNP) в плазме крови и значений фракции выброса левого желудочка (ФВ ЛЖ) пациенты с ИМпST были разделены на 2 группы: с СН и без нее. Было обнаружено, что экспрессия JDP2 при ОИМ отмечена у больных с большей частотой развития СН после ОИМ. Это свидетельствует в пользу того, что JDP2 может служить ценным лабораторным маркером для прогнозирования развития СН у пациентов с ИМ [15].
В 2019 г. было показано, что JDP2 принимает активное участие в белок-белковом взаимодействии (protein–protein interactions, PPIs) у пациентов с ИМ [16].
Kehat I. et al. оценивали экспрессию JDP2 и ее связь с развитием дилатации полостей сердца на экспериментальных моделях 4-месячных мышей. Экспрессия JDP2 привела к массивной дилатации предсердий, нарушениям проводимости сердца и летальному исходу [17].
Shiai. W. и Na C. опубликовали данные исследования, посвященного изучению прогностической роли JDP2 в развитии СН после перенесенного ИМ [18]. Было идентифицировано несколько пар регуляторных взаимодействий между микроРНК и информационными РНК, в том числе hsa – miR – 17‑3p – JDP2. Эти результаты нашли подтверждение при обследовании небольшой группы пациентов с ИМ, у которых было обнаружено понижение регуляции has-mir-17-3p и повышение регуляции микроРНК JDP2 в крови [18].
Немецкими и венгерскими учеными было выполнено исследование in vivo на мышах со сверхэкспрессией JDP2 с целью изучения влияния JDP2 на прогрессирование СН. С момента рождения до возраста 4 нед избыточная экспрессия JDP2 предотвращалась путем кормления трансгенных мышей доксициклином, далее происходила сверхэкспрессия JDP2. Уже через 1 нед показатели сердца по данным эхокардиографии (ЭхоКГ) ухудшились. Через 5 нед было отмечено падение артериального давления (АД), ФВ ЛЖ и формирование дилатации ЛЖ. Также было обнаружено увеличение массы сердца, экспрессии микроРНК предсердного натрийуретического пептида (ANP), маркеров воспаления, коллагена и фибронектина. Экспрессия белка коллагена 1 увеличилась, вследствие чего развился фиброз. Критерием повышенного ремоделирования внеклеточного матрикса явилось увеличение активности матриксной металлопротеиназы 2 (MMP2, MMP-2; желатиназа A) [19].
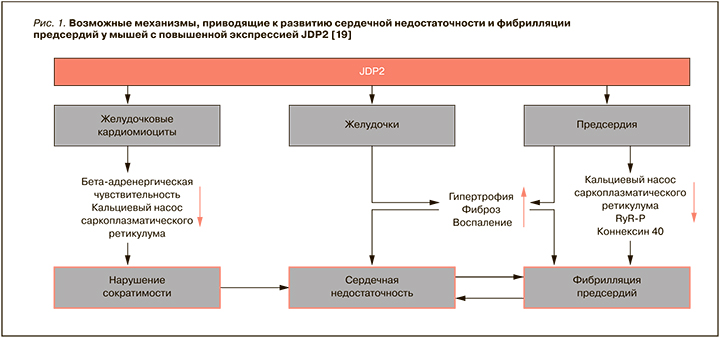
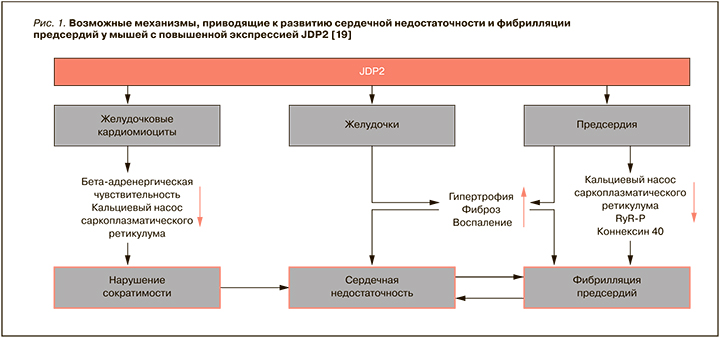
Heger J. et al. сообщили о сократительной дисфункции и на клеточном уровне: выделение кардиомиоцитов желудочков у мышей выявило снижение скорости укорочения и сокращения клеток при электростимуляции после одной недели сверхэкспрессии JDP2. После продолжительной сверхэкспрессии JDP2 сократительная способность снижалась еще больше, а после пожизненной сверхэкспрессии JDP2 положительные инотропные эффекты за счет бета-адренергической стимуляции нивелировались [20]. Также было описано нарушение кальциевого насоса саркоплазматического ретикулума (SERCA) в желудочках взрослых мышей со сверхэкспрессией JDP2 [19] (рис. 1).
Представляет интерес и исследование, проведенное Koren L. et al. Ученые опубликовали данные о том, что у мышей, чрезмерно экспрессирующих гомолог JDP2, активирующий фактор транскрипции 3 (ATF3), развивается увеличение массы сердца и нарушение его функции [21]. На моделях трансгенных мышей с сердечной сверхэкспрессией ATF3 было показано дезадаптивное ремоделирование сердца и снижение его функции. Также было обнаружено, что экспрессия ATF3 индуцируется сердечной ишемией в сочетании с реперфузией (ишемия–реперфузия) как в культивируемых клетках, так и в моделях на животных. У трансгенных мышей, экспрессирующих ATF3, обнаружили расширение и гипертрофию предсердий и желудочков. Микроскопическое исследование продемонстрировало дегенерацию и фиброз миоцитов. Трансгенное сердце имело пониженную сократимость и аберрантную проводимость. Интересно, что экспрессия белка сорцина, ингибирующего высвобождение кальция из саркоплазматического ретикулума, была повышена в сердцах трансгенных мышц. Эти результаты показали, что экспрессия ATF3 приводит к изменению экспрессии генов и нарушению функции сердца.
Предполагается, что ATF3 и JDP2 являются близкими структурными гомологами с похожими целевыми последовательностями в промоторе различных генов, которые дают аналогичные эффекты при их активации. Также было описано, что у мышей с двойным дефицитом JDP2 и ATF3 наблюдалось снижение дезадаптивного ремоделирования сердца и более низкая гипертрофия после продольного сужения аорты. Таким образом, баланс JDP2 и ATF3, по-видимому, служит весовым фактором в развитии СН [21, 22].
Как уже отмечено выше, описание трансгенных мышей JDP2 с непрерывной кардиоспецифической сверхэкспрессией JDP2 от рождения до 4-недельного возраста позиционировало JDP2 в качестве основного медиатора выраженной дилатации предсердий [17]. Показательно, что аритмии и дилатация предсердий были почти полностью обратимы при прекращении сверхэкспрессии JDP2 [17].
Parahuleva M. et al. выполнили исследование in vivo на мышах со сверхэкспрессией JDP2 для изучения влияния JDP2 на предрасположенность к спонтанной фибрилляции предсердий (ФП). Спонтанное начало ФП было зарегистрировано с помощью электрокардиограммы (ЭКГ) в сроки 4–5 нед сверхэкспрессии JDP2. В предсердной ткани мышей JDP2, помимо 3,6-кратного увеличения микроРНК JDP2, не удалось обнаружить никаких изменений в течение одной недели сверхэкспрессии JDP2. Дилатация и гипертрофия предсердий, удлинение кардиомиоцитов и фиброз стали очевидными через 5 нед сверхэкспрессии JDP2. На записи ЭКГ были выявлены удлинение интервала PQ и расширение зубцов P и QRS-комплексов, а также атриовентрикулярная блокада и пароксизмальная форма ФП. Наряду с этим было обнаружено снижение уровней белков NCX, Cav1.2 и RyR2, транспортирующих ионы кальция, а также мРНК коннексина 40. Также было отмечено увеличение уровней ANP, моноцитарного хемотаксического белка 1 (MCP1), маркеров инфильтрации иммунных клеток (CD68, CD20) у мышей со сверхэкспрессией JDP2 [23].
Kehat I. et al. опубликовали данные о том, что сердечная сверхэкспрессия нескольких факторов, подавляющих транскрипцию членов семейства bZIP, таких как нефосфорилируемая форма транскрипционного фактора CREB и ATF3, вызывала массивную дилатацию предсердий. Чтобы попытаться охарактеризовать этот путь, ученые выделили мощный ингибирующий bZIP белок димеризации Jun 2. Экспрессия JDP2 влекла за собой массивную дилатацию предсердий, потерю экспрессии коннексина 40 (Cx40), коннексина 43 (Cx43) и легкой цепи миозина 2 (MLC2a), а также нарушения атриовентрикулярной проводимости и летальный исход. Ингибирование экспресии JDP2 нивелировало его негативное влияние на сердце. Авторы заключили, что ингибирование bZIP может стать новой лекарственной мишенью для предотвращения дилатации предсердий [24].
Huang S. et al. описали повышенную экспрессию TTTY15, ассоциированную с гипоксией, в кардиомиоцитах пациентов с ИМ. Было показано, что подавление длинной некодирующей РНК TTTY15 ослабляет индуцированное гипоксией повреждение кардиомиоцитов [25].
Резюме доступных клинических исследований, которые описывают эффекты JDP2, связанные с кардиологическими заболеваниями, представлено в таблице.
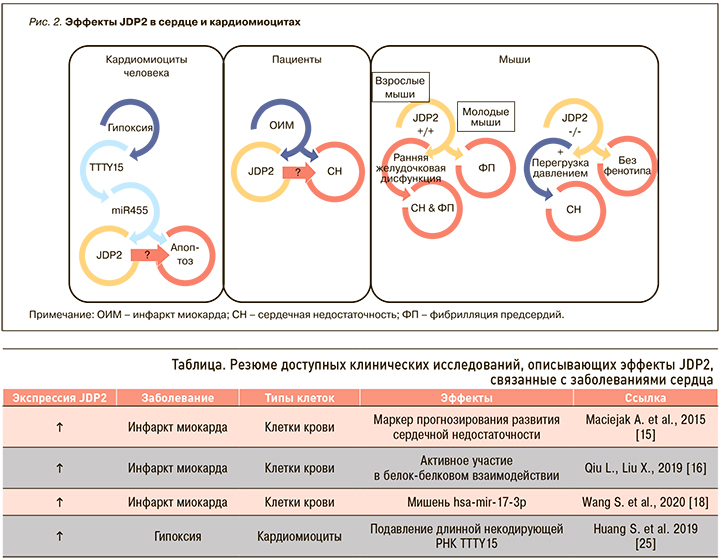
На рисунке 2 обобщены результаты имеющихся данных о кардиальных эффектах JDP2.
ЗАКЛЮЧЕНИЕ
Определение новых сердечно-сосудистых биомаркеров, анализ их патофизиологических аспектов и изменения концентрации под влиянием различных вариантов лечения позволяют нам понять многие патогенетические особенности развития и течения СН [26, 27]. На сегодня определение концентраций BNP и NT-proBNP служит неким «золотым стандартом» диагностики СН и прогнозирования ее течения, однако ограничения, обусловленные влиянием многих факторов на их концентрации, неопределенность пороговых значений и низкая информативность при СН с нормальной ФВ ЛЖ предопределяют необходимость дальнейшего поиска высокочувствительных и специфичных лабораторных маркеров [3, 4, 28]. Новые маркеры, такие как маркер фиброза галектин-3 (Gal-3), стимулирующий фактор роста ST2, пептидный гормон адреномедуллин, суррогатный маркер вазопрессин, хемокин-CX3CL1 и другое, все больше находят свое место в клинической практике [3, 4, 29]. Кроме того, весьма важен мультимаркерный подход к диагностике СН, стратификации ее риска и оценке эффективности лечения [3, 4, 30].
Появляются работы, позволяющие рассматривать роль JDP 2в диагностике и оценке прогноза у пациентов кардиологического профиля. Исследования на трансгенных грызунах и ряд клинических исследований показали, что JDP2 принимает участие в развитии ФП и СН (см. рис. 1). Тем не менее точная функция этого биологического маркера еще достаточно туманна, что предопределяет необходимость будущих научных и клинических исследований в этом направлении.
1. Roth G.A., Mensah G.A., Johnson C.O. et al. GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 Study. J Am Coll Cardiol. 2020; 76(25): 2982–3021. https://dx.doi.org/10.1016/j.jacc.2020.11.010.
2. Shi M., Tang R., Huang F. et al. Cardiovascular disease in patients with type 1 diabetes: Early evaluation, risk factors and possible relation with cardiac autoimmunity. Diabetes Metab Res Rev. 2021; 37(6): e3423. https://dx.doi.org/10.1002/dmrr.3423.
3. Алиева А.М., Резник Е.В., Гасанова Э.Т. с соавт. Клиническое значение определения биомаркеров крови у больных с хронической сердечной недостаточностью. Архивъ внутренней медицины. 2018; 5: 333–345. [Alieva A.M., Reznik E.V., Hasanova E.T. et al. Clinical value of blood biomarkers in patients with chronic heart failure. Arkhiv vnutrenney meditsiny = Archives of Internal Medicine. 2018; 5: 333–345 (In Russ.)]. https://dx.doi.org/10.20514/2226-6704-2018-8-5-333-345. EDN: YKJWIP.
4. Алиева А.М., Пинчук Т.В., Алмазова И.И. и с соавт. Клиническое значение определения биомаркера крови ST2 у больных с хронической сердечной недостаточностью. Consilium Medicum. 2021; 6: 522–526. [Alieva A.M., Pinchuk T.V., Almazova I.I. et al. Dinical value of blood biomarker ST2 in patients with chronic heart failure. Consilium Medicum. 2021; 6: 522–526 (In Russ.)].https://dx.doi.org/10.26442/20751753.2021.6.200606. EDN: ZWUXUD.
5. Euler G., Kockskamper J., Schulz R., Parahuleva M.S. JDP2, a novel molecular key in heart failure and atrial fibrillation? Int J Mol Sci. 2021; 22(8): 4110. https://dx.doi.org/10.3390/ijms22084110.
6. Tsai M.H., Wuputra K., Lin Y.C. et al. Multiple functions of the histone chaperone Jun dimerization protein 2. Gene. 2016; 590(2): 193–200. https://dx.doi.org/10.1016/j.gene.2016.03.048.
7. Aronheim A., Zandi E., Hennemann H. et al. Isolation of an AP-1 repressor by a novel method for detecting protein-protein interactions. Mol Cell Biol. 1997; 17(6): 3094–102. https://dx.doi.org/10.1128/MCB.17.6.3094.
8. Darlyuk-Saadon I., Weidenfeld-Baranboim K., Yokoyama K.K. et al. The bZIP repressor proteins, c-Jun dimerization protein 2 and activating transcription factor 3, recruit multiple HDAC members to the ATF3 promoter. Biochim Biophys Acta. 2012; 1819(11–12): 1142–53. https://dx.doi.org/10.1016/j.bbagrm.2012.09.005.
9. Tanigawa S., Lee C.H., Lin C.S. et al. Jun dimerization protein 2 is a critical component of the Nrf2/MafK complex regulating the response to ROS homeostasis. Cell Death Dis. 2013; 4(11): e921. https://dx.doi.org/10.1038/cddis.2013.448.
10. Maruyama K., Fukasaka M., Vandenbon A. et al. The transcription factor Jdp2 controls bone homeostasis and antibacterial immunity by regulating osteoclast and neutrophil differentiation. Immunity. 2012; 37(6): 1024–36. https://dx.doi.org/10.1016/j.immuni.2012.08.022.
11. Nakade K., Pan J., Yoshiki A. et al. JDP2 suppresses adipocyte differentiation by regulating histone acetylation. Cell Death Differ. 2007; 14(8): 1398–405. https://dx.doi.org/10.1038/sj.cdd.4402129.
12. Mimura J., Inose-Maruyama A., Taniuchi S. et al. Concomitant Nrf2- and ATF4-activation by carnosic acid cooperatively induces expression of cytoprotective genes. Int J Mol Sci. 2019; 20(7): 1706. https://dx.doi.org/10.3390/ijms20071706.
13. Wang S., Chen X.A., Hu J. et al. ATF4 gene network mediates cellular response to the anticancer PAD inhibitor YW3-56 in triple-negative breast cancer cells. Mol Cancer Ther. 2015; 14(4): 877–88. https://dx.doi.org/10.1158/1535-7163.MCT-14-1093-T.
14. Liu Y., He J., Chen R. et al. AP-1 activity is a major barrier of human somatic cell reprogramming. Cell Mol Life Sci. 2021; 78(15): 5847–63. https://dx.doi.org/10.1007/s00018-021-03883-x.
15. Maciejak A., Kiliszek M., Michalak M. et al. Gene expression profiling reveals potential prognostic biomarkers associated with the progression of heart failure. Genome Med. 2015; 7(1): 26. https://dx.doi.org/10.1186/s13073-015-0149-z.
16. Qiu L., Liu X. Identification of key genes involved in myocardial infarction. Eur J Med Res. 2019; 24(1): 22.https://dx.doi.org/10.1186/s40001-019-0381-x.
17. Kehat I., Heinrich R., Ben-Izhak O. et al. Inhibition of basic leucine zipper transcription is a major mediator of atrial dilatation. Cardiovasc Res. 2006; 70(3): 543–54. https://dx.doi.org/10.1016/j.cardiores.2006.02.018.
18. Wang S., Cao N. Uncovering potential differentially expressed miRNAs and targeted mRNAs in myocardial infarction based on integrating analysis. Mol Med Rep. 2020; 22(5): 4383–95. https://dx.doi.org/10.3892/mmr.2020.11517.
19. Heger J., Bornbaum J., Wurfel A. et al. JDP2 overexpression provokes cardiac dysfunction in mice. Sci Rep. 2018; 8(1): 7647.https://dx.doi.org/10.1038/s41598-018-26052-w.
20. Hill C., Wurfel A., Heger J. et al. Inhibition of AP-1 signaling by JDP2 overexpression protects cardiomyocytes against hypertrophy and apoptosis induction. Cardiovasc Res. 2013; 99(1): 121–28. https://dx.doi.org/10.1093/cvr/cvt094.
21. Koren L., Alishekevitz D., Elhanani O. et al. ATF3-dependent cross-talk between cardiomyocytes and macrophages promotes cardiac maladaptive remodelling. Int J Cardiol. 2015; 198: 232–40. https://dx.doi.org/10.1016/j.ijcard.2015.06.099.
22. Kalfon R., Friedman T., Eliachar S. et al. JDP2 and ATF3 deficiencies dampen maladaptive cardiac remodeling and preserve cardiac function. PLoS One. 2019; 14(2): e0213081. https://dx.doi.org/10.1371/journal.pone.0213081.
23. Parahuleva M.S., Kockskamper J., Heger J. et al. Structural, pro-inflammatory and calcium handling remodeling underlies spontaneous onset of paroxysmal atrial fibrillation in JDP2-overexpressing mice. Int J Mol Sci. 2020; 21(23): 9095.https://dx.doi.org/10.3390/ijms21239095.
24. Kehat I., Hasin T., Aronheim A. The role of basic leucine zipper protein-mediated transcription in physiological and pathological myocardial hypertrophy. Ann N Y Acad Sci. 2006; 1080: 97–109. https://dx.doi.org/10.1196/annals.1380.009.
25. Huang S., Tao W., Guo Z. et al. Suppression of long noncoding RNA TTTY15 attenuates hypoxia-induced cardiomyocytes injury by targeting miR-455-5p. Gene. 2019; 701: 1–8. https://dx.doi.org/10.1016/j.gene.2019.02.098.
26. Алиева А.М., Батов М.А., Воронкова К.В. с соавт. Реналаза – новый инструмент в многокомпонентной оценке сердечной недостаточности. Клиницист. 2021; 1–4: 42–46. [Alieva A.M., Batov M.A., Voronkova K.V. et al. Renalase – a new instrument in multicomponent heart failure assessment. Klinitsist = Clinician. 2021; 1–4: 42–46 (In Russ.)].https://dx.doi.org/10.17650/1818-8338-2021-15-1-4-K644. EDN: HJAJMY.
27. Алиева А.М., Пинчук Т.В., Воронкова К.В. и др. Неоптерин – биомаркер хронической сердечной недостаточности (обзор современной литературы). Consilium Medicum. 2021; 10: 756–759. [Alieva A.M., Pinchuk T.V., Voronkova K.V. et al. Neopterin is a biomarker of chronic heart failure (review of modern literature). Consilium Medicum. 2021; 10: 756–759 (In Russ.)].https://dx.doi.org/10.26442/20751753.2021.10.201113. EDN: SKCMCT.
28. Алиева А.М., Байкова И.Е., Кисляков В.А. с соавт. Галектин-3: диагностическая и прогностическая ценность определения у пациентов с хронической сердечной недостаточностью. Терапевтический архив. 2019; 9: 145–149. [Aliyeva A.M., Baykova I.E., Kislyakov V.A. et al. Galactin-3: diagnostic and prognostic value in patients with chronic heart failure. Terapevticheskiy arkhiv = Therapeutic Archive. 2019; 9: 145–149 (In Russ.)]. https://dx.doi.org/10.26442/00403660.2019.09.000226. EDN: NSZGZS.
29. Алиева А.М., Алмазова И.И., Пинчук Т.В. с соавт. Значение копептина в диагностике и прогнозе течения сердечно-сосудистых заболеваний. Клиническая медицина. 2020; 3: 203–209. [Alieva A.M., Almazova I.I., Pinchuk T.V. et al. The value of copeptin in the diagnosis and prognosis of cardiovascular diseases. Klinicheskaya meditsina = Clinical Medicine. 2020; 3: 203–209 (In Russ.)].https://dx.doi.org/10.30629/0023-2149-2020-98-3-203-209. EDN: IBOPWG.
30. Алиева А.М., Алмазова И.И., Пинчук Т.В. с соавт. Фракталкин и сердечно-сосудистые заболевания. Consilium Medicum. 2020; 5: 83–86. [Alieva A.M., Almazova I.I., Pinchuk T.V. et al. Fractalkin and cardiovascular disease. Consilium Medicum. 2020; 5: 83–86 (In Russ.)]. https://dx.doi.org/10.26442/20751753.2020.5.200186. EDN: IGGQHI.
Amina Magomedovna Alieva, PhD in Medicine, associate professor of the Department of hospital therapy No. 2 of the Faculty of general medicine, N.I. Pirogov Russian National Research Medical University of the Ministry of Healthcare of Russia. Address: 117997, Moscow, 1 Ostrovityanova Str. E-mail:
.
ORCID: https://orcid.org/0000-0001-5416-8579. SPIN-code: 2749-6427
Elena V. Reznik, Dr. med. habil, professor, head of the Department of propaedeutics of internal diseases of the Faculty of general medicine, N.I. Pirogov Russian National Research Medical University of the Ministry of Healthcare of Russia, general practitioner, cardiologist, doctor of functional diagnostics, ultrasound diagnostics at City Clinical Hospital No. 31 of the Healthcare Department of Moscow. Address: 117997, Moscow, 1 Ostrovityanova Str. E-mail:
. ORCID: https://orcid.org/0000-0001-7479-418X. SPIN-code: 3494-9080. Researcher ID: N-6856-2016
Natalia V. Teplova, Dr. med. habil, professor, head of the Department of clinical pharmacology of the Faculty of general medicine, N.I. Pirogov Russian National Research Medical University of the Ministry of Healthcare of Russia. Address: 117997, Moscow, 1 Ostrovityanova Str. ORCID: https://orcid.org/0000-0002-7181-4680
Gayane G. Totolyan, PhD in Medicine, associate professor of the Department of hospital therapy No. 2 of the Faculty of general medicine, N.I. Pirogov Russian National Research Medical University of the Ministry of Healthcare of Russia. Address: 117997, Moscow, 1 Ostrovityanova Str. E-mail:
Elvina T. Gasanova, postgraduate student of the Department of hospital therapy No. 2 of the Faculty of general medicine, N.I. Pirogov Russian National Research Medical University of the Ministry of Healthcare of Russia. Address: 117997, Moscow, 1 Ostrovityanova Str.
Marina R. Kalova, postgraduate student of the Department of hospital therapy No. 2 of the Faculty of general medicine, N.I. Pirogov Russian National Research Medical University of the Ministry of Healthcare of Russia. Address: 117997, Moscow, 1 Ostrovityanova Str. E-mail:
. ORCID: https://orcid.org/0000-0002-8949-4523
Elina E. Sabanchieva, 6th year student of the Faculty of general medicine, A.I. Yevdokimov Moscow State University of Medicine and Dentistry of the Ministry of Healthcare of Russia. Address: 127473, Moscow, 20/1 Delegatskaya Str
Igor G. Nikitin, Dr. med. habil, professor, head of the Department of hospital therapy No. 2 of the Faculty of general medicine, N.I. Pirogov Russian National Research Medical University of the Ministry of Healthcare of Russia. Address: 117997, Moscow, 1 Ostrovityanova Str. E-mail:
. ORCID: https://orcid.org/0000-0003-1699-0881