ВВЕДЕНИЕ
Происходящие в мире изменения демографической структуры характеризуются увеличением возраста населения и количества хронических неинфекционных заболеваний (ХНИЗ), тесно связанных с особенностями образа жизни. Наибольший вклад в смертность населения вносят сердечно-сосудистые заболевания (ССЗ), злокачественные новообразования, хронические обструктивные болезни легких и сахарный диабет (СД) [1]. Анализ динамики смертности от ССЗ в регионах Российской Федерации в 2019–2021 гг. показал увеличение среднерегионального стандартизованного коэффициента смертности с 301,02 в 2019 г. до 336,15 в 2020 г. (p=0,025) и до 338,73 – в 2021 г. (p=0,9 между 2021 и 2020 г., p=0,015 между 2021 и 2019 г.) [2]. В период 2015–2019 гг. был выявлен ежегодный прирост уровней заболеваемости болезнями системы кровообращения (БСК) в трудоспособном возрасте по следующим показателям: первичная и общая заболеваемость БСК в целом и цереброваскулярными заболеваниями, общая заболеваемость ишемической болезнью сердца (ИБС) [3]. В странах европейского региона на долю смертности от ССЗ приходится 31% всех случаев смерти мужчин и 26% – женщин в возрасте до 65 лет [4].
На сегодняшний день отмечается неравномерность снижения бремени смертности в разных возрастных группах: положительная тенденция наблюдается в группе лиц пожилого возраста, тогда как в группе лиц молодого возраста такая динамика отсутствует [5]. Преждевременное развитие ССЗ свидетельствует о том, что молодые люди проживают свои продуктивные годы с плохим здоровьем и низким качеством жизни, что приводит к ранней инвалидизации. В связи с этим изучение факторов, ассоциированных с развитием ССЗ и их осложнений у лиц трудоспособного возраста, видится актуальной проблемой.
Факторы, ассоциированные со смертностью в трудоспособном возрасте, неоднородны и включают как традиционные (ожирение, курение, гиперхолестеринемия и др.), так и характерные для этой возрастной категории, к которым относятся недостаточная осведомленность о ССЗ и кардиоваскулярных факторах риска (ФР) [6]. В связи с этим вероятность развития CCЗ у некоторых лиц молодого и среднего возраста существенно повышена за счет имеющихся ФР. Кроме того, нередко недооцениваются биологические и психосоциальные различия в риске развития ССЗ. Согласно исследованию INTERHEART, охватившему 52 страны мира с участием более 30 000 пациентов, депрессия и тревога вносят существенный вклад в развитие сердечно-сосудистых событий наряду с такими общепринятыми факторами, как курение, гиперхолестеринемия, артериальная гипертензия (АГ), ожирение, малоподвижный образ жизни и злоупотребление алкоголем [7]. Широко используемая шкала SCORE для стратификации кардиоваскулярного риска опирается на «классические» ФР и не лишена такого существенного недостатка, как недооценка истинной вероятности развития сердечно-сосудистых осложнений. В частности, в шкале SCORE не учитывается наличие измененного психоэмоционального статуса пациента. Особенно это актуально для пациентов с низким и умеренным кардиоваскулярным риском, определяемым по критериям этой системы. Сохранение низкого сердечно-сосудистого риска у лиц с минимальной вероятностью развития заболевания, особенно в молодом и среднем возрасте, жизненно необходимо для предупреждения развития ранней мультиморбидности.
Понимание того, какие именно ФР и их сочетания связаны с функциональным состоянием организма, мультиморбидностью и сердечно-сосудистым риском в молодом возрасте, является важным шагом на пути к продлению жизни и поддержания независимой жизни на должном уровне в более старшем возрасте. К настоящему времени существует достаточно доказательств, что мультиморбидность чаще встречается и раньше формируется у лиц с более низким социально-экономическим статусом, а ее встречаемость у лиц молодого и среднего возраста требует более детального изучения факторов, с ней ассоциированных [8, 9].
Тревожные и депрессивные состояния рассматривают в качестве модификаторов риска развития ХНИЗ, а их роль в прогрессировании ССЗ была подтверждена многими исследователями [1, 10, 11].
Исследования, направленные на изучение факторов сердечно-сосудистого риска у лиц молодого и среднего возраста, немногочисленны и обычно ограничиваются оценкой традиционных ФР. Количество работ, посвященных комплексному анализу состояния здоровья лиц молодого и среднего возраста с учетом психологических ФР (тревожности и депрессии) и мультиморбидности, также ограниченно. Чтобы восполнить этот пробел, целью нашего исследования стало изучение встречаемости субклинической тревожности и депрессии у лиц трудоспособного возраста, оценка их связи с факторами кардиоваскулярного риска и мультиморбидностью.
МАТЕРИАЛ И МЕТОДЫ
Одномоментное сравнительное исследование проводилось в рамках ежегодного профилактического медицинского осмотра городских жителей трудоспособного возраста.
Критерии включения: лица мужского и женского пола, возраст 25–59 лет, добровольное участие в исследовании.
Критерии невключения: тяжелое течение заболевания в настоящее время или в анамнезе, психическое или ментальное расстройство/заболевание в анамнезе, которые могли помешать проведению исследования, злоупотребление алкоголем или наркотиками и/или алкогольная или наркотическая зависимость, участие в другом клиническом исследовании во время данного исследования или в течение последних 30 дней, невозможность подписать информированное согласие для участия в исследовании в силу отсутствия у пациента приверженности к процедурам исследования.
Всем пациентам выполнялся общепринятый физикальный осмотр. Сведения о ФР, анамнезе, сопутствующей патологии были получены из данных опроса и предоставленной медицинской документации. Расчет индекса массы тела (ИМТ) осуществлялся по формуле Кеттле. Значение ИМТ менее 25 кг/м² служило показателем нормальной массы тела, 30 кг/м² и более – критерием ожирения, промежуточные значения рассматривались как избыточная масса тела [13]. Гиперхолестеринемия определялась при уровне общего холестерина >4,9 ммоль/л [14].
Сердечно-сосудистый риск оценивался у относительно здоровых лиц в возрасте 40 лет и старше по шкале Systematic Coronary Risk Estimation (SCORE), в возрасте до 40 лет – по шкале относительного риска. К регулярно курящим относили лиц, выкуривающих хотя бы 1 сигарету в день или бросивших курить менее 1 года назад [13].
Артериальная гипертензия (АГ) верифицировалась при уровне офисного измерения артериального давления (АД) ≥140/90 мм рт.ст. и при домашнем измерении АД (≥135/95 мм рт.ст.) не менее чем при трехкратном измерении на двух руках. В качестве критериев целевого АД рассматривались значения, соответствующие актуальным российским клиническим рекомендациям (2020) [15].
Верификация ИБС осуществлялась при наличии типичных клинических симптомов, указаний на перенесенный инфаркт миокарда в анамнезе [16]. Диагноз сахарного диабета подтверждался на основании клинико-анамнестических данных и результатов лабораторного обследования, заключения эндокринолога в соответствии с общепринятыми рекомендациями [17].
Сочетание ≥2 любых ХНИЗ с высокой медико-социальной значимостью рассматривалось как мультиморбидность [18]. Лечение АГ, ИБС, сахарного диабета, гиперхолестеринемии при их наличии проводилось согласно современным клиническим рекомендациям и не менялось в течение 1 мес до включения в исследование.
Для оценки уровня тревожности и депрессии проводилось анкетирование по опроснику госпитальной шкалы тревоги и депрессии (Hospital Anxiety and Depression Scale, HADS). При интерпретации результатов учитывался общий балл по каждой из подшкал: значения в 0–7 баллов указывали на отсутствие тревоги и депрессии, 8–10 баллов – на субклиническую тревогу/депрессию, более 10 баллов – на клинически выраженную тревогу/депрессию [19].
Протокол исследования (от 22.10.2018 №178) был принят к сведению этическим комитетом ФГАОУ ВО «Российский национальный исследовательский медицинский университет им. Н.И. Пирогова» Минздрава России. Все пациенты подписали согласие на участие в исследовании. Исследование проводилось в отделении медицинской профилактики – ГБУЗ «Городская клиническая больница № 13 Департамента здравоохранения г. Москвы». Лабораторное обследование проводилось на базе клинико-диагностической лаборатории этого учреждения.
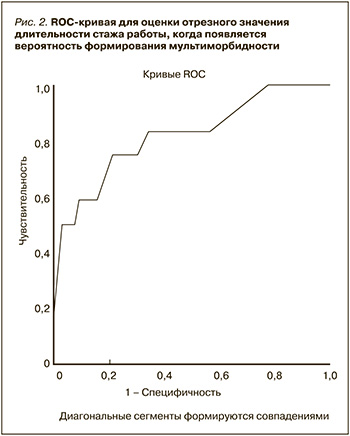
Для статистической и графической обработки данных использовались программы Microsoft Excel и SPSS Statistics version 20.0 (IBM, USA). При обработке результатов для стандартизации показателей применялась возрастная структура пациентов в диапазоне 25–59 лет. Данные представлены в виде медианы и интерквартильного размаха для непрерывных переменных с распределением, отличным от нормального. Для анализа различий между количественными признаками применялся ранговый U-критерий Манна–Уитни, между качественными – таблицы сопряженности 2×2 по критерию χ2 Пирсона с поправкой Йетса и точному критерию Фишера. Взаимосвязь между непрерывными показателями оценивалась с помощью коэффициента ранговой корреляции Спирмена. Для выявления факторов, оказывающих значимое влияние на субклиническую тревогу, депрессию и мультиморбидность, рассчитывалось отношение шансов (ОШ) с 95% доверительным интервалом (ДИ). Порог формирования мультиморбидности в зависимости от длительности стажа определялся с помощью ROC (receiver-operating characteristic) анализа с построением характеристических кривых и расчетом площади под кривой. Различия считались статистически значимыми при двустороннем p <0,05.
РЕЗУЛЬТАТЫ
В исследовании приняли участие 94 пациента: 36 (38,2%) мужчин и 58 (61,8%) женщин. Медиана возраста составила 30 (26; 40) лет: возраст мужчин – 30 (29; 36) лет, женщин – 34 (25; 40) лет. В возрасте 25–44 лет было 84 (89,3%), 45–59 лет – 10 (10,7%) пациентов. Клиническая характеристика исследованных пациентов представлена в таблице 1.

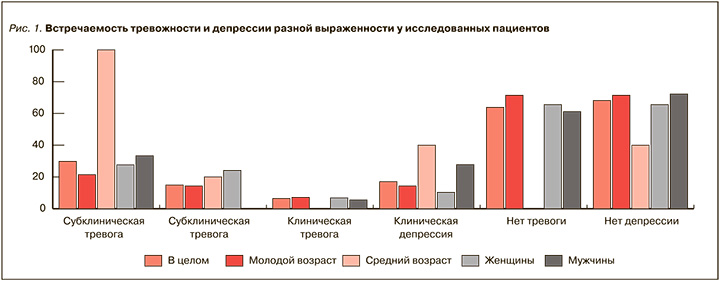
Расстройства тревожного и депрессивного спектра имелись у 34 из 94 (36,2%) пациентов (рис. 1).
Данные корреляционного анализа между изучаемыми показателями и субклинической тревогой/депрессией, мультиморбидностью представлены в таблице 2, логистического регрессионного анализа – в таблице 3.


Отрезное значение длительности стажа работы, когда появляется вероятность формирования мультиморбидности, в изучаемой когорте лиц молодого и среднего возраста составило 16,5 лет при чувствительности 75% и специфичности 77% (значение площади под ROC-кривой 0,822±0,072 при 95% ДИ 0,68–0,96; р <0,001; рис. 2).
ОБСУЖДЕНИЕ
В вышеприведенном исследовании проанализирована группа пациентов (медиана возраста 30 лет), проходивших профилактический медицинский осмотр у врача общей практики. Большинство из них было лицами молодого возраста (89,3 %), женского пола (61,8 %), имело семью (65,9%), вело подвижный образ жизни (80,9 %) и соответствовало градации низкого сердечно-сосудистого риска (80,8 %). У каждого третьего пациента (34 %) был отягощенный семейный анамнез по ССЗ. Избыточная масса тела имелась у 37,5 %, нарушение ночного сна – у 21,2 %, курили 27,6 % человек, стаж курения соответствовал медиане 5 лет. Практически у каждого десятого участника были выявлены гиперхолестеринемия (11,7 %), ожирение (12,7 %), ИБС (11,7 %) и сахарный диабет (10,6 %). Полученные нами результаты согласуются с существующими данными, согласно которым в возрасте 25–64 лет 25,7 % человек курят, 38,8 %ведут малоподвижный образ жизни, 29,7 % имеют ожирение [20]. Результаты исследования STEPS c участием пациентов в возрасте 18 лет и старше свидетельствуют о наличии сахарного диабета у 8,4 %, гиперхолестеринемии – у 15 %, что также совпадет с нашими результатами [21].
Принципы профилактики сердечно-сосудистых заболеваний одинаковы для людей разного возраста, а различия в тенденциях формирования ФР и развития кардиоваскулярных патологий требуют более детального изучения, поскольку существует мнение, что люди более молодого возраста менее восприимчивы к стратегиям профилактики. Тревожно-депрессивные расстройства могут усугублять этот процесс, поскольку оказывают негативное воздействие на качество жизни, функционирование человека в обществе и на течение заболеваний. Показано, что пациенты без субклинической тревоги и депрессии имели риск развития сердечно-сосудистых осложнений примерно в 5 раз ниже (ОШ 4,9; 95% ДИ: 1,4–17,9), чем лица с этими нарушениями. По данным 10-летнего наблюдения в случае наличия у пациентов нарушения липидного обмена, повышения систолического АД более 130 мм рт.ст. и депрессии и/или тревоги, включая их субклинические формы, вероятность развития сердечно-сосудистых осложнений и смерти возрастала более чем в 7 раз (ОШ 7,28; 95% ДИ: 2,48–21,36) [10].
Оценивая полученные результаты, мы отметили, что 34 (36,2%) пациента имели расстройства тревожного и депрессивного спектра по шкале HADS. У каждого третьего пациента (29,8%) была выявлена субклиническая тревога, у 14,9% – субклиническая депрессия. Субклиническая тревога определялась у 21,4% лиц молодого и у всех (100%) пациентов среднего возраста, с одинаковой частотой у женщин (27,4%) и мужчин (33,3%). Субклиническая депрессия была установлена у 14,3% лиц молодого и у 20% – среднего возраста, при этом она встречалась у каждой четвертой женщины и отсутствовала у мужчин.
Согласно результатам исследования ЭССЕ-РФ, тревожные расстройства достаточно широко распространены среди населения разного возраста и достигают 18,1% (10,9% у мужчин и 22,7% у женщин), а симптомы клинической тревожности возможны у 30–40% лиц, обращающихся за помощью к врачу общей практики [22, 23].
Именно пациенты с субклинической тревогой и депрессией в дальнейшем анализировались нами, поскольку клинические формы этих заболеваний рассматриваются в рамках диагноза и требуют дальнейшего дообследования у специалиста. Выбор шкалы HADS был обусловлен ее показанием для применения в качестве инструмента скрининга тревожно-депрессивного статуса в общемедицинской практике терапевта и кардиолога, удобством для врачей первичного звена здравоохранения из-за небольшого периода времени, необходимого для ее заполнения, и простоты вопросов и интерпретации показателей [19, 24].
Обследованные нами пациенты с тревожно-депрессивными расстройствами имели более высокий уровень систолического АД (р=0,004), среди них чаще встречались лица с гиперхолестеринемией (р=0,001), отягощенным семейным анамнезом по сахарному диабету (р=0,045), малоподвижным образом жизни (р=0,030), с умеренным (р=0,045) и очень высоким сердечно-сосудистым риском (р=0,001), ИБС (р=0,001), ожирением (р=0,004) и мультиморбидностью (р=0,001), чем среди лиц без этих расстройств.
Выполненный нами анализ показал тесную корреляцию имевшейся субклинической тревоги и депрессии с умеренным сердечно-сосудистым риском. Кроме того, субклиническая тревога тесно коррелировала с возрастом 45–59 лет и такими традиционными ФР, как гиперхолестеринемия, ожирение, систолическое АД, малоподвижный образ жизни, отягощенный семейный анамнез по ССЗ, ИБС и сахарный диабет (СД), а субклиническая депрессия – с женским полом и средним образованием. При логистическом регрессионном анализе была подтверждена тесная ассоциация субклинического тревожно-депрессивного состояния с умеренным сердечно-сосудистым риском (ОШ 29,3). Сахарный диабет (ОШ 8,7), ССЗ у родителей (ОШ 4,2), ИБС (ОШ 36,1), сахарный диабет в анамнезе (ОШ 30,8) и ожирение (ОШ 6,2) тесно ассоциировались с субклинической тревогой у лиц молодого и среднего возраста.
Полученные результаты вполне закономерны, поскольку в последние годы накоплены данные, подтверждающие факт связи тревожно-депрессивного состояния с рядом факторов риска ССЗ [25– 28]. С другой стороны, субклинические тревога и депрессия, особенно выявленные на раннем этапе их формирования, за счет тесной связи с ФР, в некоторых ситуациях могут позволить обнаружить их предвестники, в частности бессимптомную дислипидемию, и предотвратить развитие фатальных кардиоваскулярных событий, что было показано в исследовании авторов из Южной Кореи с участием 72 235 человек [29]. В свою очередь, своевременно не диагностируемые тревога и депрессия, особенно у женщин, могут препятствовать проведению рациональной фармакотерапии и снижать приверженность пациентов рекомендациям врача [30, 31].
Бремя мультиморбидности требует повышенного внимания к состоянию здоровья лиц молодого возраста, поскольку именно на этом этапе закладывается ее основа в виде формирования ФР ХНИЗ. С этой точки зрения крайне актуальным представляется выделение дополнительных факторов, которые могут повлиять на формирование мультиморбидности на данном этапе жизни. Наше исследование выявило мультиморбидность у 9,5% обследованных и ее тесную корреляцию (р <0,001) и ассоциацию с субклинической тревогой (ОШ 17,8), которую возможно рассматривать в качестве нетрадиционного фактора (модификатора) развития мультиморбидности. Профессия и стаж работы являются неотъемлемой частью жизни любого человека. Учитывая колоссальную нагрузку, прежде всего психоэмоциональную, которая постоянно сопровождает практически любого работающего человека, предположить, что не только специальность, но и длительность профессионального стажа служат факторами риска мультиморбидности. Это и было показано в ходе проведенного нами исследования.
Важнейший фактор профилактики прогрессирования заболеваний – приверженность пациента рекомендациям врача и его осведомленность о показателях своего здоровья. Согласно нашим данным, об уровне АД, холестерина и глюкозы были осведомлены 80,8 % обследованных, высокая приверженность лечению была установлена у 61,7 % человек, при этом регулярно досаливали пищу 36,1 %, употребляли овощи и фрукты 44,6% лиц. Обращает на себя внимание тесная ассоциация субклинической тревоги с ключевыми моментами, нарушающими здоровый образ жизни, а именно с гиподинамией (ОШ 4,0) и недостатком овощей/фруктов в рационе питания (ОШ 2,7) как маркером нездорового питания. Образ жизни, пищевые привычки и характер питания, которые закладываются в раннем детстве, изменяются со времени под влиянием разных факторов, включая и психосоциальные. В связи с этим нельзя не согласиться с существующим мнением о смене парадигмы в отношении взгляда на проблему здоровья, а именно о необходимости формирования сердечно-сосудистого здоровья на каждом этапе жизни человека: в детстве, юности, молодом среднем и пожилом возрасте [32].
Наличие тревожно-депрессивного состояния может усилить склонность к нерациональному питанию и гиподинамии, что требует их своевременного выявления и коррекции на субклиническом этапе и в более молодом возрасте. Ряд крупных исследований свидетельствует о превалировании в рационе питания лиц молодого возраста продуктов с высокой энергетической ценностью и недостатке овощей, фруктов на фоне чрезмерного употребления насыщенных жиров по сравнению с лицами более старшего возраста [33]. Rosinger A. et al. показали, что мужчины в возрасте 20–39 лет потребляли из сахаросодержащих напитков в среднем 249 ккал, женщины – 160 ккал, в возрасте 40–59 лет – 172 и 111 ккал соответственно; это соответствовало 6,9 и 6,1% от общей суточной калорийности обследованных в возрасте [34].
Точный механизм, лежащий в основе ассоциации тревожно-депрессивных расстройств с развитием и прогрессированием ССЗ, не установлен, однако эту связь возможно объяснить нездоровым образом жизни пациентов, снижением приверженности рекомендациям врача, влиянием социальных и экономических воздействий, кардиометаболическими эффектами некоторых видов фармакотерапии, а также недостаточной осведомленностью врача в области психоэмоционального состояния здоровья пациентов и несвоевременным выявлением традиционных факторов риска ХНИЗ [35].
В настоящее время рекомендована оценка психосоциальных факторов риска с помощью клинического опроса или стандартизованных опросников для выявления возможных препятствий к изменению образа жизни (класс рекомендаций IIa, уровень доказательности В) [23, 35].
Нетрадиционные ФР (модификаторы) целесообразно учитывать, если они улучшают прогностические показатели сердечно-сосудистого риска, влияют на общественное здравоохранение, доступны к применению в рутинной практике, обладают информацией относительно того, как возрастает риск при неблагоприятном результате и как возможно его снизить. Этим критериям соответствуют субклиническая тревога и депрессия, которые могут вносить вклад в оценку состояния здоровья лиц молодого и среднего возраста с умеренным сердечно-сосудистым риском, когда необходима дополнительная информация для детализации уровня риска не только в сторону его увеличения, но и снижения [23].
Ограничения исследования: малая выборка пациентов, превалирование лиц молодого возраста, отсутствие метода слепой рандомизации, что необходимо учитывать при интерпретации результатов.
ЗАКЛЮЧЕНИЕ
Расстройства тревожного и депрессивного спектра были обнаружены у 36,2% лиц молодого и среднего возраста. У 14,9% обследованных была выявлена субклиническая депрессия, у каждого третьего пациента (29,8%) – субклиническая тревога, имевшаяся у всех лиц среднего возраста. Субклиническая депрессия с одинаковой частотой встречалась у лиц молодого и среднего возраста, у каждой четвертой женщины и отсутствовала у мужчин. Тесная ассоциация субклинической тревоги и депрессии с умеренным сердечно-сосудистым риском, а также ряда факторов риска ССЗ, ИБС и сахарного диабета с субклинической тревогой позволяет рассматривать последнюю как дополнительный модификатор ранней сердечно-сосудистой мультиморбидности. Бремя мультиморбидности требует повышенного внимания к состоянию здоровья людей, начиная с молодого возраста, тем более, как показало наше исследование, мультиморбидность ассоциирована не только с субклинической тревогой, но и средним возрастом, а также длительностью профессионального стажа. Полученные результаты свидетельствуют о целесообразности скрининга субклинической тревоги и депрессии у уязвимых (с множественными факторами риска, семейным анамнезом ССЗ, умеренным кардиоваскулярным риском) лиц молодого и среднего возраста, поскольку представляют собой доступный и недорогой метод получения дополнительной информации, который может позволить инициировать комплексную оценку риска.
Открытым остается вопрос разработки методики учета психосоциальных ФР для улучшения модели прогнозирования сердечно-сосудистого риска и накопления достаточных доказательств для потенциальных модификаторов кардиоваскулярного риска как составляющих улучшения предсказания прогноза, наряду с классическими ФР.