ВВЕДЕНИЕ
Пандемия новой коронавирусной инфекции (COVID-19) распространилась по всему миру и до настоящего момента остается причиной серьезного кризиса в области общественного здравоохранения. Хотя отличительной чертой COVID-19 является поражение органов дыхания, варьирующееся от легких симптомов верхних дыхательных путей до острого респираторного дистресс-синдрома [1], тяжелое течение инфекции также связано с мультисистемным поражением органов, значительная доля которого приходится на сердечно-сосудистую систему [2].
Известно, что все коронавирусы прямо или опосредованно поражают сердечно-сосудистую систему, вызывая развитие широкого спектра кардиоваскулярных осложнений, включая острый коронарный синдром, сердечную недостаточность и миокардит. Помимо этого, острое миокардиальное повреждение на фоне инфекции может быть связано с процессом неишемического генеза (миокардит, цитокин- или стресс-индуцированная кардиомиопатия и т.д.) или с ишемией миокарда вследствие эндотелиальной дисфункции, гипоксии и нарушений ритма [3]. По данным литературы, повышение уровня кардиоспецифических ферментов было зафиксировано у многих пациентов на фоне COVID-19, что в последующем было связано с более высокими показателями осложнений и летального исхода [2].
В ряде обзоров обсуждается влияние сердечно-сосудистых факторов риска, таких как ожирение, сахарный диабет (CД), дислипидемия, артериальная гипертензия (АГ) и курение на течение и смертность от новой коронавирусной инфекции [4]. Это может быть связано с тем, что латентное воспаление при этих заболеваниях приводит к неадекватному и несоразмерному иммунному ответу организма.
Ожирение вызывает различные нарушения в респираторной системе, а именно снижение податливости стенок грудной клетки и эластичности легочной ткани за счет увеличения кровенаполнения сосудов легких. Это, в свою очередь, способствует нарушению дыхательной функции, а гиперпродукция провоспалительных цитокинов и высокий риск тромбоза служат предпосылками тяжелого течения COVID-19 [5, 6]. Вклад ожирения в тяжесть течения болезни может быть до конца недооценен, так как оно довольно часто сопровождается сопутствующими патологиями – АГ, дислипидемией, нарушением толерантности к глюкозе.
Сведения о том, является ли дислипидемия прогностическим фактором тяжести и смертности у пациентов с COVID-19, противоречивы [7, 8]. По данным литературы, «цитокиновый шторм» сопровождается снижением уровня липопротеинов низкой и высокой плотности, повышением триглицеридов и окисленных липопротеинов [9], а клиническая тяжесть инфекции может определяться снижением уровня липопротеинов низкой плотности и общего холестерина [10]. С учетом имеющихся данных в контексте новой коронавирусной инфекции, вероятно, более актуален вопрос не столько о наличии дислипидемии, сколько о снижении смертности от COVID-19 на фоне приема статинов и омега-3-полиненасыщенных жирных кислот [9, 11].
АГ является самым распространенным фактором риска сердечно-сосудистых заболеваний (ССЗ) и часто встречается у больных COVID-19 [4]. Длительно неконтролируемое повышенное артериальное давление, по-видимому, может способствовать более тяжелому течению COVID- 19 в связи с поражением органов, обусловленным АГ, ухудшением эндотелиальной дисфункции, повреждением эндотелия и развитием эндотелиита на фоне инфицирования SARS-CoV-2 [12].
Среди пациентов с COVID-19 высока встречаемость не только АГ, но и сахарного диабета 2-го типа (СД 2) [13]. Показано, что СД 2, в особенности неконтролируемый, выступает фактором риска тяжелого течения COVID-19 и повышенной летальности [14]. Механизмы, лежащие в основе неблагоприятных исходов у этой когорты пациентов, включают хроническое воспаление с нарушением иммунного ответа, повышенную коагуляционную активность и дополнительное прямое повреждение поджелудочной железы вирусом SARS-CoV-2 [15].
Курение сигарет служит важным предиктором ССЗ. Метаанализ ранее опубликованных работ показал, что наличие этой вредной привычки, в том числе и в прошлом, приводит к тяжелому течению COVID-19 и более частому лечению в отделении реанимации и интенсивной терапии [16]; более того, объем поражения легочной ткани на фоне инфекции увеличивается в зависимости от стажа курения [17]. Наряду с этим курение табака потенциально увеличивает риск заражения коронавирусом, так как способствует возникновению кашля и чихания, что повышает распространение инфекции.
Немодифицируемые факторы риска, такие как возраст, пол, наследственность, генетические особенности, также могут влиять на течение новой коронавирусной инфекции. У мужчин старше 50 лет с сопутствующими заболеваниями чаще регистрируются ее тяжелое течение и летальный исход [18, 19], по сравнению с большинством пациентов молодого возраста и детьми, которые зачастую болеют легкой и инаппарантной формами COVID-19.
Среди симптомов COVID-19 также есть те, которые чаще сопутствуют тяжелой форме инфекции и осложняют ее течение. Так, наличие лихорадки, наблюдавшейся преимущественно у пациентов на стационарном лечении, увеличивало риск потребности в инвазивной вентиляции легких (ИВЛ) и летального исхода [20]. Пациенты с одышкой тоже чаще нуждались в стационарном лечении и ИВЛ [13]. Кроме того, одышка была более распространена у больных с двумя и более сопутствующими заболеваниями [13]. Нередко наблюдалась при COVID-19 и синусовая тахикардия. По данным литературы, у пациентов с этим ССЗ чаще отмечался повышенный уровень С-реактивного белка, имелись более выраженные изменения на рентгенографии органов грудной клетки и большая длительность госпитализации [21].
Распространенность факторов сердечно-сосудистого риска представляет значительную проблему здравоохранения во всем мире. Большинство таких являются модифицируемыми, и соответственно выявление наиболее значимых среди них имеет большую ценность в разрезе превентивной персонифицированной медицины. С учетом вышесказанного целью нашего исследования стало изучения влияние предикторов сердечно-сосудистого риска на течение COVID-19 у лиц молодого и среднего возраста.
МАТЕРИАЛ И МЕТОДЫ
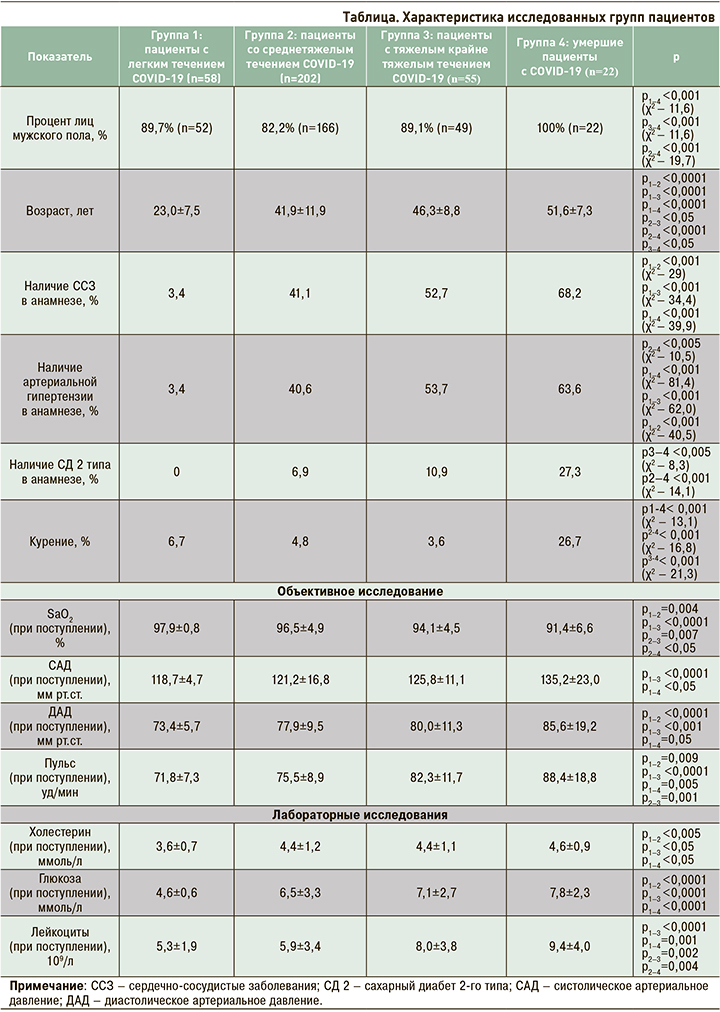
Проведен ретроспективный анализ 337 историй болезни лиц молодого и среднего возраста (40,0±13,3 лет). В зависимости от тяжести течения новой коронавирусной инфекции пациенты были разделены на 4 группы: 1-я группа – легкое течение (n=58); 2-я группа – среднетяжелое течение (n=202); 3-я группа – тяжелое и крайне тяжелое течение (n=55); 4-я группа – умершие (n=22).
При сборе первичной медицинской информации были проанализированы такие данные, как жалобы при поступлении, анамнез заболевания и жизни, наличие сердечно-сосудистых и сопутствующих заболеваний, факторы сердечно-сосудистого риска, объективные и лабораторно-инструментальные данные. Для создания базы данных была использована программа MS Excel 2016.
Статистическая обработка полученных результатов осуществлялась в программах Statistica for Windows и SPSS. Результаты представлены в виде M ± m, где M – среднее арифметическое, а m – стандартное отклонение. Оценка характера распределения в совокупности по выборочным данным проводилась с помощью критерия Колмогорова–Смирнова с поправкой Лиллиефорса. Для статистической обработки полученных данных использовались параметрические и непараметрические методы статистики, выбор которых был обусловлен характером распределения изучаемых признаков: для количественных признаков с нормальным распределением применялся дисперсионный анализ с последующим использованием критерия Стьюдента с поправкой Бонферрони, при предположении о неравенстве дисперсий сравнение групп выполнялось с помощью критерия Геймса–Хоуэлла. Равенство дисперсий оценивалось по критерию Ливиня. В случае отличия распределения от нормального применялся критерий Краскела–Уоллиса с последующим парным сравнением групп посредством U-критерия Манна–Уитни. Для качественных и порядковых признаков использовался Хи-квадрат. Проверка статистических гипотез проводилась по уровню значимости р <0,05. Для разработки статистической модели применялся логистический регрессионный анализ по многофакторной модели с пошаговым включением переменных и последующей оценкой диагностической ценности прогностической модели с помощью ROC-кривой и определением площади под ней.
РЕЗУЛЬТАТЫ
В исследовании во всех группах преобладали лица мужского пола. Было выявлено, что тяжесть течения COVID-19 закономерно увеличивалась с возрастом и индексом массы тела (ИМТ). ССЗ и АГ преобладали во 2-й, 3-й и 4-й группах. СД 2 и факт курения чаще регистрировались в группе умерших. Значения пульса, систолического и диастолического АД при поступлении были выше в 3-й и 4-й группах, при этом сатурация при дыхании атмосферным воздухом на момент поступления в стационар в этих группах была ниже, чем в других. Самые низкие уровни холестерина и глюкозы отмечались в 1-й группе. Наиболее высокий уровень лейкоцитов при поступлении в стационар наблюдался в 3-й и 4-й группах. Характеристика групп представлена в таблице.
При анализе полученных данных обращает на себя внимание, что лица с легким течением COVID-19 характеризовались более молодым возрастом по сравнению с остальными группами, но в то же время у них реже встречались факторы кардиоваскулярного риска. Как известно, риск более тяжелого течения новой коронавирусной инфекции возрастает по мере увеличения возраста, что, вероятно, обусловлено происходящими изменениями в сердечно-сосудистой системе и ее дисрегуляцией на фоне длительно существующих факторов сердечно-сосудистого риска и развития сердечно-сосудистого континуума. В связи с этим нам представлялось важным разработать модель для оценки вероятности тяжелого течения и летального исхода на фоне новой коронавирусной инфекции.
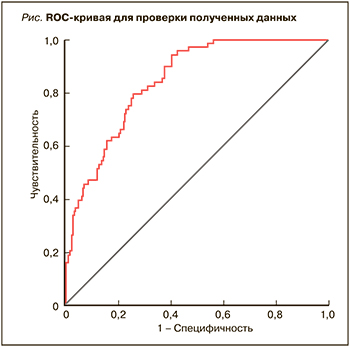
Для разработки статистической модели выявления вероятности тяжелого течения и летального исхода новой коронавирусной инфекции был использован логистический регрессионный анализ по многофакторной модели с пошаговым включением переменных с последующей оценкой диагностической ценности прогностической модели с помощью ROC-кривой и определением площади под ней. Вид сформированной математической модели представлен ниже (χ2=86,32; df=5; p <0,001):
P(Y) = 1/(1+e–(-10,71 + 0,60 × Х1 + 0,785 × Х2 + 0,904 × Х3 + 0,066 × Х4 + 0,125 × Х5)),
где Х1 – возраст пациента (лет); Х2 – наличие ожирения; Х3 – наличие одышки; X4 – частота пульса при поступлении в стационар (уд/мин); X5 – количество лейкоцитов при поступлении в стационар, ×109/л.
Чувствительность построенной модели составила 74,6%, специфичность – 72,1%, точность – 81%.
С помощью построения ROC-кривой была выполнена оценка качества созданной модели. Площадь под кривой (рис.), равная 0,84 (95% ДИ: 0,79–0,89), говорит об очень хорошем качестве модели. Исходя из анализа графического представления ROC-кривой, оптимальной точке отсечения соответствуют показатель чувствительности, равный 0,794 (79,4%), и показатель 1-специфичности, равный 0,258 (специфичность 74,2%). При оценке таблицы координат ROC-кривой точка отсечения составила 0,43.
ОБСУЖДЕНИЕ
В представленном исследовании показано, что тяжелое течение COVID-19 и летальный исход преимущественно встречались у лиц среднего возраста с повышенными показателями ИМТ, АД и высокой частотой пульса при поступлении в стационар. Более высокие значения глюкозы и холестерина ассоциировались с увеличением тяжести течения COVID-19. ССЗ, АГ, СД и курение в анамнезе преобладали в группе умерших и соответственно могут рассматриваться как предикторы неблагоприятного течения и риска развития летального исхода у больных молодого и среднего возраста с COVID-19.
Существует множество моделей оценки риска для прогнозирования неблагоприятного исхода у пациентов с COVID-19, но модели, включающие сердечно-сосудистые факторы риска, практически не встречаются. На основе таких выявленных факторов риска, как возраст, ожирение, одышка, частота пульса и количество лейкоцитов при поступлении в стационар, нами была разработана математическая модель прогнозирования тяжелого течения и развития летального исхода на фоне новой коронавирусной инфекции. Следует отметить, что в большинстве опубликованных работ медиана возраста исследованных пациентов составляет 60–70 лет. В нашем же исследовании оценивались параметры лиц молодого и среднего возраста как самой трудоспособной группы населения и целевой аудитории для осуществления первичной профилактики. Более того, по данным литературы, в ряде моделей часто используется уровень кардиоспецифических ферментов и параметры эхокардиографии (ЭхоКГ) [22]. Действительно, повреждение миокарда при коронавирусной инфекции является отрицательным прогностическим предиктором ее тяжелого течения и летальности, однако необходимо отметить, что в нашем исследовании уровень кардиоспецифических ферментов, анализируемый при поступлении в стационар, между группами не различался. ЭхоКГ выполнялась нами у малочисленной группы пациентов, поскольку целесообразность проведения такого исследования у каждого пациента сомнительна.
Таким образом, представленная нами математическая модель может использоваться в практической деятельности врачей всех профилей для выявления лиц с возможностью развития тяжелого течения и летального исхода на фоне новой коронавирусной инфекции среди пациентов молодого и среднего возраста. Кроме того, последствия поражения сердечно-сосудистой системы на фоне тяжелой инфекции могут ухудшить прогноз у больных COVID-19, что подчеркивает важность заблаговременного прогнозирования и оптимизации терапевтических стратегий.
ЗАКЛЮЧЕНИЕ
Отсутствие приверженности к здоровому образу жизни, а также старение общества способствуют увеличению числа больных ожирением, АГ, дислипидемией и СД 2. Наличие этих заболеваний, не всегда адекватное их лечение или недостаточная терапия с недостижением целевых значений терапии (например, показателей АД, уровня глюкозы и холестерина крови) может ухудшить течение новой коронавирусной инфекции. Своевременная медикаментозная коррекция уровня АД, поддержание целевого уровня гликемии, триглицеридов и липопротеинов низкой плотности, профилактика избыточного веса должны стать главной целью для своевременной профилактики осложнений при COVID-19. Более того, при выявлении у пациента с новой коронавирусной инфекцией риска тяжелого течения и неблагоприятного исхода заболевания следует незамедлительно назначать и/или при необходимости корректировать терапию факторов риска ССЗ. Принимая во внимание, что возраст является одним из самых сильных факторов риска летального исхода при СOVID-19, так как распространенность кардиоваскулярных предикторов может увеличиваться с каждым годом, в будущих исследованиях целесообразна оценка биологического возраста пациентов для более эффективной профилактики осложненного течения инфекции.
Необходимо также отметить роль вакцинопрофилатики у пациентов высокого риска возникновения неблагоприятного исхода на фоне COVID-19. Летальность и риск инвалидизации лиц молодого и среднего возраста с перенесенной коронавирусной инфекцией, зачастую большой срок временной нетрудоспособности, увеличение риска сердечно-сосудистых осложнений в процессе болезни и реконвалесцентном периоде требуют тщательного выявления кардиоваскулярных заболеваний и оценки предикторов сердечно-сосудистого риска; это подчеркивает важность заблаговременного прогнозирования, выявления и оптимизации терапевтических стратегий. Таким образом, с учетом представленных данных профилактические меры для своевременного предупреждения развития ССЗ, а также предотвращения тяжелого течения и летального исхода на фоне COVID-19 как никогда актуальны.