Современный этап развития медицины знаменует переход от эпохи «одного хронического заболевания» в эпоху «полиморбидной медицины» [1]. Широко известный принцип, что «лечить нужно не болезнь, а больного», был провозглашен еще знаменитым врачевателем древности Гиппократом. Матвей Яковлевич Мудров, известный клиницист-терапевт начала XIX в., сделал принцип Гиппократа девизом русской медицинской школы. Однако на протяжении XX в. медицинская наука развивалась вокруг нозологии и патофизиологии отдельных заболеваний, очень мало исследований было посвящено изучению сосуществования различных хронических заболеваний у одного пациента. Но развитие, как известно, всегда идет по спирали. Начиная с конца ХХ в., в специализированной литературе появился и стал все чаще использоваться термин «индивидуализированная медицина». Речь идет о новой модели организации медицинской помощи, которая позволит выбирать диагностические, лечебные и профилактические средства, оптимальные для конкретного человека с учетом всех его заболеваний, его генетических, физиологических и биохимических особенностей.
Всемирная организация здравоохранения определяет хронические заболевания, как «проблемы со здоровьем, которые требуют постоянного лечения в течение нескольких лет или десятилетий». Многие люди с хроническими проблемами со здоровьем имеют более одного заболевания [2]. Термины «коморбидность» и «полиморбидность» часто используются как синонимы. Тем не менее в последние годы под термином «коморбидность» понимают взаимодействие нескольких заболеваний. В то же время полиморбидность предполагает наличие 2-х заболеваний или более, которые могут и не находиться в причинно-следственной связи [3]. Таким образом, полиморбидность – это более широкое понятие. В целом взаимосвязь нескольких заболеваний может быть представлена четырьмя вариантами. Во-первых, одно заболевание может быть причиной другого заболевания. Во-вторых, два заболевания могут иметь общие факторы риска или общие механизмы патогенеза. В-третьих, два заболевания могут не иметь причинно-следственной связи или имеют только слабую ассоциацию [4]. В-четвертых, одно заболевание может быть вызвано ятрогенными факторами, возникшими в связи с другим заболеванием [5].
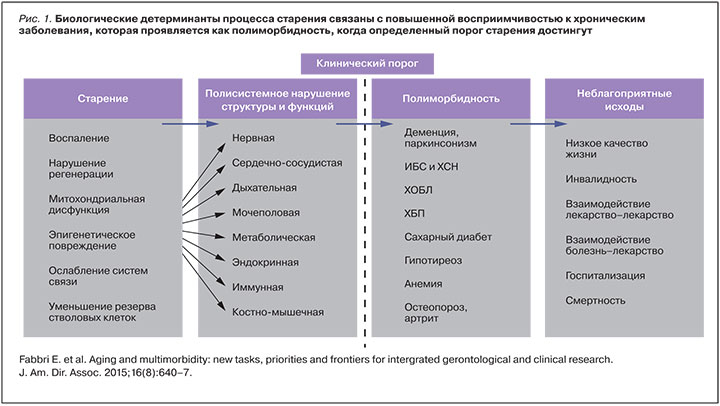
С точки зрения геронтологии, накопление заболеваний в пожилом возрасте обусловлено усугублением биологических детерминант старения, что приводит к нарушению структуры и функций систем органов, а также к развитию хронических заболеваний (рис. 1). Наиболее вероятно, что одни и те же механизмы, которые управляют старением, также управляют связанными с возрастом хроническими заболеваниями. Устранение этих механизмов могло бы предотвратить развитие полиморбидности. Поэтому изучение полиморбидности может помочь лучше понять процесс старения, т.к., по мнению экспертов, полиморбидность можно рассматривать как маркер ускоренного старения [1].
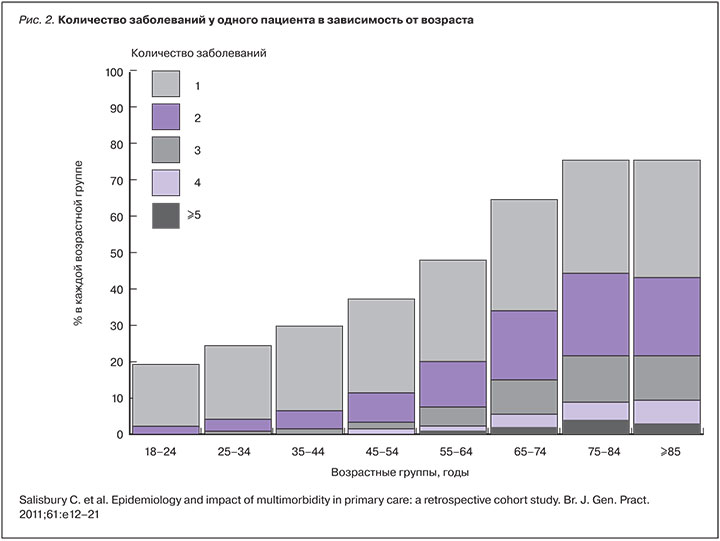
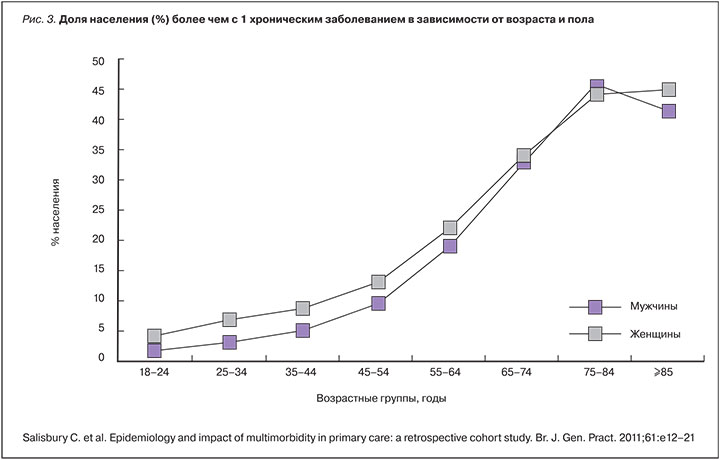
Распространенность полиморбидности растет и в настоящее время достигает 23–25% общего числа населения и до 65% – у людей в возрасте 65 лет и старше [6]. Кроме того, 55% пациентов с хроническими заболеваниями являются полиморбидными [7]. По оценкам экспертов, 26% населения США будет жить с несколькими хроническими заболеваниями к 2030 г. [8]. Хотя полиморбидность не ограничивается пожилыми людьми, ее распространенность значительно повышается с возрастом (рис. 2). По данным исследования, в Шотландии полиморбидность имеет место у 30,4% населения в возрасте от 45 до 64 лет, у 64,9% – в возрасте от 65 до 84 лет и у 81,5% – в возрасте 85 лет и старше [6]. Большинство экспертов считают факторами риска полиморбидности женский пол (рис. 3), низкий социально-экономический статус и более низкий уровень образования [9]. Недавнее исследование на основе большой выборки в Великобритании показало, что люди, живущие в самых бедных районах, значительно чаще имеют полиморбидность в среднем возрасте, чем те, кто живет в самых богатых районах. Они становятся полиморбидными на 10–15 лет раньше, чем их сверстники из более богатых семей [10]. Есть данные, что ожирение также является фактором риска полиморбидности у людей среднего возраста и пожилых людей [11]. Доказательства ассоциации полиморбидности с уровнем физической активности и табакокурением являются непоследовательными и противоречивыми, не было обнаружено ассоциации между полиморбидностью и потреблением алкоголя [12].
В последние годы опубликовано много исследований, касающихся ассоциативной полиморбидности. Речь идет о комплексном возникновении заболеваний, которые развиваются у пациентов с более высокой скоростью, чем ожидалось от чистой случайности [13]. В 1998 г. van den Akker и соавт. [14] опубликовали основополагающую статью, в которой выдвинули гипотезу о том, что некоторые заболевания имеют тенденцию появляться в кластерах. Авторы обнаружили, что больше людей чем ожидалось либо не имели никакого заболевания, либо имели 4 заболевания и более, в то время как меньше людей чем ожидалось имели 1 или 2 заболевания. Эти данные позволяют предположить, что некоторые люди имеют тенденцию к высокой восприимчивости к нескольким заболеваниям, в то время как другие кажутся необычайно устойчивыми. Другими словами, объединения некоторых специфических заболеваний происходит не только из-за случайности. Пожалуй, наиболее широко известным примером кластеризации хронических состояний является т.н. метаболический синдром, который связан с повышенным риском развития сердечно-сосудистых заболеваний и смертности от всех причин и может отражать генетическую предрасположенность к этой комбинации хронических заболеваний [15].
Некоторые другие исследования показали, что хроническая обструктивная болезнь легких (ХОБЛ) является частью системного воспалительного синдрома [16] и ассоциируется с такими заболеваниями, как рак легких [17], остеопороз [18], прогрессирование атеросклероза [19] и хронической болезни почек (ХБП) [20]. Комплекс сопутствующих заболеваний имеет накопительное влияние на смертность пациентов с ХОБЛ [21]. При исследовании когорты пациентов с бронхиальной астмой (БА) было найдено, что сахарный диабет (СД) был более распространенным у этих больных, но ожирение чаще встречалось у пациентов без БА [22]. Пациенты с болезнью Альцгеймера в 28% случаев также имеют клинически значимую хроническую сердечную недостаточность (ХСН), в 27% – ХОБЛ, в 22% – СД, в 20% – рак [23]. По сравнению с населением в целом, лица, получающие помощь при шизофрении или аффективных расстройствах в специализированных учреждениях, чаще страдают от БА, хронического бронхита, СД и болезней печени [24]. И, наконец, лица, страдающие от эпилепсии, имеют более высокую распространенность целого ряда хронических заболеваний, в том числе заболеваний кишечника, ХОБЛ, болезней сердечно-сосудистой системы, по сравнению с населением в целом [15, 25].
Систематический обзор и мета-анализ 26 статей показал достоверную связь между полиморбидностью и смертностью (ОР 1,44 [95% ДИ 1,34–1,55]). Число заболеваний также было положительно связано с риском смерти (ОР 1,20 [95% ДИ 1,10–1,30]). По сравнению с лицами с 1 заболеванием риск смерти был повышен у пациентов с 2 заболеваниями (ОР 1,73 [95% ДИ 1,41–2,13]) и у пациентов с ≥3 заболеваниями (ОР 2,72 [95% ДИ 1,81–4,08]) [26]. Среди пациентов с декомпенсацией ХСН, представленных в регистре ОРАКУЛ-РФ, наиболее высокая летальность в течение года наблюдалась именно у полиморбидных больных: летальность при пневмонии составила 49,5%, циррозе печени – 45,7%, при ХБП – 47,2% [27].
Полиморбидность связана не только с более высокими показателями смертности, но и с более высокими показателями инвалидности, с побочными эффектами лечения, с повышенным использования ресурсов системы здравоохранения, а также с более низким качеством жизни [28]. Течение заболеваний, поражение органов-мишеней у пациентов с полиморбидностью могут иметь существенные особенности, что отличает их от больных с одним заболеванием. Например, пациенты, имеющие сочетание ишемической болезни сердца (ИБС) и гастродуоденальной патологии, демонстрируют более тяжелое клиническое течение ИБС, часто атипичное, а также более существенные структурно-функциональные нарушения со стороны сердечно-сосудистой системы и желудочно-кишечного тракта, что способствует ускоренной декомпенсации состояния по сравнению с больными, страдающими изолированной патологией [29]. Пациенты с частыми приступами подагры имеют более высокую распространенность сопутствующих заболеваний (ХБП, артериальная гипертензия [АГ], дислипидемия, ИБС, ХСН) в сравнении с пациентами с редкими атаками [30]. У больных с сочетанием АГ и БА легочная гипертензия регистрируется значительно чаще, чем у пациентов с изолированными АГ или БА (38% против 16 и 7%). Кроме того, у пациентов с АГ в сочетании с БА чаще имеет место концентрическое ремоделирование и гипертрофия левого желудочка (ЛЖ), ремоделирование и гипертрофия правых отделов сердца [31]. Особенности ремоделирования и функционального состояния миокарда ЛЖ у пациентов с СД 2 типа и АГ 1–2 степени зависят от выраженности нарушений углеводного обмена; частота концентрической гипертрофии миокарда ЛЖ возрастает при наличии СД 2 типа, нарушения диастолической функции миокарда ЛЖ чаще выявляются у лиц с нарушениями углеводного обмена (СД 2 типа, нарушенная толерантность к глюкозе), чем у пациентов с нормогликемией [32].
Полиморбидность представляет собой фундаментальную проблему для современной доказательной медицины. Существует разрыв между высоким уровнем распространенности сопутствующих заболеваний у пожилых людей и клиническими исследованиями, которые фокусировались бы на кластерах сопутствующих заболеваний [33]. Для создания клинических рекомендаций, предназначенных для полиморбидных пациентов, большое значение имеет планирование новых клинических исследований. Пожилые люди с полиморбидностью систематически исключались или были недостаточно представлены в рандомизированных испытаниях [34]. Наблюдательные исследования, хотя и считаются более слабого качества, чем хорошо продуманные рандомизированные клинические исследования, но все-таки чаще включают пожилых людей с полиморбидностью и предоставляют важные данные о неблагоприятных событиях [34]. Например, значимость коморбидности как таковой для тактики лечения заболевания изучалась только в одном из больших исследований [35]. В этом исследовании была оценена частота сердечно-сосудистых осложнений, связанных с жестким контролем СД, среди лиц с разным уровнем коморбидности. Было показано, что достижение уровня HbA1с 6,5% или менее было связано с более низкой 5-летней частотой сердечно-сосудистых событий у пациентов с низким или умеренным уровнем коморбидности (ОР 0,60 [95% ДИ 0,42–0,85]; р=0,005), но не у пациентов с высокой коморбидностью (ОР 0,92 [ДИ 0,68–1,25], р=0,61). На основании этих данных был сделан вывод, что у пациентов с высоким уровнем коморбидности при СД 2 типа имеет место меньшая польза в отношение сердечно-сосудистого риска от интенсивного контроля уровня глюкозы и что коморбидность следует учитывать при терапии сахароснижающими препаратами у больных СД 2 типа.
Таким образом, необходимы новые клинические испытания, которые будут нацелены на больных с множественными хроническими состояниями и проверят эффективность лечения несколькими лекарственными препаратами. Эти исследования необходимы для создания новых руководств по клинической практике. Опираясь на них, врачи общей практики и другие специалисты смогут оптимизировать лечение полиморбидных пациентов [1], т.к. существующие клинические рекомендации не подходят для «управления» полиморбидностью. Пожилые люди с полиморбидностью разнородны с точки зрения заболевания, тяжести функционального состояния, прогноза, личных приоритетов, а также риска развития побочных эффектов, даже если имеют одинаковый диагноз. Не только сами физические лица, но и варианты их лечения будут отличаться, что требует более гибкого подхода к тактике ведения этих пациентов [34]. Вероятно, уже созрела необходимость перехода от нынешней практики лечения одного заболевания к подходу, ориентированному на пациента [7]. Например, в Великобритании Национальному институту здоровья и медицинской помощи (NICE) уже было предложено разработать рекомендации по полиморбидности для определения стратегии и тактики лечения этих пациентов [36].
Лечение пациентов с полиморбидностью в настоящее время является сложной задачей. С одной стороны, в ряде ситуаций эффективное лечение одного заболевания поможет оптимизировать лечение другого заболевания. Например, стандартные алгоритмы лечения ИБС у пациентов с гастродуоденальной патологией, не учитывающие значения эрадикации Helicobaсter pylori, не позволяют обеспечить достаточную эффективность терапии. Проведение полноценной эрадикационной терапии способствует более значимому, чем «стандартная» терапия улучшению клинико-функционального состояния пациентов, структурно-функциональных параметров сердца, функционального состояния эндотелия больных с сочетанием ИБС и гастродуоденальной патологии [37]. С другой стороны, фармакологические и немедикаментозные схемы лечения могут стать обременительными у людей со сложной полиморбидностью [10]. Клинические рекомендации в основном написаны так, как будто все пациенты имеют одно заболевание [38]. Для того чтобы лечить полиморбидного пациента, врачи должны сочетать все рекомендации, разработанные для каждого конкретного заболевания, что приводит к полипрагмазии и большим затратам времени и средств. Например, пациент с СД 2 типа, получающий сахароснижающие пероральные препараты, должен потратить 143 мин ежедневно для выполнения всех рекомендаций врача [39]. В другой ситуации при лечении гипотетической 78-летней женщины с 5-ю хроническими заболеваниями (остеопороз, остеоартрит, СД 2 типа, АГ и ХОБЛ), с учетом всех клинических рекомендаций, будет назначено до 12 отдельных лекарственных средств, принимаемых 5 раз в течение дня, и пациентка будет должна принимать участие в 14 нелекарственных мероприятиях в месяц [40].
Полипрагмазия влечет за собой проблему неблагоприятного лекарственного взаимодействия. Американское гериатрическое общество рассматривает лекарственную болезнь и лекарственные взаимодействия в качестве ключевой проблемы организации помощи пожилым людям с полиморбидностью [41]. С точки зрения экспертов, тема полипрагмазии должна рассматриваться в клинических рекомендациях гораздо в большем объеме, чем это имеет место сейчас [38]. Иногда добавление лекарственных препаратов в схему лечения может приносить больше вреда, чем пользы [42]. Возникает т.н. каскад назначений, когда побочные эффекты очередного лекарственного средства будут приняты за новое медицинское состояние, что приведет к дополнительным назначениям [43].
Важной также является проблема терапевтической конкуренции, которая предполагает, что назначение лекарственного средства для одного заболевания наносит вред другому заболеванию пациента. В национальной репрезентативной выборке пожилых людей в США более 20% лиц принимают по меньшей мере 1 препарат, который может отрицательно повлиять на их другое хроническое заболевание [44]. По данным одного исследования среди 91 возможной пары изученных хронических заболеваний, в 25 (27,5%) случаях пациенты получают по крайней мере 1 препарат, который потенциально может вступить в терапевтическую конкуренцию. Большую огласку получили такие случаи терапевтической конкуренции, как негативные эффекты ингибиторов ЦОГ-2 при заболеваниях сердечно-сосудистой системы или розиглитазона по отношению к пациентам с ХСН [45]. Степень распространенности терапевтической конкуренции остается неизвестной, но она может быть широко представлена, учитывая частоту полиморбидности у пожилых людей. Лекарства также могут отрицательно повлиять на пациентов через несколько других механизмов. Например, многие лекарственные средства могут способствовать возникновению таких гериатрических синдромов, как падения и депрессия, что опасно для пациентов с остеопорозом или принимающих антикоагулянты. ХБП тоже может усугубить негативные последствия лекарств [46]. Вполне вероятно, что многие из пациентов имеют выгоду от лекарств, несмотря на наличие терапевтической конкуренции. Наличие «конкурирующих» заболеваний не означает противопоказаний для лекарств; скорее, указывает клиницистам на необходимость взвешивать влияние лекарственных препаратов на каждое из заболеваний пациента. Это особенно верно, если одно вмешательство может иметь положительное влияние на некоторые из заболеваний в пределах общего кластера заболеваний [47]. К сожалению такие доказательства отсутствуют в настоящее время для многих лекарств и хронических заболеваний. Несмотря на это, клиницисты должны уметь определять приоритеты, какие лекарства, скорее всего, принесут пользу и в меньшей степени могут нанести вред конкретному больному [48].
В попытке уменьшить количество вмешательств, необходимо определить лекарственные средства, процедуры и нефармакологические методы лечения, которые могут быть неуместными у людей пожилого возраста или у лиц с полиморбидностью; эта информация должна быть широко представлена в клинических руководствах. В настоящее время появился новый подход для безопасного и эффективного прекращения приема лекарств, известный как «де-предписание», с целью минимизации вреда от полипрагмазии [49, 50]. Естественно, любое решение в отношении уменьшения количества препаратов должно быть принято после серьезной оценки для того, чтобы отмена была максимально безопасна. Однако надо учитывать, что существуют определенные классы препаратов, отмена которых нежелательна и/или проводится с большой осторожностью. Это лекарственные средства, применяющиеся для лечения заболеваний сердечно-сосудистой и центральной нервной системы [51]. Как правило, нельзя отменять более 1 препарата за раз [52].

Для реализации индивидуального подхода к ведению полиморбидных больных сформулирован «принцип Ариадны» [53] (рис. 4), который, как нить Ариадны, помогает выйти из лабиринта сложной клинической ситуации и представляет основные элементы непрерывного процесса консультирования для пациентов с полиморбидностью на уровне первичной медицинской помощи. Центральное место в процессе занимает совместный выбор реалистичных целей лечения семейным врачом пациента. Выбор является результатом тщательной оценки взаимодействия заболеваний и методов лечения. Для выбора цели лечения врач должен выявить приоритеты и предпочтения пациента: выживание, независимость, снятие боли и облегчение симптомов, потребность в паллиативной помощи. Далее необходимо сопоставить приоритеты пациента с предпочтениями врача и принять общее решение с пациентом. Если это возможно, желательно рассмотреть также предпочтения опекунов или членов семьи. После этого можно обсудить с пациентом выбранную реалистичную цель лечения и получить согласие пациента и/или членов семьи. При выборе метода лечения приходится взвешивать ожидаемые выгоды от лечения (и профилактики) и возможные недостатки и вред, учитывая весь спектр заболеваний пациента, его предпочтения и ожидаемую продолжительность жизни. Далее вместе с пациентом составляется график последующих посещений, чтобы оценить достижение поставленной цели и повторно пересмотреть взаимодействие болезней и методов лечения в связи с появлением новых обстоятельств. Необходимо вместе с пациентом составить график консультаций у других специалистов, которые должны быть осведомлены о цели лечения, выбранной пациентом и врачом. В идеале все медицинские работники, консультирующие пациента, должны быть информированы о принятии решений о лечении и иметь полный доступ к информации о пациенте.
Процесс не обязательно должен идти все время в одном русле, т.к. предпочтения пациента могут меняться с течением времени или тактику лечения придется скорректировать, например, вследствие возникновения недопустимых побочных эффектов. В отличие от пациентов с единичными заболеваниями, у больных с полиморбидностью имеет место широкое разнообразие потенциальных взаимодействий между заболеваниями и методами лечения. Поэтому при назначении нового метода лечения сразу должны быть проверены возможные взаимодействия лекарство–лекарство, лекарство–болезнь (терапевтическая конкуренция). Например, для пациента с ревматоидным артритом и ХСН пользу от нестероидных противовоспалительных препаратов необходимо соотносить с высоким риском декомпенсации ХСН [54]. Помимо возможных побочных эффектов лекарств, сложные схемы лечения должны вызвать настороженность врача и осознание повышенного риска снижения приверженности и недостаточного лечения [55]. Медикаменты, которые в настоящее время принимаются, должны регулярно пересматриваться [73], так же как и перечень других врачей, участвующих в лечении пациента. Если достижение запланированного результата лечения принесет больше вреда, чем пользы, или цели лечения конкурируют друг с другом, или общее бремя лечения является неприемлемым, то приоритеты должны быть установлены более жестко. При этом, прежде всего, необходимо учитывать прогноз пациента с точки зрения физического и психического здоровья, качества жизни и продолжительности жизни [56].
Кроме эффективно работающего врача первичного звена (семейный врач, участковый врач), для оптимального оказания медицинской помощи пожилым полиморбидным пациентам необходимо создание эффективной междисциплинарной команды, что ставит совершенно новые задачи перед системой организации медицинской помощи.
В качестве ответа на проблему полиморбидности в современном мире происходит формирование новой модели медицинской помощи, которая выходит за рамки традиционных подходов лечения конкретных заболеваний. Ее целью является удовлетворение разносторонних потребностей полиморбидных пациентов. «Интеграция» и «мультидисциплинарный подход» должны быть положены в основу реформирования здравоохранения, в ходе которого будут подготовлены будущие лидеры среди поставщиков медицинских услуг, «специализированные» в лечении сложных полиморбидных больных [1]. Например, существует высокий уровень доказательств, который демонстрирует, что для госпитализированных пациентов по поводу декомпенсации ХСН применение многопрофильных программ медицинской помощи значительно снижает общую смертность, повторные госпитализации, способствует улучшению качества жизни пациентов и снижению расходов на здравоохранение [57].
Полиморбидность, безусловно, создает также существенные трудности для политики распределения ресурсов здравоохранения на фоне старения населения и роста нежелательных социальных характеристик образа жизни [47, 58]. Большое значение возрастного градиента также означает, что, если не будет столь же высокого качества медицинской и социальной помощи людям с множественными хроническими заболеваниями, как и пациентам с одним заболеванием, существует риск того, что люди в конце жизни будут получать более низкое качество медицинской помощи, чем молодые люди, которые имеют меньше шансов иметь несколько заболеваний. Возрастные различия в качестве медицинской помощи должны быть причиной серьезного беспокойства общественности и государственных структур [58].
Предполагается, что новая модель развития здравоохранения, ориентированная на пациентов с полиморбидностью, будет связана с существенно более высокими затратами на здравоохранение, включая затраты на лекарственные препараты [59], на работу первичного звена медицинской помощи и на многократные консультации специалистов [60], а также на более частые экстренные и плановые госпитализации [61]. Например, исследование, проведенное в Канаде, показало, что каждое дополнительное хроническое заболевание увеличивает на 51% использование услуг врача [62]. Пожилые люди с полиморбидностью используют в 2–5 раз больше врачебных назначений, чем их сверстники без хронических заболеваний [63]. В настоящее время объем затрат на полиморбидных пациентов выходит за пределы возможностей страховщиков и государственного финансирования систем здравоохранения для отдельных пациентов, которые вынуждены покрывать расходы из своего кармана [64]. Например, затраты собственных средств в 2,1 раза выше у пожилых людей, страдающих множественными хроническими заболеваниями, чем у пациентов без полиморбидности [65]. Следует также отметить, что собственные расходы на лечение людей с полиморбидностью растут быстрее, чем рост доходов, что оказывает негативное влияние на жизнь наиболее уязвимых членов общества, особенно тех, кто не имеет адекватного медицинского страхования или не может получить доступ к универсальным системам здравоохранения [66].
Нехватка данных об экономической эффективности для обоснования выделения средств для решения проблемы полиморбидности является серьезным вызовом современному здравоохранению [67]. Тем не менее это не отменяет необходимость перераспределения ресурсов, чтобы попытаться остановить рост бремени полиморбидности, хотя и при отсутствии достаточной информации. Возможно, одним из лучших решений, как с точки зрения медицины, так и экономики, является курс, направленный на предотвращение развития множественных хронических заболеваний в самом начале [68]. С другой стороны, почти экспоненциальный рост стоимости медицинских услуг, связанных с дополнительными хроническими заболеваниями, может означать, что целевые мероприятия вторичной профилактики также следует считать важной стратегией для снижения бремени полиморбидности экономически эффективным способом [69, 70]. Возможно, что вторичная профилактика может иметь несколько большую эффективность (по сравнению с первичной профилактикой), когда она направлена на приоритетные клинические группы очень высокого риска [71].
Для повышения экономической эффективности медицинской помощи пациентам с полиморбидностью предложена еще одна тактика – «минимально разрушительной медицины» [72]. Она направлена на решение ключевых проблем здоровья пациента с минимально деструктивными вмешательствами, которые могли бы усугубить бремя болезни для пациента. Подоплека этой тактики заключается в том, что минимально разрушительное вмешательство может иметь больше шансов на приверженность пациента и, следовательно, будет более эффективным, чем вмешательства, несущие большую нагрузку для пациента [72]. Акцент на минимально разрушительное вмешательство может быть экономически эффективным подходом на системном уровне для обеспечения медицинской помощи пациентам с полиморбидностью в отличие от продвижения многих сложных, громоздких и потенциально дорогостоящих мер, которые не будут эффективны в связи с низкой приверженностью пациентов и их семей.
ЗАКЛЮЧЕНИЕ
Распространенность полиморбидности значительно растет в современном мире и охватывает почти четверть взрослого населения развитых стран. Старение является основным фактором риска для полиморбидности, кроме того, факторами риска являются женский пол и низкий социально-экономический статус. Полиморбидность связана не только с более высокими показателями смертности, но и с более высокими показателями инвалидности, с побочными эффектами лечения, с повышенным использованием ресурсов системы здравоохранения, а также с более низким качеством жизни. Понимание того, как эффективно лечить людей с множественными хроническими заболеваниями, является одной из наиболее сложных проблем, с которыми сталкивается наша система здравоохранения. Для решения этой проблемы необходимы клинические испытания, включающие больных с множественными хроническими заболеваниями, чтобы проверить эффективность и безопасность множественной лекарственной терапии. На основе этой информации должны быть разработаны новые клинические рекомендации, на которые могли бы опираться практические врачи при лечении полиморбидных пациентов. Ключевую роль в лечении таких пациентов играет семейный врач, но ему необходима поддержка мультидисциплинарной команды.
Организация медицинской помощи населению должна соответствовать проблемам современного мира, одной из которых является быстро растущая когорта пациентов с множественными хроническими заболеваниями.



