Головная боль напряжения (ГБН) относится к первичным цефалгиям, которые не связаны с органическим поражением центральной нервной системы (ЦНС), сосудов мозга, других структур, расположенных в области головы и шеи, системными заболеваниями [1]. По данным эпидемиологических исследований последних лет, ГБН стала не только самой распространенной формой головной боли, но и самым частым неврологическим заболеванием в мире [2].
Несмотря на международный опыт изучения ГБН у детей и подростков, до сих пор встречаются указания на то, что начало этого заболевания приходится на 3–4-е десятилетия жизни. Между тем дебют первичных форм головной боли, включая ГБН, нередко отмечается в детском или подростковом периоде, и начиная с возраста 7 лет прослеживается отчетливое увеличение частоты их встречаемости [3, 4].
ЭПИДЕМИОЛОГИЯ
ГБН страдают до 18–25 % детей и подростков [5, 6]. В дальнейшем распространенность заболевания возрастает: среди взрослого населения она достигает 30–80%, что сопряжено со значительными негативными социально-экономическими последствиями [7–9].
В 2015 г. началось глобальное исследование детской и подростковой головной боли и связанных с ней ограничений. Сбор данных и их интерпретация осуществляются в соответствии со стандартизированным протоколом [10] по меньшей мере в 20 странах мира. Вот лишь некоторые результаты этого исследования: в Турции среди детей и подростков ГБН была выявлена в 12,9% случаев [11], в Австрии – в 21,6% [12], в Литве – в 25,6% [13]. Тем самым подтверждено, что ГБН – наиболее распространенная форма первичных цефалгий в педиатрической популяции.
ПАТОФИЗИОЛОГИЯ И ПАТОГЕНЕЗ ГОЛОВНОЙ БОЛИ НАПРЯЖЕНИЯ
Патогенез ГБН является многофакторным [14–17] и включает периферические (мышечный спазм), центральные механизмы (центральную сенситизацию и дезингибицию), а также психологические факторы и конституционально-генетическую предрасположенность [18]. Доминирующую роль в формировании частых эпизодических и хронических ГБН играют центральные механизмы усиления боли, однако начальные звенья патогенеза ГБН связаны с напряжением перикраниальных мышц, возникающим в ответ на воздействие стресса [15–17]. В исследованиях подтверждена связь между интенсивностью стресса и частотой головной боли [19, 20]. У лиц, предрасположенных к сенситизации, стресс сопровождается неконтролируемыми миофасциальными феноменами и повышенной чувствительностью перикраниальной мускулатуры. Сложный комплекс механизмов патогенеза ГБН нашел отражение в ранее применявшихся ее обозначениях, таких как «головная боль мышечного напряжения», «психомиогенная головная боль», «психогенная головная боль», «стрессорная головная боль» и ряде других терминов, которые иллюстрируют значимую роль психологических факторов в развитии ГБН [21–23]. Повышенная возбудимость ЦНС из-за повторяющейся и продолжительной перикраниальной миофасциальной импульсации постулируется как возможная причина эпизодических ГБН и их перехода в хронические [24].
Характерным симптомом при физикальном обследовании пациентов с ГБН выступает повышенная болезненность при пальпации перикраниальных миофасциальных тканей. Электромиографические исследования показали, что у больных наблюдается снижение релаксации перикраниальных мышц в покое [23]. В основе формирования мышечно-тонического синдрома лежит механизм «порочного круга», когда повторяющееся напряжение мышцы, появляющееся в ответ на стресс, приводит к рефлекторному напряжению и ишемизации мышцы, перевозбуждению спинальных нейронов, повышению чувствительности болевых рецепторов мышцы, позным нарушениям и еще большему усилению боли [7, 9]. Считается, что активация периферических перикраниальных миофациальных ноцицепторов в основном ответственна за эпизодические ГБН, а сенситизация болевых путей в ЦНС приводит к трансформации эпизодических ГБН в хронические [23].
ГБН относят к классу дисфункциональных болей, учитывая ее обусловленность изменением функционального состояния отделов ЦНС, участвующих в контроле боли, и появлением таких патофизиологических маркеров патологической боли, как периферическая и центральная сенситизация, функциональная недостаточность антиноцицептивных образований. Основное отличие дисфункциональных болей от двух других типов боли – ноцицептивной (соматогенной, соматической) и нейропатической (нейрогенной) – состоит в невозможности выявления ее непосредственной причины и органического поражения структур нервной системы. Основные факторы, влияющие на развитие дисфункциональной боли (эмоциональные и социально-психологические), способствуют дисфункции нейромедиаторных систем мозга (норадренергической и серотонинергической), в результате чего обычные неболевые стимулы начинают восприниматься как боль [14, 25]. Данный феномен описал Barsky A.J. [26], обозначив его «соматосенсорная амплификация».
Влияние психологического статуса пациента на развитие ГБН реализуется посредством изменения состояния лимбико-ретикулярного комплекса, задействованного в регуляции вегетативных функций, мышечного тонуса, восприятия боли через общие нейромедиаторные механизмы [17, 21, 22]. Феномен центральной сенситизации характеризуется тем, что после длительной периферической ноцицептивной стимуляции сохраняется определенный уровень возбуждения в чувствительных нейронах ЦНС; это поддерживает боль даже при отсутствии периферической патологии [14]. Данная сенситизация, вероятно, потенцируется за счет нарушений супраспинального и супрануклеарного торможения ноцицептивной передачи, что ведет не только к снижению порога возбуждения ноцицептивных нейронов, но и увеличению количества клеток, участвующих в обработке болевого сигнала на спинальном и стволовом уровне [15, 27]. В результате значительно возрастает афферентная импульсация с расширенных рецептивных полей, что влечет за собой сенситизацию нейронов таламуса и сенсорной коры.
Центральные механизмы значимы при хронической ГБН, при которой выявляется общая гиперчувствительность к болевым стимулам [27]. Получены данные о существенном уменьшении серого вещества в областях мозга, участвующих в ноцицептивной передаче, у пациентов с хронической ГБН в исследованиях с применением магнитно-резонансной томографии (МРТ) на основе воксельной морфометрии [24, 28]. Эти изменения относились к коре передней поясной извилины, островку, орбитофронтальной коре, парагиппокампальной извилине, дорсальным и ростральным отделам моста. Данное уменьшение положительно коррелировало с длительностью головной боли, что может свидетельствовать о структурных изменениях, являющихся следствием центральной сенситизации [28].
При длительно существующем болевом синдроме страдают функции глии (астроцитов и микроглии), и это потенцирует выработку провоспалительных цитокинов и хемокинов, высокие уровни которых обнаружены у пациентов с ГБН [29]. При этом повышается тонус ноцицептивного рецепторного аппарата, облегчается действие глутамата на NMDA-рецепторы и последующий биохимический каскад, вызывающий повышение проницаемости мембран для кальция и накопление кальция внутри клеток [15]. Развивается реакция по типу нейрогенного воспаления, которая сопровождается вазодилатацией, выходом в интерстиций химических медиаторов и белков плазмы, высвобождением медиаторов боли – оксида азота, серотонина, брадикинина, калия, субстанции Р, гистамина [29–31]. В результате этих нейрохимических и патофизиологических механизмов снижается порог возбудимости, возникают такие патологические реакции, как гипералгезия и аллодиния.
В исследовании Bougea A. et al. [29] показан повышенный уровень интерлейкина-1β в слюне у пациентов с ГБН в период приступа головной боли. Одна из возможных теорий иктального увеличения количества провоспалительных цитокинов заключается в том, что миофасциальная боль активирует высвобождение медиаторов воспаления, стимулирующих афферентные периферические нервы. Согласно другой гипотезе, спиноретикулоталамический тракт может быть активирован периферическими импульсами, что приводит к увеличению выхода кортикотропин-рилизинг-гормона, вазопрессина и бета-эндорфина, которые способствуют выработке кортизола, запускающего высвобождение периферических цитокинов [29].
К числу провоцирующих ГБН факторов, наряду с влиянием эмоционального стресса, относятся выраженная тревога, переутомление и астенизация, вынужденное голодание, зрительное напряжение (при нарушениях зрения вследствие длительного пребывания за компьютером), а также нефизиологические позы (долгая работа в статических, неудобных позах за столом, с избыточным напряжением мышц шеи, спины, глаз), депривация сна, неудобное положение головы во время сна [5, 17, 30, 32, 33]. Нарушения зрения, связанные с аномалиями рефракции, неудобные положения головы, нефизиологические позы приводят к активации периферических (сегментарно-рефлекторных) факторов, при которых потоки болевой импульсации первоначально определяются локальными причинами.
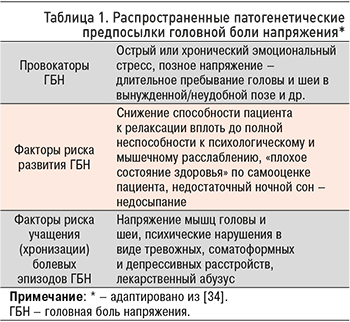 Различные группы распространенных патогенетических предпосылок ГБН суммированы в таблице 1.
Различные группы распространенных патогенетических предпосылок ГБН суммированы в таблице 1.
Необходимо отметить, что причины ГБН следует анализировать с учетом возраста пациента, особенно в случае с детьми и подростками. Основными провоцирующими факторами для развития ГБН у ребенка считаются тревожность и наличие клинически значимой психотравмирующей ситуации, трудности адаптации к новой обстановке, неспособность к психологическому и мышечному расслаблению, расстройства сна, что приводит к нарушению функционального состояния лимбико-ретикулярного комплекса [5, 22, 27, 32]. Это сопровождается дизрегуляцией ноци- и антиноцицептивной систем, нарушением функционального состояния, в том числе системы тройничного нерва. В результате возникают спазм и болевая ишемия перикраниальных мышц [21].
Патофизиологической особенностью ГБН у детей является незрелость механизмов психологической защиты, что обусловливает проявление заболевания при воздействии незначительных, с точки зрения взрослых, стрессовых воздействий. Под влиянием психотравмирующих ситуаций формируются тревожные расстройства (фобическое тревожное расстройство, генерализованное тревожное расстройство, социальная фобия) [4, 5, 22, 32]. Эти ситуации приводят к неконтролируемым миофасциальным феноменам, тоническому напряжению перикраниальных мышц.
В исследованиях последних лет подтверждена нейробиологическая основа ГБН, а патогенез заболевания связывают с комбинацией факторов, которые включают влияние стресса у предрасположенных лиц, периферические (мышечный спазм) и центральные механизмы (центральную сенситизацию и дезингибицию) [5, 35].
КЛИНИЧЕСКИЕ ПРОЯВЛЕНИЯ И КЛАССИФИКАЦИЯ ГОЛОВНОЙ БОЛИ НАПРЯЖЕНИЯ
ГБН – легкая или умеренная, повторяющаяся двусторонняя ГБ сжимающего или давящего характера, которая имеет значительную продолжительность. Длительность приступа может варьироваться от 30 мин до нескольких дней (с некоторым колебанием интенсивности боли), но менее недели. ГБН может сопровождаться свето- или звукобоязнью (но не обоими этими признаками сразу), не усиливается под влиянием повседневной физической активности и не сопровождается рвотой [4, 5, 7, 22, 34–37].
Боль при ГБН описывается пациентами как постоянная, давящая. В большинстве случаев она локализуется в области лба, висков с иррадиацией в затылочную область и заднюю поверхность шеи, затем может становиться диффузной и описывается как ощущение сжатия головы обручем (симптом «шлема, каски»). Хотя головная боль обычно бывает двусторонней и диффузной, локализация ее наибольшей интенсивности в течение дня может попеременно переходить с одной половины головы на другую. Стойкая односторонняя головная боль (гемикрания), как правило, связана с повышенной чувствительностью перикраниальной мускулатуры [5, 37]. У детей и подростков головная боль обычно появляется днем (после 2–3-го урока) или во второй половине дня и продолжается до вечера. Может она возникать и утром, после пробуждения, если отмечалась накануне вечером. У больных могут наблюдаться различные временные паттерны течения ГБ – от редких, кратковременных эпизодических приступов с длительными ремиссиями, до волнообразного течения, характеризующегося длительными периодами ежедневных головных болей, чередующимися с кратковременными ремиссиями [4, 22, 37]. Транзиторные неврологические симптомы для ГБН не характерны.
Варианты ГБН, в зависимости от частоты приступов в соответствии с Международной классификации головных болей 3-го пересмотра (МКГБ), приведены в таблице 2.

В зависимости от наличия мышечной дисфункции различают ГБН с напряжением и без напряжения перикраниальных мышц. Для выявления напряжения перикраниальной мускулатуры и определения «триггерных» точек проводится пальпация височной, лобной, затылочных областей, мышц задней поверхности шеи, трапециевидной и грудино- ключично-сосцевидных.
Согласно диагностическим критериям МКГБ- III [1], ГБН не усиливается от рутинной физической нагрузки, интенсивность ее обычно слабая или умеренная. Между тем клинические проявления ГБН у детей и подростков могут иметь индивидуальные особенности. Так, по данным Dura Trave T. и Yoldi Petri M.E. [38], у большинства детей ГБН были двусторонними (81,8%) и давящими (85,3%), но могли усиливаться от физической нагрузки (11,8%), иногда сопровождались тошнотой (7,3%), фото-фонофобией (21,8%).
В отличие от взрослых, у детей продолжительность приступов ГБН может составлять как 5–30 мин, так и более 48 ч. По данным Gallai V. et al. [39], у 36,7% детей с ГБН продолжительность приступов составляет менее 30 мин. По наблюдениям Н.Ю. Будчановой с соавт. [40], наиболее специфичными характеристиками ГБН у детей и подростков оказались локализация и интенсивность боли. При этом интенсивность ГБН у детей увеличивалась при трансформации эпизодических вариантов из редких в частые с 4,41 до 5,09 балла (p >0,05), из эпизодических в хронические – с 5,09 до 5,61 балла (p >0,05) [40].
Для маленьких детей, которым трудно объяснить локализацию головной боли, наиболее значимой ее характеристикой для дифференцирования ГБН и мигрени становится критерий интенсивности. В то же время локализация головной боли зачастую недостаточно специфичный диагностический критерий в детской популяции [4, 37].
Согласно рекомендациям Американской академии неврологии и общества детских неврологов [41], включение методов нейровизуализации в комплекс обследования пациентов с повторяющимися головными болями и отсутствием изменений в неврологическом статусе, примером которых как раз является ГБН, нецелесообразно. Проведение электроэнцефалографии детям с повторяющимися головными болями (прежде всего первичными) также неоправданно, поскольку выяснение этиологии боли с помощью этого метода маловероятно [41]. Лабораторные и инструментальные исследования показаны только при решении вопросов дифференциального диагноза и подозрении на симптоматический характер головной боли [4, 5, 36, 37].
КОМОРБИДНЫЕ РАССТРОЙСТВА ПРИ ГОЛОВНОЙ БОЛИ НАПРЯЖЕНИЯ
Пациенты с ГБН обращаются за помощью не только к неврологам, но и врачам других специальностей в связи с разнообразием соматических жалоб и нарушений в эмоциональной сфере [17, 23]. Для них характерны вегетативные нарушения и эмоциональные расстройства (в основном тревожные, в ряде случаев депрессивные), нередко протекающие в «маскированных» формах. Эти проявления в соматической и психоэмоциональной сферах нередко затрудняют диагностику и выбор адекватного лечения [9, 22, 34]. Одновременно эмоциональные нарушения у пациентов с ГБН усиливают трудности их социально-психологической адаптации [42].
В межприступном периоде, в отличие от мигрени, большинство пациентов с ГБН предъявляет жалобы соматоформного типа на боли и чувство дискомфорта в других органах (боли в ногах, кардиалгии, затруднения дыхания при вдохе, глотания, дискомфорт в животе), которые характеризуются непостоянством и достаточно неопределенным характером, однако при клиническом и инструментальном обследовании патологические изменения не определяются [37].
ГБН у детей и подростков нередко приводит к ухудшению социальной и академической деятельности, что может быть связано с проявлениями сопутствующих (коморбидных) расстройств. Обращает на себя внимание высокая частота встречаемости церебрастенического синдрома у пациентов с ГБН [43]. Одним из его основных признаков считается так называемая раздражительная слабость, для которой характерны общая пассивность, вялость, медлительность в мышлении и движениях, повышенная утомляемость, истощаемость, снижение фона настроения даже при незначительных нервно-психических нагрузках. При интеллектуальных нагрузках отмечаются истощаемость внимания и мышления в сочетании со снижением психической работоспособности и оперативной памяти. С другой стороны, нередко имеют место повышенная раздражительность, готовность к аффективным вспышкам, недостаточная критичность [37, 43].
Среди предикторов ГБН в детском возрасте называются нарушения концентрации внимания, медленный темп когнитивной деятельности, эмоциональная нестабильность, гиперактивность, напряженные отношения в школе [44]. По данным популяционного исследования Strine T.W. et al. [45], включавшего детей и подростков 4–17 лет, у тех из них, которые страдали частыми головными болями, в 2,6 раза чаще наблюдались нарушения внимания и гиперактивность. Genizi J. et al. [46] обследовали группу из 243 детей в возрасте 6–18 лет с первичными головными болями, из них у 44% (n=107) была диагностирована мигрень и у 47,7% (n=116) – ГБН. Анализ психоневрологических нарушений у этих детей, выявленных до обращения и проведения обследования по поводу головной боли, показал, что в связи с синдромом дефицита внимания и гиперактивности (СДВГ) наблюдались 28% детей с первичными головными болями. СДВГ чаще отмечался у пациентов с ГБН, чем с мигренью (36,5 против 19,8%; p=0,006). При этом трудности школьного обучения отмечались у 24,7% пациентов с первичными головными болями. Таким образом, как СДВГ, так и трудности школьного обучения чаще обнаруживались среди пациентов с первичными головными болями, чем в детской популяции.
По результатам исследования, в котором оценивалась ассоциация между СДВГ и первичными головными болями, сделан вывод о том, что мигрень и ГБН коморбидны не с СДВГ как таковым, а с гиперактивно-импульсивным поведением [47]. С другой стороны, в исследованиях Riva D. et al. [48] продемонстрирована ассоциация между расстройствами внимания у детей и обоими основными типами первичных головных болей – мигренью и ГБН. Высказывается предположение о том, что мигрень и ГБН формируют континуум, который может иметь некоторые общие патофизиологические механизмы, а комплексы мозговых структур, обеспечивающие механизмы внимания, особенности профиля личности и механизмы головной боли, могут перекрываться [46].
Интересны результаты исследований, в которых обнаружена более высокая частота встречаемости СДВГ среди пациентов с ГБН по сравнению с мигренью [46]. По-видимому, связанные с СДВГ трудности школьного обучения и проблемы поведения, которые сопровождаются длительными и многочисленными стрессами в семье, школе, взаимоотношениях со сверстниками и другими людьми, через влияние повторяющихся стрессов способствуют формированию ГБН.
По данным Е.М. Шипиловой [49], наиболее распространенными коморбидными состояниями у детей и подростков с ГБН в возрасте 8–16 лет выступают тревожные расстройства: они были диагностированы у большинства – 109 (72,7%) из 150 обследованных пациентов, что в несколько раз превышает среднепопуляционные значения. Чаще тревожные расстройства встречались среди детей и подростков с хроническими ГБН – 48 случаев (81,4%) из 59, чем с частыми эпизодическими ГБН – 61 (67,0%) из 91 (р <0,05). При этом у пациентов с ГБН в сочетании с тревожными расстройствами (по сравнению с пациентами с ГБН без коморбидных эмоциональных и поведенческих расстройств) обнаружены значимо более высокие показатели частоты ГБН и ее негативного влияния на повседневную активность; одновременно прослеживалась тенденция к увеличению средней продолжительности и интенсивности приступов головной боли [49].
У большинства детей и подростков с ГБН обнаруживаются нарушения сна. Известно, что дизрегуляция сна служит триггером эпизодических ГБН и может осложнять и утяжелять их течение, способствуя переходу в хроническую форму [50]. Существует взаимосвязь между эмоциональными нарушениями и расстройствами сна: последние входят в число диагностических критериев тревожных расстройств и депрессии. По данным литературы, у многих пациентов с ГБН выявляются инсомния, дневная сонливость, снижение субъективного качества сна [51]. При оценке по шкале нарушения сна [49] у детей и подростков с ГБН с высокой частотой обнаружены различные по степени выраженности (клинически значимые и пограничные) инсомнические расстройства (у 60,4% пациентов с частыми эпизодическими ГБН и 72,9% с хроническими ГБН), чрезмерная сонливость (67,1 и 86,4% соответственно), нарушения дыхания во время сна (23,1 и 32,2% соответственно), расстройства пробуждения (42,9 и 50,8% соответственно), расстройства перехода «сон–бодрствование» (67,1 и 62,7% соответственно), ночной гипергидроз (26,4 и 39,0% соответственно). Все виды расстройств сна (за исключением расстройств перехода «сон–бодрствование») значительно чаще встречались у пациентов с хроническими ГБН.
При выборе тактики лечения детей и подростков с ГБН необходимо уделять особое внимание диагностике сопутствующих нарушений и принимать меры для их коррекции. Поэтому при проведении лечения ГБН не следует ограничиваться только купированием цефалгического синдрома; целесообразно применять терапевтические средства, обладающие комплексным действием на ЦНС, различные патогенетические механизмы ГБН и сопутствующих им расстройств.
МЕТОДЫ ЛЕЧЕНИЯ И ПРОФИЛАКТИКИ ГОЛОВНОЙ БОЛИ НАПРЯЖЕНИЯ
Для профилактики ГБН может применяться комплекс мер, включающий различные рекомендации по физической активности, режиму питания и образу жизни, который обозначается англоязычной аббревиатурой SMART (от начальных букв слов Sleep, Meals, Activity, Relaxation, Trigger). Он подразумевает достаточный и качественный сон, регулярное здоровое питание, адекватную физическую активность, применение методов релаксации, распознавание и исключение триггеров [52]. Важной частью лечения служит разъяснение пациенту в доступной для него форме природы ГБН, в том числе роли эмоциональных факторов и перенапряжения перикраниальных мышц, рекомендаций по исключению факторов, провоцирующих головную боль, режиму питания и гигиене сна, регулярной оздоровительной физической нагрузке, а также обучение методикам психологической и мышечной релаксации. Поскольку к ГБН может привести неправильное положение головы во время ночного сна, следует обратить внимание на «удобство» подушек и постели.
Лечение ГБН следует начинать с обнаружения и устранения ситуации хронического стресса [37]. У ребенка с ГБН не всегда сразу удается выявить хроническую психотравмирующую ситуацию, но если она обнаружена (развод родителей, конфликтная ситуация в школе, физическая или психологическая агрессия и др.), то лечение должно начинаться с мер по устранению психотравмирующей ситуации. Поэтому целесообразны занятия с психологом или психотерапевтом для выработки стратегии поведения в стрессовой ситуации, уменьшения выраженности тревожности и формирования позитивного образа мышления.
Хорошим эффектом в профилактике ГБН обладают немедикаментозные подходы [16, 35, 37, 52], к которым относятся методы, направленные на уменьшение выраженности мышечно-тонического синдрома: когнитивно-поведенческая терапия, аутогенная тренировка, постизометрическая мышечная релаксация, массаж воротниковой зоны, водные процедуры.
Поскольку для современных школьников характерно повышение умственных и психоэмоциональных нагрузок в сочетании с ограничением двигательной активности, для профилактики ГБН рекомендуются регулярные оздоровительные физические нагрузки (преимущественно аэробные). С учетом этого заслуживает внимания дыхательная гимнастика А.Н. Стрельниковой, особенностью которой является использование форсированного вдоха и вовлечение самой мощной дыхательной мышцы – диафрагмы. Упражнения включают тренировку короткого, резкого, шумного вдоха через нос с частотой приблизительно 3 вдоха за 2 секунды с последующим пассивным выдохом через нос или через рот [53]. Активная работа всех частей тела – ног, рук, головы, брюшного пресса, тазового, плечевого пояса – в совокупности с выполнением коротких и резких вдохов через нос при пассивном выдохе вызывает общую физиологическую реакцию, приводит к усилению внутреннего тканевого дыхания и повышению усвояемости кислорода тканями [53].
В соответствии с современными рекомендациями [35–37, 52, 54], в рамках лекарственной терапии ГБН применяются средства как для купирования, так и профилактики головной боли. Симптоматическое лечение безрецептурными анальгетиками может применяться у пациентов с эпизодической ГБН, при частоте болевых эпизодов не более 2 раз в неделю. Использование анальгетиков должно быть однократным или проводиться короткими курсами при длительных приступах головной боли. При этом необходимо помнить о недопустимости злоупотребления обезболивающих препаратов. Прием более сильных анальгетиков или комбинации анальгетиков с мышечными релаксантами значительной эффективностью не обладает, однако вызывает нежелательные симптомы со стороны желудочно-кишечного тракта. Детям для обезболивания рекомендуется использовать парацетамол (разовая доза 10–15 мг/кг, максимальная суточная доза не более 60 мг/кг массы тела) или ибупрофен (разовая доза 5–10 мг/ кг, максимальная суточная доза не более 30 мг/кг, интервал между приемами 6–8 ч). При эпизодической ГБН, с частотой более 2 дней в неделю, профилактическая терапия предпочтительнее купирования приступов. При хронической ГБН обезболивающие лекарственные средства обладают сомнительной эффективностью и повышают риск развития лекарственно-индуцированной головной боли [37, 54].
Возможности фармакотерапии при профилактическом лечении частых эпизодических и хронических ГБН у детей и подростков ограничены в связи малым числом проведенных клинических исследований [4, 55].
Имеются подтверждения эффективности профилактических курсов трициклического антидепрессанта амитриптилина при частых эпизодических и хронических ГБН у детей и подростков [55]. Механизм его антидепрессивного действия связан с повышением концентрации норадреналина в синапсах и/или серотонина в ЦНС за счет угнетения обратного нейронального захвата этих медиаторов. Эффект антидепрессантов при первичных головных болях обусловлен их собственным противоболевым действием вследствие усиления активности антиноцицептивных систем [7]. Амитриптилин обладает определенным анальгезирующим эффектом, предположительно связанным с изменениями концентраций моноаминов в ЦНС, особенно серотонина, и влиянием на эндогенные опиоидные системы. Отмечается, что анальгетический эффект антидепрессантов наступает раньше и при приеме меньших доз, чем собственно антидепрессивное действие [9].
Обоснование применения амитриптилина и некоторых других антидепрессантов для профилактической терапии частых ГБН у детей основано на положительных результатах клинических исследований, показавших их эффективность у взрослых пациентов с ГБН [35, 54]. Детям и подросткам рекомендуется начинать терапию амитриптилином с малых доз (5–10 мг или 0,25 мг/кг массы тела) перед сном. В зависимости от ответа дозировку можно увеличивать каждые 2–3 нед на 0,25 мг/ кг до максимальной дозы 1 мг/кг в день [36, 37]. Побочные эффекты амитриптилина включают ортостатическую гипотензию и антихолинергические эффекты [55], в том числе сухость во рту, седацию, запоры и нечеткость зрения. Около четверти пациентов отмечают увеличение массы тела [9]. При назначении доз выше 30–40 мг/сут часто возникает дневная сонливость, даже когда прием препарат осуществляется перед сном. Кроме того, при назначении амитриптилина необходим контроль электрокардиограммы для исключения нарушений проводимости.
В исследовании Grazzi L. et al. [56] сравнивалась эффективность 3-месячных курсов лечения пациентов с ГБН в возрасте 8–16 лет с применением расслабляющих тренингов и фармакотерапии амитриптилином, назначавшимся ежедневно по 10 мг/сут. Клиническое улучшение было достигнуто в обеих группах. В группе лечившихся амитриптилином исходная частота ГБН составляла 17±11 приступов в месяц, через 3 мес терапии данный показатель снизился до 5,6±6,7. Эти результаты оказались сопоставимы с группой, в которой проводились расслабляющие тренинги: в ней первоначальная частота приступов 12,1±10,1 в месяц и уменьшилась до 6,4±9,6.
Представляется перспективным изучение эффективности в профилактическом лечении ГБН у детей и подростков лекарственных средств с комплексным анксиолитическим и ноотропным эффектами. Нами было проведено открытое рандомизированное сравнительное исследование в трех параллельных группах пациентов продолжительностью 2 мес, посвященное оценке эффективности монотерапии аминофенилмасляной кислоты гидрохлоридом, амитриптилином или дыхательной гимнастикой (группа сравнения) в рамках профилактической терапии ГБН у детей и подростков [57]. В ходе открытого параллельного исследования 90 пациентов с ГБН в возрасте 8–16 лет были распределены на три группы по 30 человек (в каждой по 15 пациентов мужского и женского пола).
В исследовании были подтверждены достоверные различия с группой сравнения по индивидуальному ответу на терапию. По такому критерию, как уменьшение среднего числа приступов ГБН за месяц на 50% и более, в 1-й группе (аминофенилмасляной кислоты гидрохлорид) улучшение было достигнуто у 56,7% пациентов, во 2-й (амитриптилин) – у 73,3%, в группе сравнения (дыхательная гимнастика) – у 30%. По более строгому критерию – уменьшение среднего числа приступов ГБН за месяц на 75% и более – ответ на терапию наблюдался в 1-й группе у 30%, во 2-й группе – у 23,3%, в группе сравнения – у 3,3% пациентов. В 1-й и 2-й группах, наряду со значимым уменьшением на фоне лечения частоты приступов ГБН, их продолжительности и интенсивности, было обнаружено существенное улучшение повседневной активности, благоприятное влияние терапии на сопутствующие ГБН проявления церебрастенического синдрома, тревожных расстройств и нарушений сна.
Одновременно было установлена терапевтическая эффективность в профилактике ГБН комплекса упражнений дыхательной гимнастики. Она проявлялась в сокращении частоты, продолжительности и интенсивности ГБН, а также снижении влияния ГБН на повседневную активность, умеренном уменьшении выраженности проявлений церебрастенического синдрома, тревожных расстройств по самооценкам пациентов и улучшении показателей сна.
ЗАКЛЮЧЕНИЕ
Таким образом, важным аспектом эффективного лечения ГБН является правильная постановка диагноза, основанная на особенностях клинической картины, определении коморбидных расстройств и рациональном выборе терапии с применением как немедикаментозных методов, так и лекарственных препаратов. Высокая частота встречаемости коморбидных тревожных и поведенческих расстройств среди детей и подростков с ГБН определяет потребность в дополнительном применении психотерапевтических методов при оказании комплексной помощи этим пациентам. Лечение коморбидных расстройств в дополнение к терапии ГБН у детей и подростков может способствовать улучшению прогноза заболевания и показателей качества жизни, а также уменьшению потребности в анальгетиках для лечения самих головных болей.
Ранняя и точная диагностика ГБН у детей и подростков дает возможность оптимизировать терапевтическую программу, организовать психолого-педагогическую помощь, улучшить прогноз и снизить риск развития хронической формы заболевания.