ВВЕДЕНИЕ
Хроническая обструктивная болезнь легких (ХОБЛ) – предотвратимое и поддающееся лечению гетерогенное заболевание, в основе которого лежат стойкие респираторные симптомы с ограничением воздушного потока за счет изменения структуры дыхательных путей и/или альвеол по причине регулярного или значительного воздействия вредных частиц или газов [1].
Распространенность ХОБЛ достаточно велика: по данным международного исследования Burden of Obstructive Lung Disease (BOLD), частота выявления этого заболевания составляла 11,2% у мужчин и 8,6% у женщин в возрасте от 40 лет [2]. В России, согласно результатам мультицентрового исследования, опубликованного в 2014 г., встречаемость ХОБЛ в общей популяции достигала 15,3% [3].
ХОБЛ – заболевание с выраженным системным компонентом, характеризующееся высокой частотой коморбидных расстройств. Вовлечению в патологический процесс различных органов и систем способствуют хроническая гипоксия, системное воспаление, легочная гипертензия с развитием правожелудочковой сердечной недостаточности и другие патогенетические механизмы.
Нарушение венозной циркуляции при ХОБЛ также имеет патогенетическое обоснование: помимо сердечной недостаточности, расстройству венозного оттока способствует ослабление присасывающего действия грудной клетки, повышение внутригрудного давления вследствие формирования воздушной ловушки и внутрибрюшного давления при затруднении выдоха. Известно, что наличие ХОБЛ в анамнезе влияет на выраженность и течение варикозной болезни, частоту тромбозов глубоких вен нижних конечностей, тромбоэмболии легочной артерии [4–7]. Венозная дисциркуляция зачастую носит системный характер [8], и при наличии указанных патогенетических механизмов можно ожидать также и нарушения венозного оттока из полости черепа, особенно при обострении обструктивной болезни. Некоторые авторы указывают на значительный вклад нарушения венозного оттока в формирование энцефалопатии при ХОБЛ [9–11], однако степень выраженности церебральной венозной дисциркуляции, ее зависимость от тяжести и фенотипического варианта обструктивной болезни, а также связь с клиническими симптомами остаются недостаточно изученными.
В связи с этим целью нашего исследования стала клинико-инструментальная оценка наличия и выраженности церебральной венозной дисциркуляции у пациентов с ХОБЛ в стадии обострения.
МАТЕРИАЛ И МЕТОДЫ
Проведенное исследование носило характер наблюдательного («случай–контроль»). Исследование прошло этическую экспертизу на базе ФГБОУ ВО «Московский государственный медико-стоматологический университет им. А.И. Евдокимова» Минздрава России в 2018 г.
Было обследовано 100 пациентов, поступивших в стационар по поводу обострения ХОБЛ. В качестве группы контроля выступили 50 пациентов неврологического отделения стационара, проходивших лечение с диагнозом «дорсопатия». От всех пациентов было получено информированное согласие на участие в исследовании.
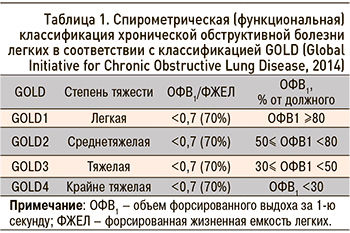
В основную группу исследования включались пациенты с установленным диагнозом ХОБЛ и тяжестью заболевания по данным исследования функции внешнего дыхания GOLD1 или GOLD3 (согласно Спирометрической классификации рекомендаций GOLD 2014 г. пересмотра – табл. 1).
В исследование не включались пациенты, перенесшие за последние два месяца хирургические операции, острое нарушение мозгового кровообращения или инфаркт миокарда, а также больные, принимавшие на момент поступления венотонические препараты.
Среди 150 человек, вошедших в исследование, было 63 женщины и 87 мужчин. Возраст участников составил от 23 до 72 лет (в среднем 59 лет).
Пациенты в основной группе были достоверно старше (в среднем 63±5,8 лет), чем в контрольной. По половому составу, частоте атеросклероза, гипертонической болезни, сахарного диабета группы достоверно не различались. 44 пациента с ХОБЛ имели «бронхитический» фенотип заболевания (что предполагает преимущественно бронхиолит в качестве основного патогенетического звена повреждения легких), 56 – «эмфизематозный» подтип (преобладание деструкции легочной паренхимы).
Всем пациентам был проведен тщательный клинико-неврологический осмотр. Отдельно фиксировались жалобы, которые, согласно литературным данным, могут быть характерны для вероятной церебральной венозной дисциркуляции: утренняя головная боль давящего, распирающего характера [12], ощущение резкой сонливости, дурноты, «очумелости» после пробуждения, проходящие после вертикализации и начала утренней активности (далее объединены в группу жалоб «трудности при пробуждении»), пастозность лица и век в утреннее время [13], дневная сонливость. Также особое внимание уделялось выявлению расширения вен переорбитальной и височной области, отеков век, признаков возможной венозной патологии других локализаций (варикозная болезнь и/или перенесенные тромбозы вен нижних конечностей, геморрой, варикоцеле).
Всем участникам исследования (в том числе из контрольной группы) выполнялись оценка функции внешнего дыхания, кардиореспираторный мониторинг, бодиплетизмография, дуплексное сканирование брахиоцефальных артерий с дополнительной оценкой кровотока по яремным венам, позвоночным венозным сплетениям, глазничным венам. Врачам, проводившим ультразвуковое допплеровское обследование, не сообщалось о наличии у больного ХОБЛ и ее тяжести. Пульсирующий венозный поток оценивался по максимальной скоростной составляющей.
Необходимо отметить, что, хотя ультразвуковые сосудистые исследования осуществлялись в первой половине дня (до 12 ч), лишь незначительная часть из них была выполнена в первые 30 мин после пробуждения, как это рекомендуется при утренних симптомах [13]
Особенностью исследования функции внешнего дыхания стало то, что при ОФВ1 более 80% точное значение этого показателя не определялось (в силу особенностей использовавшейся аппаратуры). Таким образом, в контрольной группе все значения ОФВ1 были обозначены как ≥80%, а индексы, использующие этот показатель, в том числе ОФВ1/ ЖЕЛ, не вычислялись.
РЕЗУЛЬТАТЫ
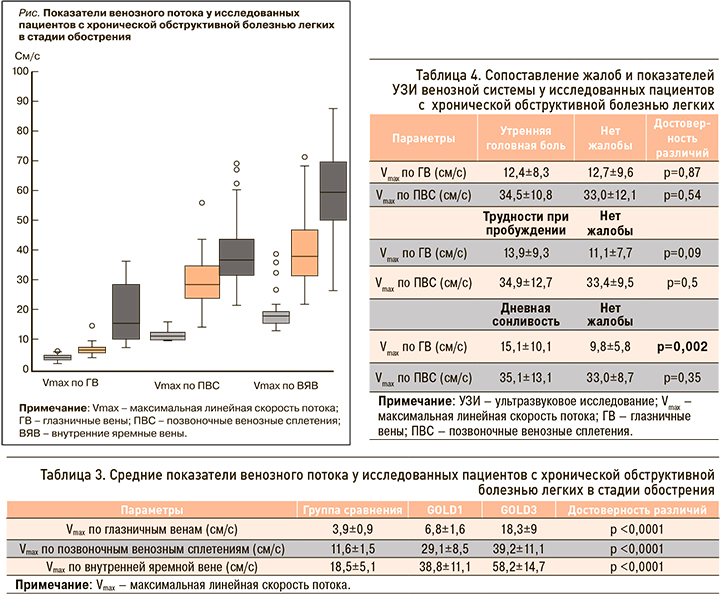
Все пациенты основной группы предъявляли жалобы на одышку разной степени выраженности и кашель с мокротой. Упомянутые ранее жалобы предположительно «венозного» происхождения встречались в основной группе со следующей частотой: характерная утренняя головная боль – 72; трудности при пробуждении – 50; дневная сонливость – 77 человек. Несколько чаще они выявлялись у более тяжелых пациентов (GOLD3) и больных с бронхитическим фенотипом заболевания (табл. 2). В группе сравнения указанные симптомы не встречались.
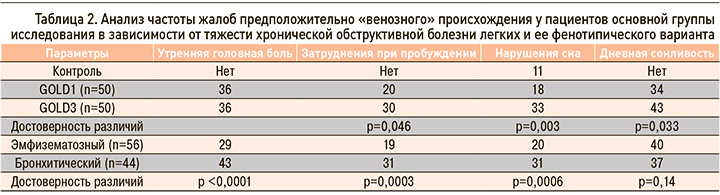
Наибольший интерес, по нашему мнению, представляют результаты анализа данных ультразвукового исследования (УЗИ) вен и их сопоставление с показателями функции внешнего дыхания и наличием клинической симптоматики. Практически у всех пациентов основной группы отмечалась инверсия потока по глазничным венам с одной или с обеих сторон, яремные вены приобретали округлую форму в поперечном сечении, не спадались полностью при компрессии датчиком. Максимальные скорости потока по глазничным венам и позвоночным сплетениям в среднем были выше как в основной группе по сравнению с контрольной, так и у пациентов с тяжелой степенью ХОБЛ (GOLD3) по сравнению с более легким течением болезни (GOLD1). Различия были высоко достоверными (табл. 3). Скорость кровотока в яремных венах в среднем также несколько возрастала, однако этот показатель был наиболее вариабельным. При подробном анализе данных можно отметить, что у больных GOLD 1 по сравнению с контрольной группой было наиболее выражено повышение венозного потока по позвоночным сплетениям, а по мере утяжеления процесса присоединялась существенная дисциркуляция по глазничным венам (рис.).
Следует также сказать, что у пациентов с эмфизематозным и бронхитическим фенотипическими вариантами каких-либо достоверных различий в параметрах венозного кровотока не выявлялось.
При сравнении показателей допплерографии с данными, полученными при исследовании функции внешнего дыхания, были обнаружены достоверные корреляции. Так, максимальный поток по глазничной вене показал сильную (коэффициент корреляции R=-0,68; p=0,4×10-7), а по позвоночным сплетениям умеренную (R=-0,42; p=0,002) достоверную отрицательную связь с ОФВ1. Сильные обратные корреляции наблюдались у параметров венозного потока с показателем, характеризующим наличие и выраженность воздушной ловушки, – отношением ОФВ1/ФЖЕЛ. Для глазничной вены коэффициент корреляции составил R=-0,6 (p=0,14×10-8), а для позвоночного сплетения – R=-0,54 (p=0,002).
Сопоставление жалоб и результатов УЗИ продемонстрировало отсутствие достоверных различий в показателях венозного потока у пациентов с жалобами на утреннюю распирающую головную боль (для глазничной вены p=0,87, для позвоночного сплетения p=0,54). Достоверно более высокие скорости потока по глазничной вене наблюдались у пациентов с жалобами на дневную сонливость. У пациентов с жалобами на трудности при пробуждении также отмечалась тенденция к более высоким значениям кровотока по глазничной вене, но эта тенденция была недостоверной (p=0,09; табл. 4).
ОБСУЖДЕНИЕ
Критерии нормы и патологии церебрального венозного оттока до сих пор однозначно не сформулированы, по крайней мере для относительно простых функциональных методов обследования, таких как экстракраниальная допплерография и дуплексное сканирование. Этому, безусловно, способствует целый ряд объективных причин, в первую очередь большая вариабельность строения венозного русла и значительная функциональная изменчивость венозного оттока. В изложенных результатах мы ограничились сравнением средних значений параметров венозного кровотока в группах, а также с показателями функции внешнего дыхания. Полученные высоко достоверные результаты позволяют заключить, что у пациентов с ХОБЛ, даже на ранних стадиях заболевания, имеются изменения оттока крови из полости черепа, а степень этих изменений связана с выраженностью дыхательных расстройств. С другой стороны, сопоставление ультразвуковых и клинических данных показало отсутствие четкой связи между жалобами, которые принято считать типичными, и изменениями венозного потока, за исключением дневной сонливости и отчасти синдрома «энцефалопатии пробуждения» (при котором выявленные различия не достигли предела статистической достоверности). Здесь нужно принять во внимание, что данные дуплексного сканирования были собраны в первой половине дня, а не в течение 30 мин после пробуждения, когда сохраняется клиническая симптоматика [13]. Кроме того, по современным представлениям энцефалопатия при ХОБЛ носит сложный, многокомпонентный характер [10, 11], и венозная дисциркуляция является лишь одним из звеньев патогенеза.
Исследование не касалось вопросов лечения нарушений венозного оттока, однако полученные результаты позволяют заключить, что меры, направленные на коррекцию этого состояния, рациональны при выявлении ретроградного венозного потока по глазничным венам более 10 см/с.
ЗАКЛЮЧЕНИЕ
Изменения церебрального венозного потока наблюдаются у пациентов с ХОБЛ уже на ранних стадиях заболевания, они имеют прямую связь с выраженностью «воздушной ловушки» и могут влиять на клиническую симптоматику. Исходя из полученных нами данных, всем пациентам с ХОБЛ в стадии обострения оправданно рекомендовать проведение дуплексного сканирования с оценкой венозного статуса, а тяжелым пациентам – с обязательной регистрацией потока по глазничным венам.