Несмотря на активное развитие и внедрение современных методов визуализации ишемии миокарда [1], наиболее распространенным диагностическим инструментом в повседневной клинической практике остается электрокардиография (ЭКГ). В то же время интерпретация изменений сегмента ST на фоне имеющихся нарушений внутрижелудочковой проводимости представляется трудно выполнимой задачей [2–4]. Наличие дискордантных изменений конечной части желудочкового комплекса у пациентов с полными внутрижелудочковыми блокадами объясняет необходимость поиска новых ЭКГ-маркеров преходящей ишемии миокарда, отличных от депрессии сегмента ST. В качестве таковых мы предлагаем рассмотреть дисперсию интервала QT (QTd) и дисперсию коррригированного интервала QT (QTcd).
QTd представляет собой один из ЭКГ-маркеров электрической неоднородности миокарда, определяемый как максимальная разность между значениями интервала QT в 12 отведениях [5]. Существенным преимуществом QTcd является устранение влияний частоты сердечных сокращений (ЧСС) на длительность электрической систолы, что позволяет с большей точностью оценить негомогенность процессов реполяризации желудочков [6]. Современные системы длительного мониторирования ЭКГ предоставляют возможность автоматического расчета показателей QTd и QTcd на протяжении всего периода регистрации ЭКГ-сигнала.
Целью настоящего исследования стала комплексная оценка параметров QTd и QTcd в покое на максимальной ЧСС, разности дисперсии интервала QT (QTdD), корригированного интервала QT (QTcdD) у пациентов с полными внутрижелудочковыми блокадами (QRS >120 мс), имеющих различную степень атеросклеротического поражения коронарного русла, а также у лиц с неизмененными коронарными сосудами.
МАТЕРИАЛ И МЕТОДЫ
В обсервационном исследовании приняли участие 112 пациентов с длительно существующими полными внутрижелудочковыми блокадами: 84 – с ранее перенесенным инфарктом миокарда и хронической сердечной недостаточностью (ХСН) с сохраненной фракцией выброса; 28 – без коронарного анамнеза, находившихся на стационарном лечении в кардиологических отделениях в 2017–2018 гг. Всем участникам было проведено холтеровское мониторирование ЭКГ с определением показателей QTd и QTcd в покое и на максимальных значениях ЧСС, а также диагностическая коронароангиография (КАГ).
С учетом результатов КАГ пациенты были разделены на четыре группы:
1 – однососудистое поражение коронарных артерий;
2 – двухсосудистое поражение;
3 – трехсосудистое поражение;
4 – отсутствие значимого коронарного атеросклероза (группа контроля).
Статистическая обработка данных проводилась в программе StatTech v. 1.2.0 («Статтех», Россия). Количественные показатели оценивались на предмет соответствия нормальному распределению с помощью критерия Шапиро–Уилка. Показатели, имеющие нормальное распределение, описывались через средние арифметические величины (M), стандартные отклонения (SD), а также 95% доверительный интервал (95% ДИ). В случае отсутствия нормального распределения количественные данные представлялись в виде медианы (Me), нижнего и верхнего квартилей (Q1–Q3). Сравнение четырех групп по количественному показателю, имеющему нормальное распределение, выполнялось посредством однофакторного дисперсионного анализа, апостериорные сравнения проводились с помощью критерия Тьюки (при условии равенства дисперсий). В случае если распределение количественного показателя отличалось от нормального, сравнение четырех групп выполнялось с применением критерия Краскела–Уоллиса, апостериорные сравнения – критерия Данна с поправкой Холма. Направление и теснота корреляционной связи между количественными и порядковыми показателями оценивались с использованием коэффициента ранговой корреляции (ρ Спирмена). Прогностическая модель, характеризующая зависимость числа пораженных сосудов от значений дисперсии, разрабатывалась на основе метода парной линейной регрессии. Различия считались статистически значимыми при p <0,05 (далее отмечены *).
РЕЗУЛЬТАТЫ
Нами был выполнен сравнительный анализ показателей QTd и QTcd в состоянии покоя в зависимости от количества коронарных сосудов, вовлеченных в атеросклеротических процесс (табл. 1).
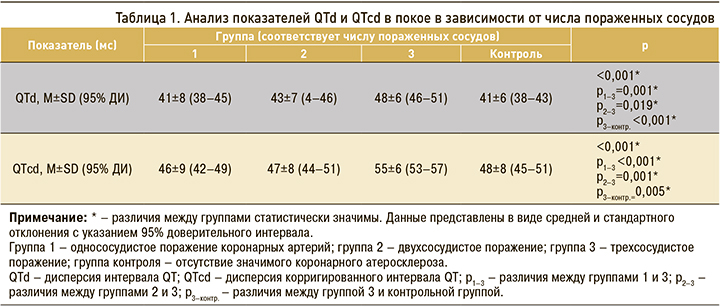
При сравнении показателей QTd и QTcd в покое в зависимости от группы нами были установлены статистически значимые различия (p <0,001 в обоих случаях). Наиболее высокие значения показателей регистрировались в случае многососудистого поражения коронарных артерий (группа 3).
 В ходе корреляционного анализа были выявлены прямые умеренные взаимосвязи значений QTd и QTcd в покое с числом пораженных сосудов (ρ=0,367 и ρ=0,423 соответственно; p <0,001).
В ходе корреляционного анализа были выявлены прямые умеренные взаимосвязи значений QTd и QTcd в покое с числом пораженных сосудов (ρ=0,367 и ρ=0,423 соответственно; p <0,001).
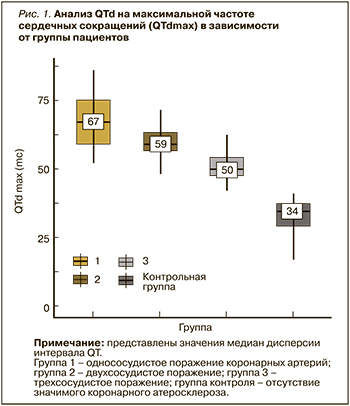
Далее нами был выполнен анализ показателей QTd и QTcd на максимальных значениях ЧСС в зависимости от распространенности коронарного атеросклероза (табл. 2, рис. 1 и 2).
При сравнении показателей QTd и QTcd на максимальных значениях ЧСС в зависимости от группы нами были установлены статистически значимые различия (p <0,001, p <0,001 соответственно). Максимальные значения показателей регистрировались в группе 1 (соответствует однососудистому поражению).
Результаты корреляционного анализа продемонстрировали наличие статистически значимой обратной взаимосвязи между значениями QTd на максимальной ЧСС и числом пораженных сосудов, так же как и между QTcd на максимальной ЧСС и числом пораженных сосудов (рис. 3 и 4). В обоих случаях корреляционная связь характеризовалась высокой теснотой по шкале Чеддока (ρ=-0,706 и ρ=-0,818 соответственно; p <0,001). Зависимость числа пораженных сосудов от QTcd на максимальной ЧСС описывалась уравнением парной линейной регрессии:
Y = 4,81 - 0,043 × XQTcd,
где Y – число пораженных сосудов (от 1 до 3), XQTcd – значение QTcd на максимальной ЧСС (мс).

В соответствии с коэффициентом детерминации R2 в модели был учтен 61% факторов, который оказывает влияние на суммарное количество сосудов, вовлеченных в атеросклеротический процесс.
Далее нами были проанализированы значения разности QTd на максимальной ЧСС и в покое (QTdD), а также разности QTсd на максимальной ЧСС и в покое (QTсdD) в изучаемых группах. Результаты сравнительного анализа отображены в таблице 3.
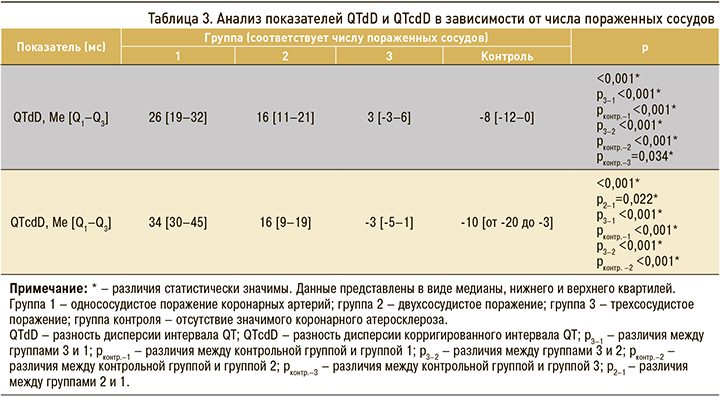
В ходе оценки параметров QTdD и QTcdD нами были установлены статистически значимые различия между группами (p <0,001 в обоих случаях). Наиболее высокие значения разности дисперсий регистрировались у пациентов с однососудистым поражением (медиана составила 26 мс для QTdD и 34 мс для QTcdD).
ОБСУЖДЕНИЕ
Перспективы использования параметров QTd и QTcd в неинвазивной диагностике ишемической болезни сердца (ИБС) неоднократно обсуждались в литературе. Результаты имеющихся на сегодняшний день исследований противоречивы и не распространяются на пациентов с полными внутрижелудочковыми блокадами – категорию лиц, у которых неприменимы стандартные ЭКГ-критерии преходящей ишемии миокарда [7–13].
В работе Demirtaş A.O. et al. был проведен сравнительный анализ показателей QTd в покое, на пике нагрузки и в восстановительный период у пациентов, направленных на КАГ для подтверждения ИБС. Результаты анализа указывали на существенно более высокие значения QTd у больных с выраженным коронарным атеросклерозом (в сравнении с лицами, имеющими незначимые атеросклеротические поражения сосудов; p <0,001). Показатели, оцененные в состоянии покоя, значимо не различались между группами. Пациенты с полной блокадой левой ножки пучка Гиса (ПБЛНПГ) не участвовали в исследовании [9].
Представляют интерес результаты небольшого ретроспективного исследования, опубликованного Stankovic I. et al., которые продемонстрировали сопоставимые значения QTcd в группах, сформированных с учетом количества вовлеченных в атеросклеротический процесс коронарных сосудов (однососудистое, двухсосудистое, трехсосудистое поражение, а также группа контроля). Однако в отличие от нашего исследования авторы ограничились определением QTcd по стандартной 12-канальной ЭКГ и соответственно не имели возможности оценить показатели на максимальной ЧСС (на пике нагрузки). Следует также обратить внимание, что в указанное исследование не включались пациенты с инфарктом миокарда и/или ПБЛНПГ [11].
В другой работе измерение интервала QT и расчет QTc, QTcd осуществлялись последовательно в покое и на пике физической нагрузки на тредмиле у пациенток с жалобами на боли в грудной клетке, без коронарного анамнеза и не имевших нарушений внутрижелудочковой проводимости на стандартной ЭКГ. Результаты сравнительного анализа продемонстрировали существенно более высокие значения вышеуказанных параметров на максимуме ЧСС в группах с однососудистым и особенно с многососудистым поражением в сравнении с контрольной группой (p <0,001) [10].
В работе Demir A.D. et al. оценка QTcd проводилась как по данным ЭКГ покоя, так и на фоне предсердной стимуляции. Авторы указывали на наличие прямой умеренной взаимосвязи между длительностью QTcd на максимальной ЧСС и числом пораженных коронарных артерий у пациентов с безболевой ишемией миокарда и нормальной внутрижелудочковой проводимостью (ρ=0,49; p <0,0001) [8]. В нашем исследовании вышеупомянутая корреляционная связь оказалась обратной, и соответственно максимальные значения параметра QTcd регистрировались у пациентов с однососудистым поражением. На наш взгляд, этот феномен может быть связан с выраженной электрической неоднородностью миокарда, обусловленной наличием как зоны локальной ишемии, усиливающейся на фоне нагрузки, так и адекватно кровоснабжаемыми участками миокарда у пациентов с изолированным поражением одной из коронарных артерий.
Ключевым отличием нашей работы от опубликованных ранее стала выборка пациентов: в исследовании был проведен анализ показателей дисперсии исключительно у больных с уширенными QRS-комплексами базового ритма, обусловленными внутрижелудочковыми блокадами. Следует отметить, что нами была найдена лишь одна работа (Calo L. et al., 1996) посвященная возможностям оценки QTd и QTcd на фоне ПБЛНПГ у 16 кардиологических больных [14]. В то же время дальнейшее изучение данной темы представляется перспективным и может способствовать совершенствованию алгоритмов ЭКГ-диагностики стабильной ИБС у лиц с внутрижелудочковыми блокадами.
К существенным ограничениям представленной работы следует отнести малый объем выборки, отсутствие оценки гемодинамической значимости стенозов коронарных артерий, а также влияния рассматриваемых параметров на прогноз, что будет учтено в последующих исследованиях.
ЗАКЛЮЧЕНИЕ
У пациентов с ИБС и полными внутрижелудочковыми блокадами значения показателей QTd и QTdc на максимальной ЧСС, а также QTdD и QTcdD существенно различаются в зависимости от распространенности коронарного атеросклероза, причем наиболее высокие значения, как правило, регистрируются при однососудистом поражении. Обнаружена высокая обратная корреляционная связь между QTd, а также QTcd на максимальной ЧСС и числом пораженных атеросклерозом сосудов. Получена регрессионная модель, описывающая зависимость распространенности коронарного атеросклероза от значений QTcd на максимальной ЧСС. В целом использование показателей QTd и QTcd открывает новые возможности в ЭКГ-диагностике стабильной ИБС у больных с полными внутрижелудочковыми блокадами.


