Abstract. Existing evidence suggests that abdominal obesity (AO) serves as a marker of cardiovascular disease (CVD) risk independent of body mass index.
Aim: to evaluate the incidence of AO and its association with risk factors for CVD in middle-aged people.
Material and methods. An open, cross-sectional comparative study in 111 outpatients aged 45 to 59 years. The main group consisted of 57 patients with AO, the comparison group – 54 patients without AO. Conducted general clinical examination, laboratory diagnostics, assessment of cardiovascular risk, daily monitoring of blood pressure, echocardiography.
Results. AO was detected in 57 (51,4%) people, including 24 (42,1%) men and 33 (57,9%) women (p=0,134). Among middle-aged patients with AO, persons with dyslipidemia (82,5%), hyperuricemia (28,1%) and hypodynamia (47,4%) were more common. Also, in these patients, chronic kidney disease (CKD) (36,8%) and hypertension (78,9%) were more often detected, and the achievement of the target level of blood pressure (BP) was worse in patients with AO (8,9%). AO in combination with hypertension was associated with menopause (OR 17,2; 95% CI: 3,6–82,39; p <0,001), insufficient achievement of the target BP level (OR 12,9; 95% CI: 2,82–58,56; p=0,001), multimorbidity (OR 11,5; 95% CI: 2,43–54,5; p=0,002), physical inactivity (OR 8,83; 95% CI: 1,07–73,2; p=0,044), and hyperuricemia (OR 7,35; 95% CI: 1,99–7,1; p=0,003).
Conclusions. A high occurrence of metabolic risk factors and failure to achieve the target level of BP in the majority of working-age patients with AO was revealed, which was accompanied by an increase in the size of the heart chambers and the formation of left ventricular hypertrophy.
ВВЕДЕНИЕ
За период с 1990 по 2019 г. количество случаев сердечно-сосудистых заболеваний (ССЗ) в мире увеличилось почти вдвое: с 271 (95% доверительный интервал (ДИ): 257–285) до 523 млн (95% ДИ: 497–550). При этом наблюдается и рост смертности от ССЗ – с 12,1 (95% ДИ: 11,4–12,6) в 1990 г. до 18,6 млн (95% ДИ: 17,1–19,7) в 2019 г. [1]. Следует отметить, что наибольшее количество сердечно-сосудистых жизнеугрожающих событий в мире, включая нашу страну, регистрируется среди людей трудоспособного возраста [2, 3].
С 1995 по 2012 г. частота госпитализаций среди пациентов в возрасте 18–34 лет увеличилась с 11,2 до 18,0 на 10 000 у мужчин и с 3,8 до 5,8 на 10 000 у женщин. В возрастной группе 35–44 лет тот же показатель у мужчин вырос с 37,7 до 68,2 на 1000, а у женщин – с 24,8 до 35,8 на 10 000 [4].
Кроме того, в России доля умерших вне стационара составляет более 50%. Так, из-за болезней кровообращения в 2014 г. вне стационаров скончались 74,2% (697 809 человек); внутри этой группы в 81,7% случаев (402 288 человек) причиной смерти была ишемическая болезнь сердца (ИБС). Внегоспитальная смертность в нашей стране, по сравнению со странами Западной Европы и Северной Америки, в 3–5 раз выше, а средний возраст россиян, относящихся к этой категории, на 8–12 лет меньше [5].
Количество лет жизни, скорректированных по нетрудоспособности (англ. DALY, сокр. от Disability-adjusted life year), в последние годы увеличилось почти в два раза: с 17,7 (95% ДИ: 12,9–22,5) до 34,4 млн (95% ДИ: 24,9–43,6) [1, 6]. Таким образом, наряду со снижением смертности от ССЗ и вклада болезней этой группы в общий показатель смертности в мире произошло существенное увеличение числа лет, проживаемых кардиологическими больными в состоянии нетрудоспособности.
Развитие и течение ССЗ неизбежно ассоциировано с факторами риска. Среди них наибольший вклад в смертность населения вносит артериальная гипертензия (19% всех случаев смерти в мире), за которой следуют избыточная масса тела и ожирение [7]. Кроме того, в последние годы отмечена тенденция к нарастанию количества лиц трудоспособного возраста с метаболическими нарушениями и абдоминальным ожирением [8].
Существующие данные подтверждают, что абдоминальное ожирение, определяемое по окружности талии (ОТ), служит маркером риска ССЗ, не зависящим от индекса массы тела (ИМТ), а избыточное висцеральное ожирение ассоциируется с кардиометаболическим здоровьем и рассматривается как самостоятельный индикатор неблагоприятных сердечно-сосудистых исходов [9]. Изучение факторов, ассоциированных с абдоминальным ожирением, может значительно улучшить стратификацию риска ССЗ у лиц среднего возраста.
Цель исследования – оценить встречаемость абдоминального ожирения (АО) и его ассоциацию с факторами риска ССЗ у лиц среднего возраста.
МАТЕРИАЛЫ И МЕТОДЫ
Проведено открытое одномоментное сравнительное исследование.
Критерии включения: амбулаторные пациенты в возрасте от 40 до 59 лет, давшие добровольное письменное информированное согласие на участие в исследовании.
Критерии исключения: вторичная артериальная гипертензия (АГ), острый инфаркт миокарда (ИМ), нестабильная стенокардия, острое нарушение мозгового кровообращения в течение последних 3 мес до включения в исследование, постоянная форма фибрилляции предсердий, стадия декомпенсации заболевания с тяжелым течением, беременность и период лактации.
В исследование сплошным методом были включены 111 амбулаторных пациентов. У всех проводился сбор жалоб, оценка анамнеза, физикальный осмотр. АГ верифицировали при офисном уровне артериального давления (АД) ≥140/90 мм рт. ст. и при результате домашнего определения АД ≥135/95 мм рт.ст. не менее чем при трехкратном измерении на двух руках [10, 11]. Лечение АГ и других заболеваний (ИБС, дислипидемия, сахарный диабет) осуществлялось согласно современным рекомендациям и не менялось в течение 1 мес до включения в исследование.
ИМТ ≥30 кг/м2 рассматривался в качестве критерия ожирения [12]. АО определялось при наличии индекса окружности талия/бедро более 0,85 см у женщин и более 1,0 см у мужчин. Дислипидемия верифицировалась при значении общего холестерина (ОХС) >4,9 ммоль/л, и/или уровне липопротеидов низкой плотности (ЛПНП) >3,0 ммоль/л, и/или концентрации липопротеидов высокой плотности (ЛПВП) >1,7 ммоль/л, а также при наличии в анамнезе приема гиполипидемических препаратов. Риск ССЗ определяли по шкале Systematic Coronary Risk Estimation (SCORE) [12]. За величину целевого АД брался его уровень менее 140/90 мм рт.ст., при наличии сахарного диабета – менее 140/85 мм рт.ст. [10].
Эхокардиографическое исследование (ЭхоКГ) у исследуемых пациентов выполнялось в покое в стандартных позициях по общепринятой методике Feigenbaum H. (1986) на аппарате General Electric Vivid 3. Рассчитывалась масса миокарда левого желудочка (ММЛЖ) с последующим учетом веса и индексацией этого показателя на площадь поверхности тела для определения индекса ММЛЖ (ИММЛЖ). Гипертрофию ЛЖ диагностировали при ИММЛЖ >115 г/м2 у мужчин и >95 г/ м2 у женщин [13].
Суточное мониторирование АД (СМАД) проводили по стандартному протоколу на приборе Shiller BR-102 plus [14].
Статистический анализ осуществлялся с помощью программ STATISTICА 10 и SPSS 20. Для описания количественных признаков с нормальным распределением использовали среднее ± стандартное отклонение, сравнение количественных признаков выполняли по ранговому U-критерию Манна–Уитни, качественных – с применением таблиц сопряженности 2×2 по критерию χ2 Пирсона с поправкой Йетса. Для исследования взаимосвязи между непрерывными показателями применялся коэффициент ранговой корреляции Спирмена. Для оценки влияния признака использовался логистический регрессионный анализ с определением отношения шансов (ОШ) и 95% ДИ. Различия считали статистически значимыми при значениях двустороннего p <0,05.
РЕЗУЛЬТАТЫ
Среди амбулаторных пациентов, обратившихся за медицинской помощью по любой причине, АО было выявлено у 57 (51,4%) человек: 24 (42,1%) мужчины и 33 (57,9%) женщины (р=0,134).
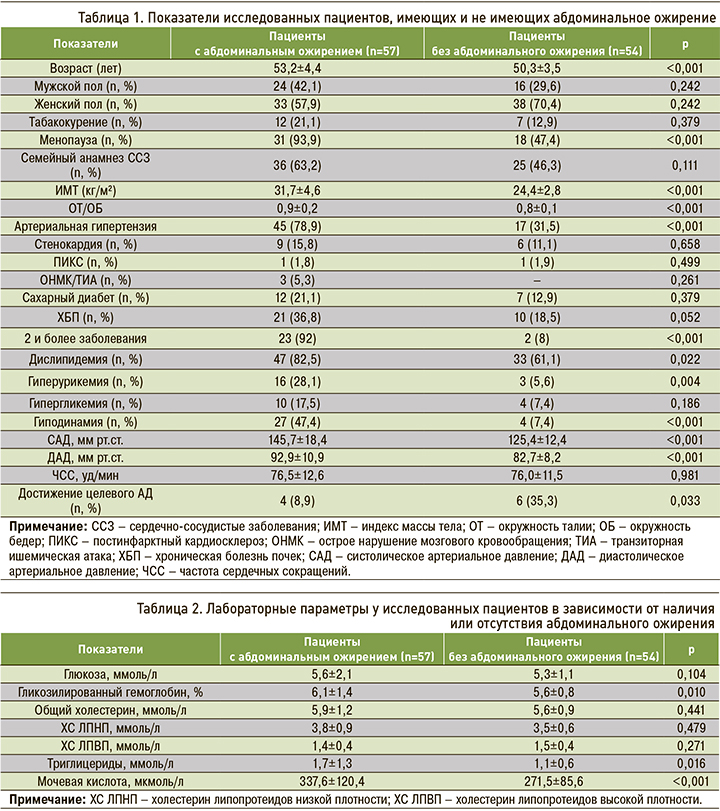
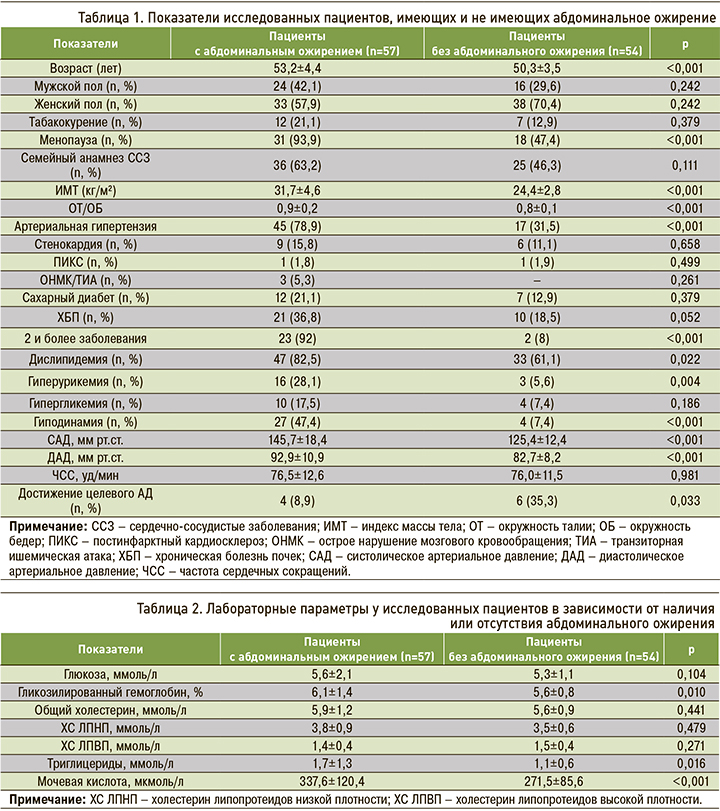
Характеристика исследованных пациентов среднего возраста, имеющих и не имеющих АО, представлена в таблице 1.
Среди пациентов с АО гипертоническая болезнь I стадии была выявлена у 8 (21,6%), II стадии – у 5 (13,5%), III стадии – у 24 (64,9%) пациентов; АГ 1-й степени имелась у 2 (5,4%), 2-й степени – у 19 (51,4%), 3-й степени – у 16 (43,2%) человек. Среди лиц без АО гипертоническая болезнь I стадии была обнаружена у 6 (35,3), II стадии – у 6 (35,3%), III стадии – у 5 (29,4%) пациентов; АГ 1-й степени страдали 2 (11.8%), 2-й степени – 14 (82,4%), 3-й степени – 1 (5,9%) человек.
Лабораторные параметры пациентов, включенных в исследование, приведены в таблице 2.
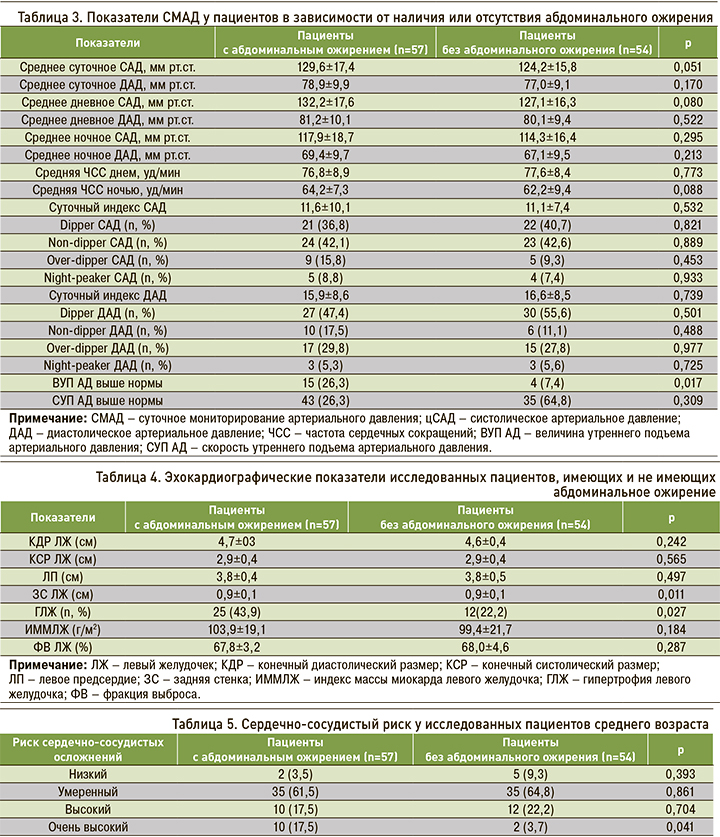
Значения суточного мониторирования АД (СМАД) у пациентов в зависимости от наличия или отсутствия АО отражены в таблице 3, эхокардиографические показатели – в таблице 4.
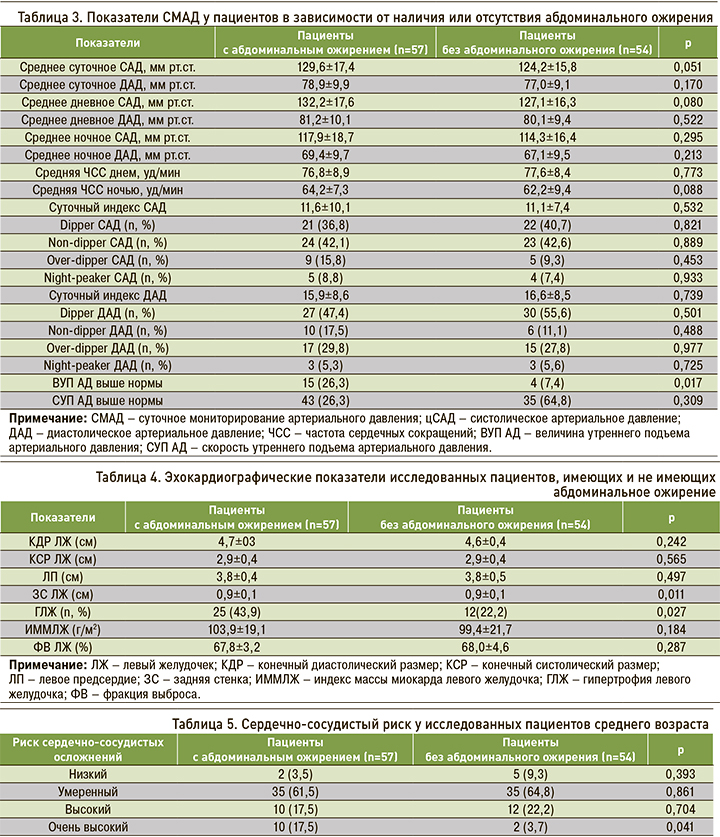
Риск развития ССЗ по шкале SCORE в исследуемой когорте составил 3,9±3,7%. У пациентов с АО этот показатель составил 4,1±4,6%, без АО – 3,4±3,2 (p=0,253), что соответствует умеренно повышенному кардиоваскулярному риску. Очень высокий риск сердечно-сосудистых осложнений чаще выявлялся у лиц с АО (табл. 5).
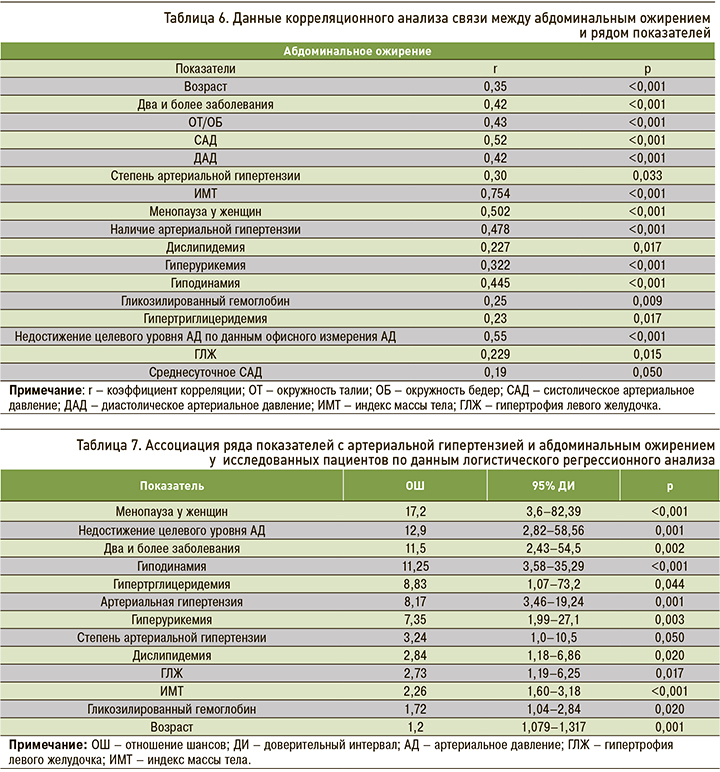
Корреляционный анализ связи между наличием АО и рядом показателей представлен в таблице 6.
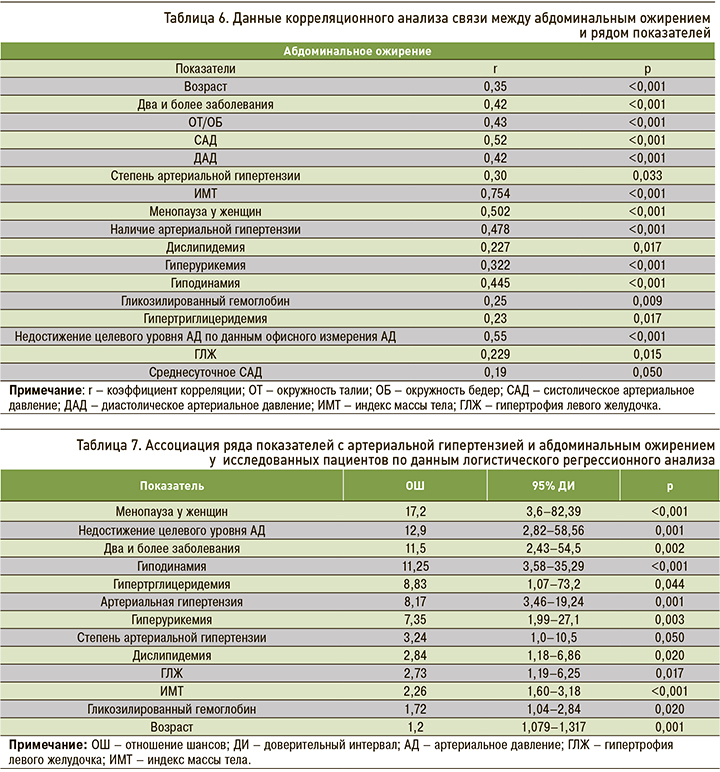
Обнаруженная ассоциация ряда показателей с АГ и АО в соответствии с результатами логистического регрессионного анализа представлена в таблице 7.
ОБСУЖДЕНИЕ
Согласно полученным нами данным, АО встречалось у 51,4% амбулаторных пациентов среднего возраста. Пациенты с АО были старше (р <0,001), и у них чаще выявлялась АГ (78,9%), чем у лиц без АО (31,5%; р <0,001).
В структуре заболеваемости среди болезней системы кровообращения АГ занимает ведущее место: по данным Росстата, больные с повышенным уровнем АД в 2015 г. составляли 41% в указанной когорте пациентов, в 2016 г. – 42%, в 2017 г. – 42,9% [15]. Результаты акции скрининга MMM-19 (от англ. May Month Measure) с участием 5394 участников из 21 региона России свидетельствуют о наличии АГ у 51,5% лиц в возрасте старше 25 лет [16].
Несмотря на снижение показателей повышенного АД (≥140/90 мм рт.ст.) в странах – членах Евросоюза на 35% за последние 35 лет, у каждого четвертого жителя по-прежнему диагностируется АГ. Систолическое АД (САД) выше у мужчин в сравнении с женщинами и выше в странах со средним уровнем дохода относительно государств с высоким уровнем дохода. В последние 40 лет также возросло количество людей с избыточной массой тела и ожирением: практически каждый пятый взрослый человек страдает этой патологией, что препятствует дальнейшему снижению смертности от ССЗ [17, 18].
Эпидемия ожирения во многом была вызвана либерализацией мировой торговли, экономическим ростом и быстрой урбанизацией, которые повлияли на образ жизни и потребление нездоровой пищи с тенденцией к увеличению приема животных жиров и сахара. В 2016 г. метаанализ Global BMI Mortality Collaboration показал, что у людей с избыточным весом и ожирением риск смертности увеличивается на 39% при увеличении ИМТ на каждые 5 кг/м2 (ОШ 1,39; 95% ДИ: 1,34–1,43) [19].
Согласно нашим данным, у пациентов с АО преобладала гипертоническая болезнь III стадии (у 64,9%) и АГ 2-й степени (у 51,4%). Этим они отличались от лиц без АО, среди которых преобладала гипертоническая болезнь II стадии (у 35,3%), а частота АГ 2-й степени равнялась 82,4%. Уровни САД и диастолического АД (ДАД) статистически значимо были выше в группе пациентов с АО.
Полученные результаты согласуются с существующими мировыми данными, в соответствии с которыми АО является глобальной проблемой из-за его ассоциации с множественными заболеваниями вследствие комплексного взаимодействия нездоровой окружающей среды, генетических и метаболических факторов [20–23].
В последние годы отмечена тенденция к нарастанию встречаемости АО среди лиц молодого и среднего возраста – с 10,8 до 26,9% у мужчин и с 26,4 до 30,8% у женщин (за период с 1993 по 2013 г.) [24]. По данным исследования ЭССЕ-РФ, распространенность АО в России среди женщин составляет 38,4%, среди мужчин – 24,3%. Количество женщин с ожирением увеличилось на 30%, а мужчин – в 2,5 раза за 10 лет с 2003 по 2013 г. [25].
В исследовании Liu F. et al. с участием 2785 госпитализированных пациентов с сахарным диабетом 2-го типа АО было выявлено у 64,9% пациентов – у 79,8% женщин и у 53,5% мужчин (p <0,001). Повышенная встречаемость АО обусловлена более старшим возрастом пациентов и наличием сопутствующего сахарного диабета, что подтверждает связь АО с риском развития этого заболевания [26].
По данным исследования корейских ученых, распространенность АО у взрослых с нормальной массой тела составила 6,9% у мужчин и 7,7% у женщин. Эта разница была значительно выше у женщин (р=0,020). Средний ИМТ в группе без АО составил 22,34±1,64 кг/м2 у мужчин и 21,86±1,69 кг/м2 у женщин. Средний ИМТ в группе с АО равнялся 24,1±0,81 кг/м2 у мужчин и 23,79±0,69 кг/м2 у женщин; таким образом, средний ИМТ был значительно больше в группе с АО, чем в контрольной группе без АО (р <0,001). Как у мужчин, так и у женщин средний возраст был выше в группах с АО, а распространенность АО имела тенденцию к повышению с увеличением возраста (р <0,001) [27].
По данным исследования Ю.И. Рагино с соавт., встречаемость АО в популяции 1415 человек в возрасте 25–44 лет г. Новосибирска составила 42,4%: у мужчин – 42,7%, у женщин – 42,1%. У лиц с АО АГ регистрировалась в 2,3 раза чаще, чем у лиц без АО. Также установлена ассоциация АО и повышенного уровня ХС ЛПНП (ОШ 1,527; 95% ДИ: 1,222–1,907; p=0,0001) [28].
Наши данные согласуются с существующими данными, согласно которым АО выявляется чаще у женщин (57,9%), по сравнению с мужчинами (42,1%), хотя эта разница не достигла статистической значимости (р=0,134).
Эпидемиологические исследования ЭССЕ РФ и ЭССЕ РФ-2 свидетельствуют о повышении осведомленности лиц в возрасте 25–64 лет о наличии у них АГ за период с 2014 по 2019 г., однако достижение целевых значений АД сохраняется на низком уровне [29, 30]. Одним из объяснений такой ситуации может быть наличие множественных факторов риска, потенцирующих друг друга и увеличивающих общий сердечно-сосудистый риск.
Доля лиц высокого и очень высокого сердечно-сосудистого риска в возрасте 25–64 лет в нашей стране составляет 31,3%, а с возрастом отмечается ее увеличение до более чем 72% [31]. У лиц с неосложненной АГ значение сердечно-сосудистого риска достигает 5,72%, а наиболее многочисленную группу составляют пациенты с умеренным (43,3%) и высоким/очень высоким риском (46%) [32].
Согласно нашим данным, очень высокий риск сердечно-сосудистых осложнений установлен у 17,5% лиц с АО и у 3,7% при его отсутствии (р=0,041), что согласуется с результатами других исследователей. Так, в Фремингемском исследовании была определена связь между ожирением и развитием кардиоваскулярных осложнений: относительный риск развития новых случаев заболевания АГ у лиц с ожирением для мужчин и женщин составил 1,75 и 1,46 соответственно в сравнении с лицами, имеющими нормальную массу тела [33]. В исследовании Community Hypertension Evaluation с участием 1 млн человек среди пациентов в возрасте 20–39 лет с избыточным весом АГ диагностировалась в 2 раза чаще, чем у лиц без ожирения [34].
Исследование Health, Aging, and Body Composition Study [35] подтвердило тесную связь АО и АГ, причем эта ассоциация прослеживалась даже у лиц с низкой общей долей жира в организме. Многие исследователи рассматривают висцеральную жировую ткань как самостоятельный эндокринный орган, поскольку ее клетки синтезируют огромное количество гормонально активных веществ, таких как лептин, резистин, свободные жирные кислоты, фактор некроза опухоли-α, инсулиноподобный фактор роста, ингибитор активатора плазминогена-I, ангиотензиноген, ангиотензин-II, интерлейкины, простагландины, эстрогены и др. Эти вещества тесно ассоциированы с запуском нарушений метаболизма углеводов, липидов, изменением чувствительности к инсулину, а также патологических изменений в сердечно-сосудистой системе.
В патогенезе АГ при АО ведущую роль играют инсулинорезистентность и гиперинсулинемия, которые, вероятно, ответственны за развитие резистентности к проводимой антигипертензивной терапии у пациентов с АГ и метаболическим синдромом [36]. Данные Lamarche B. et al. [37] свидетельствуют о повышении риска развития ИБС и ее осложнений в 20 раз в течение 5 лет при наличии именно АО, а не ожирения, в сочетании с гиперинсулинемией натощак, повышенным уровнем апо-липопротеида В и ХС ЛПНП [38, 39].
Воспаление, вызванное ожирением, увеличивает вероятность окисления ЛПНП, что со своей стороны способствует атерогенезу. Инсулинорезистентность связана с дислипидемией (высоким уровнем триглицеридов, низким уровень ХС ЛПВП, наличием мелких, плотных частиц ЛПНП) и метаболическим синдромом (множественный фактор риска ССЗ, включающий АО, атерогенную дислипидемию, повышенное АД, резистентность к инсулину с или без непереносимости глюкозы, провоспалительные и протромботические состояния), которые, в свою очередь, ассоциированы с атеросклерозом [40, 41].
На сегодняшний день накоплен значительный опыт в профилактике и лечении АГ, однако существует ряд нерешенных вопросов касательно контроля за течением заболевания и достижения целевого значения АД. Согласно результатам нашего исследования, целевой уровень АД был достигнут у каждого третьего пациента без АО (35,3%) и только у 8,9% пациентов с АО (р=0,033).
АГ и атеротромбоз выступают не только ведущими причинами сердечно-сосудистых катастроф, но и системными заболеваниями, увеличивающими поражение других органов, что мы и наблюдали на примере пациентов, включенных в исследование. Среди пациентов среднего возраста с АО преобладали лица с мультиморбидностью (92%), дислипидемией (82,5%), гиперурикемией (28,1%) и гиподинамией (47,4%). Уровень гликолизированного гемоглобина (р=0,001) и время утреннего подъема АД выше нормы (р=0,017) чаще регистрировались в группе лиц с АО. Встречаемость ГЛЖ также превалировала среди пациентов с АО, но не в группе лиц без АО (43,9 и 22,2% соответственно; р=0,027).
В проведенном нами исследовании установлена ассоциация между АО и дислипидемией (ОШ 2,84; р=0,020), а наличие АО в 8,17 раза (р=0,001) увеличивало риск АГ у обследованных нами пациентов и в 12,9 раз (р=0,001) – вероятность недостижения целевого уровня АД. Полученные результаты вполне закономерны, поскольку абдоминальный тип ожирения рассматривается как фактор формирования многих ССЗ, при котором повышается продукция биологически активных веществ, включая провоспалительные цитокины, активно принимающих участие в метаболизме липидов, глюкозы, воспалении и тромбообразовании [42–47].
Ожирение, в том числе и АО, связано с повышенным риском развития деменции. Метаанализ продольных исследований с периодом наблюдения до 42 лет подтвердил риск развития деменции у лиц среднего возраста с ожирением (ОШ 1,33; 95% ДИ: 1,08–1,63), а также связь АО со снижением когнитивных функций в течение ближайших 6 лет [48].
У 9652 участников из UK BioBank (средний возраст 55 лет, 48% – мужчины) ИМТ, соотношение талии и бедер и жировая масса были ассоциированы с меньшим объемом серого вещества (β на 1 стандартное отклонение измерения -4113; 95% ДИ: от -4862 до -3364; -4272; 95% ДИ: от -5280 до -3264; -4590; 95% ДИ: от -5386 до -3793) [49].
Известна связь ССЗ с гиперурикемией, а многочисленные исследования подтверждают более высокую концентрацию мочевой кислоты в сыворотке крови у пациентов с ИБС, АГ, чем в группе здоровых лиц [47, 50].
Liu F. et al. обнаружили положительную связь между повышенным уровнем сывороточной мочевой кислотой и ожирением, особенно абдоминальным типом ожирения у пациентов с сахарным диабетом 2-го типа. Более того, отмечена значительная распространенность ожирения и АО по мере увеличения концентрации мочевой кислоты [26].
При ожирении усиливается катаболизм пуринов в жировой ткани, а образование мочевой кислоты, в свою очередь, вызывает митохондриальный окислительный стресс, стимулирующий накопление жира независимо от чрезмерного потребления калорий. Повышенный уровень мочевой кислоты служит независимым предиктором развития ожирения, резистентности к инсулину и сахарного диабета [51].
Наше исследование также выявило наличие кардиометаболических параллелей у лиц среднего возраста с АО и подтвердило его ассоциацию с гиперурикемиией (ОШ 7,35), гипертриглицеридемией (ОШ 8,83), гипертрофией левого желудочка (ОШ 2,73) и гиподинамией (ОШ 11,26).
Существует сильная корреляционная связь между общим ожирением и АО, однако некоторые люди могут быть определены как имеющие общее ожирение, но не АО. Также может иметь место АО при отсутствии общего ожирения по результатам расчета ИМТ. Имеющиеся кардиометаболические изменения и ССЗ у пациентов, которые имеют «ожирение с нормальным весом», рассчитанным по ИМТ, приводят к неправильной диагностике риска ССЗ, особенно у лиц с избытком жира, но не ожирением. Таким образом, увеличенная ОТ, даже у людей с нормальной массой тела, может свидетельствовать о высоком риске ССЗ, поскольку этот параметр служит индикатором АО, связанного с кардиометаболическими заболеваниями и являющегося предиктором смертности. Некоторые исследователи и эксперты рекомендуют в клинической практике оценивать, помимо ИМТ, и ОТ, поскольку появляется все больше данных, подтверждающих, что АО выступает маркером сердечно-сосудистого риска [52, 53].
ЗАКЛЮЧЕНИЕ
Результаты исследования подтверждают высокую встречаемость АО (51,4%) и метаболических расстройств среди лиц среднего возраста. У пациентов с АО преобладали лица с мультиморбидностью (92%), дислипидемией (82,5%), гиперурикемией (28,1%), гиподинамией (47,4%). АГ имелась у 78,9%, гипертоническая болезнь III стадии у – 64,9%, целевой уровень АД был достигнут у 8,9% пациентов с АО. Очень высокий риск сердечно-сосудистых осложнений установлен у 17,5% лиц с АО и у 3,7% при его отсутствии. Встречаемость гипертрофии левого желудочка также превалировала в группе пациентов с АО (43,9%), но не в группе лиц без АО (22,2%). Дислипидемия, АГ, гиперурикемия, гипертриглицеридемия, гипертрофия левого желудочка и гиподинамия оказались факторами, независимо ассоциированными с АО. Поскольку некоторые антропометрические показатели демонстрируют большую способность, чем другие параметры, идентифицировать факторы сердечно-сосудистого риска, АО можно рассматривать именно в качестве такого показателя.
1. Roth G.A., Mensah G.A., Johnson C.O. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study J Am Coll Cardiol. 2020; 76(25): 2982–3021. https://dx.doi.org/10.1016/j.jacc.2020.11.010.
2. Груздева О.В., Паличева Е.И., Максимов С.А. с соавт. Метаболические факторы риска развития болезней системы кровообращения в разных возрастных группах. Клиническая медицина. 2017; 95(11): 1035–1041. [Gruzdeva O.V., Palicheva E.I., Maksimov S.A. et al. Metabolic risk factors, as a trigger mechanism of the disease of the cardiovascular system in different age periods in the adult population. Klinicheskaya meditsina = Clinical Medicine. 2017; 95(11): 1035–1041 (In Russ.)].https://dx.doi.org/10.18821/0023-2149-2017-95-11-1035-1041. EDN: YQXTJL.
3. Singh A., Collins B.L., Gupta A. et al. Cardiovascular risk and statin eligibility of young adults after an MI: Partners YOUNG-MI registry. J Am Coll Cardiol. 2018; 71(3): 292–302. https://dx.doi.org/10.1016/j.jacc.2017.11.007.
4. George M.G., Tong X., Bowman B.A. Prevalence of cardiovascular risk factors and strokes in younger adults. JAMA Neurol. 2017; 74(6): 695–703. https://dx.doi.org/10.1001/jamaneurol.2017.0020.
5. Проект. Межведомственная стратегия формирования здорового образа жизни населения, профилактики и контроля неинфекционных заболеваний на период до 2025 года. Москва. 2016. Доступ: https://gnicpm.ru/wp-content/uploads/2020/01/proekt_strategii_niz-210616.pdf (дата обращения – 01.10.2022). [Project. Interdepartmental strategy for the formation of a healthy lifestyle of the population, prevention and control of non-communicable diseases for the period up to 2025. Moscow. 2016. URL: https://gnicpm.ru/wp-content/uploads/2020/01/proekt_strategii_niz-210616.pdf (date of access – 01.10.2022) (In Russ.)].
6. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020; 396(10258): 1223–49.https://dx.doi.org/10.1016/S0140-6736(20)30752-2.
7. Ким О.Т., Драпкина О.М. Эпидемия ожирения через призму эволюционных процессов. Кардиоваскулярная терапия и профилактика. 2022; 21(1): 72–79. [Kim O.T., Drapkina O.M. Obesity epidemic through the prism of evolutionary processes. Kardiovaskulyarnaya terapiya i profilaktika = Cardiovascular Therapy and Prevention. 2022; 21(1): 72–79. (In Russ.)].https://dx.doi.org/10.15829/1728-8800-2022-3109. EDN: MUTNZI.
8. Александров А.А., Розанов В.Б., Дадаева В.А. с соавт. Ассоциация курительного статуса и интенсивности курения с общим и абдоминальным ожирением в выборке мужчин среднего возраста. Кардиоваскулярная терапия и профилактика. 2020; 19(3): 20–28. [Aleksandrov A.A., Rozanov V.B., Dadaeva V.A. et al. Association of smoking status and smoking intensity with general and abdominal obesity in a sample of middle-aged men. Kardiovaskulyarnaya terapiya i profilaktika = Cardiovascular Therapy and Prevention. 2020; 19(3): 20–28 (In Russ.)]. https://dx.doi.org/10.15829/1728-8800-2020-2446. EDN: MBUIRO.
9. Powell-Wiley T.M., Poirier P., Burke L.E. et al. Obesity and cardiovascular disease: A scientific statement from the American Heart Association. Circulation, 2021; 143(21): e984–e1010. https://dx.doi.org/10.1161/CIR.0000000000000973.
10. Чазова И.Е., Ощепкова Е.В., Жернакова Ю.В. с соавт. Клинические рекомендации. Диагностика и лечение артериальной гипертонии. Кардиологический вестник. 2015; 10(1): 3–30. [Chazova I.E., Oschepkova E.V., Zhernakova YuV. et al. Clinical guidelines. Diagnostics and treatment of arterial hypertension. Kardiologicheskiy vestnik = Russian Cardiology Bulletin. 2015; 10(1): 3–30(In Russ.)]. EDN: TNAGNX.
11. Mancia G., Fagard R., Narkiewicz K. et al. 2013 ESH/ESC guidelines for the management of arterial hypertension. The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013; 34(28): 2159–19. https://dx.doi.org/10.1093/eurheartj/eht151.
12. Недогода С.В., Барыкина И.Н., Саласюк А.С. Национальные клинические рекомендации по ожирению: концепция и перспективы. Вестник Волгоградского государственного медицинского университета. 2017; 1: 134–40. [Nedogoda S.V., Barykina I.N., Salasyuk A.S. National clinical recommendations for obesity: concept and prospects. Vestnik Volgogradskogo gosudarstvennogo meditsinskogo universiteta = Herald of the Volgograd State Medical University. 2017; 1: 134–40 (In Russ.)]. EDN: YHQTDF.
13. Lang R.M., Badano L.P., Mor-Avi V. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28(1): 1–39.e14. https://dx.doi.org/10.1016/j.echo.2014.10.003.
14. Горбунов В.М. Суточное мониторирование артериального давления: современные аспекты. М.: Логосфера. 2015; 240 с. [Gorbunov V.M. Ambulatory monitoring of blood pressure: modern aspects. Moscow: Logosfera = Logosphere. 2015; 240 pp.(In Russ.)]. ISBN: 978-5-98657-051-8.
15. Чазова И.Е. Артериальная гипертония в свете современных рекомендаций. Терапевтический архив. 2018; 90(9): 4–7. [Chazova I.E. Arterial hypertension in the light of current recommendations. Terapevticheskiy arkhiv = Therapeutic Archive. 2018; 90(9): 4–7 (In Russ.)]. https://dx.doi.org/10.26442/terarkh20189094-7. EDN: UZNFRH.
16. Ротарь О.П., Толкунова К.М., Солнцев В.Н. с соавт. Приверженность к лечению и контроль артериальной гипертензии в рамках российской акции скрининга МММ19. Российский кардиологический журнал. 2020; 25(3): 98–108. [Rotar O.P., Tolkunova K.M., Solntsev V.N. et al. May Measurement Month 2019: adherence to treatment and hypertension control in Russia. Rossiyskiy kardiologicheskiy zhurnal = Russian Journal of Cardiology. 2020; 25(3): 98–108 (In Russ.)].https://dx.doi.org/10.15829/1560-4071-2020-3-3745. EDN: FBFQZP.
17. Timmis A., Vardas P., Townsend N. et al.; Atlas Writing Group, European Society of Cardiology. European Society of Cardiology: Cardiovascular disease statistics 2021. Eur Heart J. 2022; 43(8): 716–99. https://dx.doi.org/10.1093/eurheartj/ehab892.
18. Lopez A.D., Adair T. Is the long-term decline in cardiovascular-disease mortality in high-income countries over? Evidence from national vital statistics. Int J Epidemiol. 2019; 48(6): 1815–23. https://dx.doi.org/10.1093/ije/dyz143.
19. Global BMI Mortality Collaboration, Di Angelantonio E., Bhupathiraju S., Wormser D. et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016; 388(10046): 776–86. https://dx.doi.org/10.1016/S0140-6736(16)30175-1.
20. Ventura H.O., Stewart M., Lavie C.J. New guidelines, increasing hypertension numbers, resistance and resistance to change. Mayo Clin Proc. 2019; 94(5): 745–747. https://dx.doi.org/10.1016/j.mayocp.2019.03.014.
21. Драпкина О.М., Ким О.Т. Эпигенетика ожирения. Кардиоваскулярная терапия и профилактика. 2020; 19(6): 94–100. [Drapkina O.M., Kim O.T. Epigenetics of obesity. Kardiovaskulyarnaya terapiya i profilaktika = Cardiovascular Therapy and Prevention. 2020; 19(6): 94–100 (In Russ.)]. https://dx.doi.org/10.15829/1728-8800-2020-2632. EDN: SIRSCL.
22. Цыганкова Д. П., Кривошапова К.Е., Максимов С.А. с соавт. Частота выявления ожирения в зависимости от различных критериев в популяции среднего возраста городских и сельских жителей Сибирского региона. Кардиоваскулярная терапия и профилактика. 2019; 18(4): 53–61. [Tsygankova D.P., Krivoshapova K.E., Maksimov S.A. et al. Obesity prevalence rate, depending on various criteria in the average age population of urban and rural residents of the Siberian region. Kardiovaskulyarnaya terapiya i profilaktika = Cardiovascular Therapy and Prevention. 2019; 18(4): 53–61 (In Russ.)].https://dx.doi.org/10.15829/1728-8800-2019-4-53-61. EDN: QHKIJQ.
23. Молчанова О.В. Современный взгляд на профилактику и лечение артериальной гипертонии при ожирении. Профилактическая медицина. 2021; 24(6): 97–103. [Molchanova O.V. A modern view on the prevention and treatment of arterial hypertension in obesity. Profilakticheskaya meditsina = The Russian Journal of Preventive Medicine. 2021; 24(6): 97–103. (In Russ.)].https://dx.doi.org/10.17116/profmed20212406197. EDN: DLFXPZ.
24. Шальнова С.А., Деев А.Д., Баланова Ю.А. с соавт. Двадцатилетние тренды ожирения и артериальной гипертонии и их ассоциации в России. Кардиоваскулярная терапия и профилактика. 2017; 16(4): 4–10. [Shalnova S.A., Deev A.D., Balanova Yu.A. et al. Twenty years trends of obesity and arterial hypertension and their association in Russia. Kardiovaskulyarnaya terapiya i profilaktika = Cardiovascular Therapy and Prevention. 2017; 16(4): 4–10 (In Russ.)].https://dx.doi.org/10.15829/1728-8800-2017-4-4-10. EDN: ZGIDQL.
25. Баланова Ю.А., Шальнова С.А., Деев А.Д. с соавт. Ожирение в российской популяции – распространенность и ассоциации с факторами риска хронических неинфекционных заболеваний. Российский кардиологический журнал. 2018; 23(6): 123–130. [Balanova Yu.A., Shalnova S.A., Deev A.D. et al. Obesity in Russian population – prevalence and association with the non-communicable diseases risk factors. Rossiyskiy kardiologicheskiy zhurnal = Russian Journal of Cardiology. 2018; 23(6): 123–130 (In Russ.)]. https://dx.doi.org/10.15829/1560-4071-2018-6-123-130. EDN: XSLTTN.
26. Liu F., Chen S., Zhao W. et al. Urine uric acid excretion levels are positively associated with obesity and abdominal obesity in type 2 diabetes patients without chronic kidney disease. Diabetes Metab Syndr Obes. 2021; 14: 4691–703.https://dx.doi.org/10.2147/DMSO.S335558.
27. Kim H.Y., Kim J.K., Shin G.G. et al. Association between abdominal obesity and cardiovascular risk factors in adults with normal body mass index: Based on the Sixth Korea National Health and Nutrition Examination Survey. J Obes Metab Syndr. 2019; 28(4): 262–70. https://dx.doi.org/10.7570/jomes.2019.28.4.262.
28. Рагино Ю.И., Худякова А.Д., Стрюкова Е.В. с соавт. Распространенность заболеваний и патологических состояний у молодых людей до 45 лет с абдоминальным ожирением в Сибири. Бюллетень сибирской медицины. 2021; 20(4): 39–48. [Ragino Yu.I., Khudyakova A.D., Striukova E.V. et al. Prevalence of diseases and pathological conditions in young people under 45 years of age with abdominal obesity in Siberia. Byulleten’ sibirskoy meditsiny = Bulletin of Siberian Medicine. 2021; 20(4): 39–48 (In Russ.)].https://dx.doi.org/10.20538/1682-0363-2021-4-39-48. EDN: XCDHIO.
29. Бойцов С.А., Баланова Ю.А., Шальнова С.А. с соавт. Артериальная гипертония среди лиц 25–64 лет: распространенность, осведомленность, лечение и контроль. По материалам исследования ЭССЕ. Кардиоваскулярная терапия и профилактика. 2014; 13(4): 4–14. [Boytsov S.A., Balanova Yu.A., Shalnova S.A. et al. Arterial hypertension among individuals of 25–64 years old: prevalence, awareness, treatment and control. By the data from ECCD. Kardiovaskulyarnaya terapiya i profilaktika = Cardiovascular Therapy and Prevention. 2014; 13(4): 4–14 (In Russ.)]. https://dx.doi.org/10.15829/1728-8800-2014-4-4-14. EDN: SLQTRD.
30. Баланова Ю.А., Шальнова С.А., Имаева А.Е. с соавт. Распространенность, осведомленность, Лечение и контроль артериальной гипертензии в Российской Федерации (данные обсервационного исследования ESSERF-2). Рациональная фармакотерапия в кардиологии. 2019; 15(4): 450–466. [Balanova Yu.A., Shalnova S.A., Imaeva A.E. et al. Prevalence, awareness, treatment and control of hypertension in Russian Federation (Data of observational ESSERF-2 study). Ratsional’naya farmakoterapiya v kardiologii = Rational Pharmacotherapy in Cardiology. 2019; 15(4): 450–466 (In Russ.)]. https://dx.doi.org/10.20996/1819-6446-2019-15-4-450-466.
31. Шальнова С.А., Деев А.Д., Метельская В.А. с соавт. Информированность и особенности терапии статинами у лиц с различным сердечно-сосудистым риском: исследование ЭССЕ-РФ. Кардиоваскулярная терапия и профилактика. 2016; 15(4): 29–37. [Shalnova S.A., Deev A.D., Metelskaya V.A. et al. Awareness and treatment specifics of statin therapy in persons with various cardiovasular risk: the study ESSE-RF. Kardiovaskulyarnaya terapiya i profilaktika = Cardiovascular Therapy and Prevention. 2016; 15(4): 29–37 (In Russ.)]. https://dx.doi.org/10.15829/1728-8800-2016-4-29-37. EDN: WJDXKR.
32. Камышова Т.В., Сарычева А.А., Саргсян В.Д. с соавт. Реклассификации риска у пациентов, впервые обратившихся к врачу с неосложненной артериальной гипертонией. Кардиоваскулярная терапия и профилактика. 2019; 18(6): 19–25. [Kamyshova T.V., Sarycheva A.A., Sargsyan V.D. et al. Risk reclassification in patients first contacting a doctor with uncomplicated hypertension. Kardiovaskulyarnaya terapiya i profilaktika = Cardiovascular Therapy and Prevention. 2019; 18(6): 19–25 (In Russ.)]. https://dx.doi.org/10.15829/1728-8800-2019-6-19-25.
33. Hubert H.B., Feinleib M., McNamara P.M., Castelli W.P. Obesity as an independent risk factor for cardiovascular disease: A 26-year follow-up of participants of the Framingham Heart study. Circulation. 1983; 67(5): 968–77. https://dx.doi.org/10.1161/01.cir.67.5.968.
34. Stamler J., Stamler R., Riedlinger W.F. et al. Hypertension screening of 1 million Americans. Community Hypertension Evaluation Clinic (CHEC) program, 1973 through 1975. JAMA. 1976; 235(21): 2299–306. https://dx.doi.org/10.1001/jama.235.21.2299.
35. Santanasto A.J., Goodpaster B.H., Kritchevsky S.B. et al. Body composition remodeling and mortality: The Health Aging and Body Composition study. J Gerontol A Biol Sci Med Sci. 2017; 72(4): 513–19. https://dx.doi.org/10.1093/gerona/glw163.
36. Жернакова Ю.В., Железнова Е.А., Чазова И.Е. Артериальная гипертония у лиц с ожирением. Учебное пособие слушателей дополнительного профессионального образования по специальностям «кардиология», «врач общей практики», «терапия». М.: Каллиграф. 2021; 56 с. [Zhernakova Yu.V., Zheleznova E.A., Chazov I.E. Arterial hypertension in obese persons. Textbook for students of additional professional education in the specialties «cardiology», «general practitioner», «therapy». Moscow: Kalligraf = Calligrapher. 2021; 56 pp. (In Russ.)]. ISBN: 978-5-93856-343-8.
37. Lamarche B., Tchernof A., Mauriege P. Fasting insulin and apolipoprotein B levels and low density lipoprotein particle size as risk factors for ischemic heart disease. JAMA. 1998; 279(24): 1955–61. https://dx.doi.org/10.1001/jama.279.24.1955.
38. Nieves D.J., Cnop M., Retzlaff B. et al. The atherogenic lipoprotein profile associated with obesity and insulin resistance is largely attributable to intra-abdominal fat. Diabetes. 2003; 52(1): 172–79. https://dx.doi.org/10.2337/diabetes.52.1.172.
39. Погосова Н.В., Оганов Р.Г., Бойцов С.А. с соавт. Анализ ключевых показателей вторичной профилактики у пациентов с ишемической болезнью сердца в России и Европе по результатам российской части международного многоцентрового исследования EUROASPIRE V. Кардиоваскулярная терапия и профилактика. 2020; 19(6): 2739. [Pogosova N.V., Oganov R.G., Boytsov S.A. et al. Secondary prevention in patients with coronary artery disease in Russia and Europe: Results from the Russian part of the EUROASPIRE V survey. Kardiovaskulyarnaya terapiya i profilaktika = Cardiovascular Therapy and Prevention. 2020; 19(6): 2739 (In Russ.)]. https://dx.doi.org/10.15829/1728-8800-2020-2739.
40. Fransson E.I., Nordin M., Magnusson Hanson L.L., Westerlund H. Job strain and atrial fibrillation: Results from the Swedish Longitudinal Occupational Survey of Health and meta-analysis of three studies. Eur J Prev Cardiol. 2018; 25(11): 1142–49.https://dx.doi.org/10.1177/2047487318777387.
41. Garg P.K., Claxton J.S., Soliman E.Z. et al. Associations of anger, vital exhaustion, anti-depressant use, and poor social ties with incident atrial fibrillation: The Atherosclerosis Risk in Communities study. Eur J Prev Cardiol. 2020: 28(6): 633–40.https://dx.doi.org/10.1177/204748731989716.
42. Kotseva K. The EUROASPIRE surveys: Lessons learned in cardiovascular disease prevention. Cardiovasc Diagn Ther. 2017; 7(6): 633–39. https://dx.doi.org/10.21037/cdt.2017.04.06.
43. LeBlanc S., Coulombe F., Bertrand O.F. et al. Hypertriglyceridemic waist: A simple marker of high-risk atherosclerosis features associated with excess visceral adiposity/ectopic fat. J Am Heart Assoc. 2018; 7(8): e008139.https://dx.doi.org/10.1161/JAHA.117.008139.
44. Ashwell M., Gibson S. Waist-to-height ratio as an indicator of ‘early health risk’: Simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open. 2016; 6(3): e010159. https://dx.doi.org/10.1136/bmjopen-2015-010159.
45. Дружилов М.А., Кузнецова Т.Ю. Гетерогенность фенотипов ожирения в отношении сердечно-сосудистого риска. Кардиоваскулярная терапия и профилактика. 2019; 18(1): 161–167. [Druzhilov М.A., Kuznetsova Т.Yu. Heterogeneity of obesity phenotypes in relation to cardiovascular risk. Kardiovaskulyarnaya terapiya i profilaktika = Cardiovascular Therapy and Prevention. 2019; 18(1): 161–167 (In Russ.)]. https://dx.doi.org/10.15829/1728-8800-2019-1-161-167. EDN: YXKKHJ.
46. Wilson P.W., D’Agostino R.B., Sullivan L. et al. Overweight and obesity as determinants of cardiovascular risk: The Framingham experience. Arch Intern Med. 2002; 162(16): 1867–72. https://dx.doi.org/10.1001/archinte.162.16.1867.
47. Ларина В.Н., Ларин В.Г. Гиперурикемия и хроническая сердечная недостаточность: факторы риска и прогностические параллели. Consilium Medicum. 2020; 22(5): 62–66. [Larina V.N., Larin V.G. Hyperuricemia and chronic heart failure: Risk factors and prognostic parallels. Consilium Medicum. 2020; 22(5): 62–66 (In Russ.)].https://dx.doi.org/10.26442/20751753.2020.5.200158. EDN: XYOYVY.
48. Vemulapalli S., Dolor R.J., Hasselblad V. et al. Comparative effectiveness of medical therapy, supervised exercise, and revascularization for patients with intermit-tent claudication: A network meta-analysis. Clin Cardiol. 2015; 38(6): 378–86.https://dx.doi.org/10.1002/clc.22406.
49. Centers for Disease Control and Prevention. About multiple cause of death, 1999–2020.URL: https://wonder.cdc.gov/mcd-icd10.html (date of access – 01.10.2022).
50. Bombelli M., Ronchi I., Volpe M. et al. Prognostic value of serum uric acid: New-onset in and out-of-office hypertension and long-term mortality. J Hypertensi. 2014; 32(6): 1237–44. https://dx.doi.org/10.1097/HJH.0000000000000161.
51. Johnson R.J., Nakagawa T., Sanchez-Lozada L.G. et al. Sugar, uric acid, and the etiology of diabetes and obesity. Diabetes. 2013; 62(10): 3307–15. https://dx.doi.org/10.2337/db12-1814.
52. Alonso A., Jensen P.N., Lopez F.L. et al. Association of sick sinus syndrome with incident cardiovascular disease and mortality: The Atherosclerosis Risk in Communities study and Cardiovascular Health Study. PLoS One. 2014; 9(10): e109662.https://dx.doi.org/10.1371/journal.pone.0109662.
53. Bodin A., Bisson .A, Gaborit C. et al. Ischemic stroke in patients with sinus node disease, atrial fibrillation, and other cardiac conditions. Stroke. 2020; 51(6): 1674–81. https://dx.doi.org/10.1161/STROKEAHA.120.029048.