Обструктивные заболевания легких (ОЗЛ) – хроническая обструктивная болезнь легких (ХОБЛ) и бронхиальная астма (БА) – относятся к патологическим состояниям со стремительно растущей распространенностью и рассматриваются как проблемы мирового масштаба.
ХОБЛ является одной из ведущих причин заболеваемости и смертности в мире, что ведет к значительному экономическому и социальному ущербу. По оценкам исследования Глобального бремени болезней, в 2016 г. зарегистрирован 251 млн случаев ХОБЛ во всем мире. В 2015 г. этим заболеванием было обусловлено 3,17 млн смертей, что составило 5% от всех летальных исходов. Если в 1990 г., по данным Всемирной организации здравоохранения (ВОЗ), ХОБЛ занимала 12-е место среди причин смерти в мире, то в настоящее время вышла на 3-е место [1, 2, 3, 4].
Серьезной глобальной проблемой здравоохранения остается БА, которая развивается у 1–18% населения в разных странах [5]. В настоящее время в мире ею страдают около 235 млн человек [6]. БА затрагивает все возрастные группы, создавая социальные, экономические, медицинские и личностные проблемы в обществе. В 2015 г. около 383 000 случаев смерти было вызвано этим заболеванием [7].
На современном этапе чрезвычайно актуальна проблема мультиморбидности, т.е. сочетания у одного пациента нескольких хронических заболеваний, патогенетически взаимосвязанных между собой. К числу заболеваний, которые нередко отягощают коморбидный фон у пациентов с бронхообструктивными заболеваниями легких, относится сахарный диабет 2 типа (СД2).
СД2 – самое распространенное заболевание эндокринной системы, которое в настоящий момент приняло характер эпидемии в большинстве развивающихся и развитых стран мира [8]. Распространенность диабета среди людей старше 18 лет в мире за последние 10 лет увеличилась более чем в 2 раза и к концу 2017 г. превысила отметку в 425 млн человек. По данным федерального регистра СД2, в России в 2018 г. на диспансерном учете состояло 4 584 575 человек (3,1% населения) [9]. При этом результаты российского эпидемиологического исследования NATION свидетельствуют, что СД2 диагностируется лишь в 54% случаев. Таким образом, реальная численность пациентов с СД2 в нашей стране составляет не менее 9 млн человек, т.е. около 6% населения [10].
Большинство исследований, посвященных изучению нарушений углеводного обмена у больных с ОЗЛ, рассматривает влияние уже диагностированного СД2 или нарушения толерантности к углеводам (т.е. хронической гипергликемии) на течение и прогноз заболеваний легких. Частота сочетания ХОБЛ и СД2 составляет от 2 до 35,8% [11, 12, 13, 14]; существует мнение, что наличие СД2 при ХОБЛ оказывает более существенное влияние на смертность и количество госпитализаций, чем увеличение тяжести и снижение скорости воздушного потока [15]. По данным разных авторов, БА сочетается с СД2 у 9–40% пациентов. При этом наличие коморбидного фона, в том числе СД2, определяет снижение уровня контроля БА, увеличивает частоту обострений и соответственно число госпитализаций за год [16, 17, 18].
Между тем известно, что самой распространенной формой нарушений углеводного обмена при ОЗЛ является гипергликемия, которая выявляется при госпитализации пациентов по поводу обострения болезни. Такая гипергликемия имеет разные названия: госпитальная, стационарная, острая, стрессовая, транзиторная. При этом до настоящего времени нет единого подхода к оценке механизмов формирования и верификации таких нарушений углеводного обмена. Не определены их исходы, а также влияние на течение и прогноз ОЗЛ, а также развитие СД2.
ГОСПИТАЛЬНАЯ ГИПЕРГЛИКЕМИЯ: ОПРЕДЕЛЕНИЕ ПОНЯТИЯ, ФАКТОРЫ ПАТОГЕНЕЗА
Госпитальная (стационарная, острая, стрессовая, транзиторная) гипергликемия определяется как любое значение глюкозы крови, превышающее 7,8 ммоль/л (140 мг/дл) у лиц без СД2 в анамнезе [19]. Она часто сопровождает различные острые заболевания и критические состояния (инфаркт миокарда, инсульт и т.д.).
Обсервационные исследования показывают, что гипергликемия выявляется у 32–38% из всех госпитализированных пациентов, у 41% больных с острым коронарным синдромом (ОКС), у 44% пациентов с сердечной недостаточностью и у 80% пациентов, перенесших кардиохирургические операции. В этих исследованиях около 1/3 больных отделений терапевтического профиля и 80% пациентов отделений реанимации и интенсивной терапии с выявленной гипергликемией не имели в анамнезе диабет при поступлении [20].
Госпитальная гипергликемия – частая находка при обострении бронхообструктивных заболеваний, которая встречается у 91% пациентов с сопутствующим СД2 и, что важно подчеркнуть, у 63% пациентов, не имевших ранее нарушений углеводного обмена [21].
В патогенезе госпитальной гипергликемии при обострении ОЗЛ рассматриваются следующие факторы:
- Нейроэндокринный и воспалительный стрессовый ответ. При острых состояниях продукция глюкозы повышается в связи со стрессовой реакцией организма на критическую ситуацию и/или вследствие ятрогенных воздействий. При этом активируется выработка гормонов контринсулярной системы – глюкокортикоидов и катехоламинов. Эти гормоны, а также провоспалительные цитокины (фактор некроза опухоли альфа, интерлейкины-1 и - 6 и др.) влияют на различные звенья метаболизма: активируют липолиз, повышают содержание свободных жирных кислот, способствуют развитию инсулинорезистентности, подавляют секрецию инсулина, стимулируют гликогенолиз и глюконеогенез в печени, вызывая гипергликемию [22].
- Гипоксия. Исследования, проводимые с начала 2000-х гг., свидетельствуют, что острая гипоксия сама вызывает нарушение толерантности к глюкозе, повышает уровень эпинефрина в плазме, увеличивает частоту сердечных сокращений и тревожность. Интермиттирующая гипоксия ведет к инсулинорезистентности и нарушению инсулинонезависимой утилизации глюкозы [23]. Кроме того, по данным M. Pallayova, гипоксия ассоциирована с повреждением β-клеток поджелудочной железы [24].
- Ацидоз. Обострение ХОБЛ может осложниться гиперкапнической дыхательной недостаточностью и респираторным ацидозом. Более ранние исследования показали, что респираторный ацидоз вызывает нарушение толерантности к глюкозе, индуцируя печеночную и периферическую инсулинорезистентность. Кроме того, эксперименты на животных демонстрируют, что метаболический ацидоз может вызывать нарушение секреции инсулина [23].
- Медикаменты:
- глюкокортикоиды. Препараты этой группы служат основной причиной гипергликемии, индуцированной лекарственными средствами. Они не только усугубляют гипергликемию у больных с установленным диагнозом СД2, но и вызывают заболевание у пациентов, не имевших гипергликемии до начала кортикостероидной терапии. Гипергликемия развивается у 64% госпитализированных пациентов, получающих высокие дозы системных глюкокортикоидов (≥40 мг преднизолона в день), а уровень глюкозы может увеличиваться на 68% по сравнению с исходным [25, 26]. Было показано, что в генезе СД2 и других метаболических сдвигов, возникающих на фоне длительной терапии ингаляционными глюкокортикостероидами (ИГКС) у пациентов с БА, ведущая патогенетическая роль принадлежит формирующейся инсулинорезистентности и гиперинсулинемии [26];
- β-агонисты и другие катехоламины. Экспериментальные и клинические данные свидетельствуют, что β2-агонисты повышают уровень глюкозы, влияя на секрецию инсулина и глюкагона поджелудочной железой, метаболизм печени и потребление глюкозы тканями [27];
- антибиотики. Противомикробные средства могут нарушать метаболизм глюкозы и вызывать как гипергликемию, так и гипогликемию. В наибольшей степени это относится к препаратам класса фторхинолонов, которые повышают риск развития серьезных побочных эффектов у пациентов, страдающих СД [28];
- теофиллин, аминофиллин. Существуют данные о влиянии теофиллина на метаболизм глюкозы.
В экспериментах на животных использование аминофиллина приводило к гипергликемии, возможно, за счет индукции инсулинорезистентности [23, 27].
Таким образом, у госпитализированых по поводу обострения ОЗЛ пациентов вследствие патогенетических и медикаментозных влияний формируются гипергликемия и инсулинорезистентность, что неизбежно приводит к развитию эндогенной гиперинсулинемии, которая, с одной стороны, служит компенсаторной реакцией, а с другой – патологической. Помимо прямого негативного действия гипергликемии на организм, которое мы подробно рассмотрим ниже, сама по себе гипер-инсулинемия может вызывать задержку натрия почками, дисфункцию эндотелия и изменения в свертывающей системе крови (гиперфибриногенемию и повышение активности ингибитора тканевого активатора плазминогена I типа, уменьшение фибринолиза, повышение агрегации тромбоцитов, увеличение синтеза тромбоксанов, снижение активности антитромбина III) [29].
ВЛИЯНИЕ ГОСПИТАЛЬНОЙ ГИПЕРГЛИКЕМИИ НА ИСХОДЫ ОБОСТРЕНИЙ БРОНХООБСТРУКТИВНЫХ ЗАБОЛЕВАНИЙ
Данные литературы о влиянии госпитальной гипергликемии на исходы обострений бронхообструктвивных заболеваний весьма противоречивы. Многие авторы отмечают связь госпитальной гипергликемии, ассоциированной с обострением ОЗЛ, с повышением риска неблагоприятных исходов: длительности пребывания в стационаре, острой дыхательной недостаточности, смертности [30, 31, 32, 33].
Одним из наиболее важных факторов, определяющих ухудшение прогноза при обострении ОЗЛ, выступает повышение риска легочной инфекции при гипергликемии. Установлено, что в поверхностной жидкости дыхательных путей концентрация глюкозы в 12 раз ниже, чем в плазме [33]. Низкая концентрация глюкозы в респираторном тракте вносит важный вклад в противоинфекционную защиту легких, поскольку при этом снижается доступность питательных веществ и ограничивается бактериальный рост. Присутствие глюкозы в респираторном тракте, напротив, предрасполагает к инфекционным осложнениям [34, 35].
С другой стороны, J.P. Garnett с соавт. показали, что инкубирование клеток бронхиального эпителия с провоспалительными медиаторами (фактор некроза опухоли альфа, липополисахарид) ведет к увеличению концентрации глюкозы в поверхностной жидкости дыхательных путей. При этом повышается не только трансэпителиальная проницаемость, но и апикальное поглощение глюкозы, опосредованное транспортерами GLUT-2 и GLUT-10.
Однако утилизация глюкозы возрастает недостаточно, чтобы ограничить ее накопление в поверхностной жидкости дыхательных путей. Результаты этих экспериментов объясняют механизм увеличения концентрации глюкозы в бронхиальном дереве при воспалении респираторного тракта [36].
Кроме того, известно, что гипергликемия способна нарушать клеточные механизмы защиты от инфекции. Высокие уровни глюкозы индуцируют оксидативный стресс и влияют на иммунную систему, уменьшая дегрануляцию нейтрофилов во время воспаления, вызывая дефекты адгезии и ухудшая фагоцитоз, хемотаксис, бактериальный киллинг. Гипергликемия может также снижать секрецию протеаз нейтрофилами, что приводит к снижению антимикробной активности. Кратковременная гипергликемия влияет на все главные компоненты врожденного иммунитета и нарушает способность хозяина контролировать инфекцию, способствуя снижению количества лимфоцитов и перераспределению пулов лимфоцитов. Эти аномалии обратимы при снижении уровня глюкозы [23]. Нарушение гомеостаза глюкозы способствует усилению колонизации дыхательных путей микрофлорой [34, 35, 37, 38], что вместе со снижением защитных механизмов хозяина повышает риск инфекционных осложнений и неблагоприятных исходов ХОБЛ.
В таблице представлены результаты современных ретроспективных когортных исследований, посвященных оценке влияния гипергликемии на исходы обострений бронхообструктивных заболеваний. Большинство исследователей показало, что гипергликемия повышает риск неблагоприятных исходов – длительной госпитализации и смерти [21, 31, 32, 33, 39]. В большей степени это характерно для пациентов с уже диагностированным СД2, в то время как преходящая гипергликемия не влияет на отдаленный прогноз ХОБЛ [40].
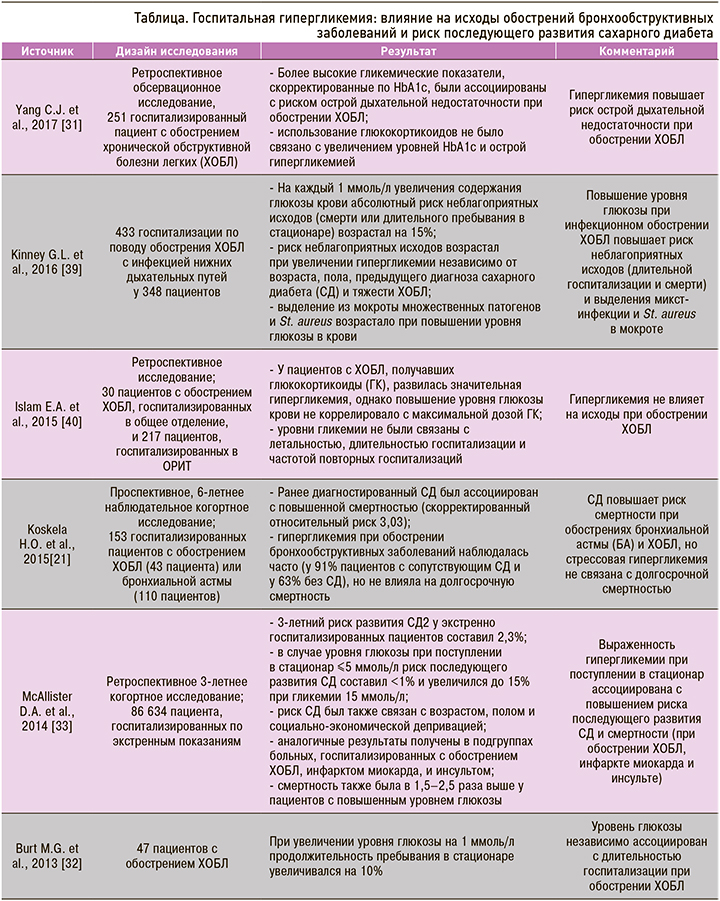
ВЛИЯНИЕ ГОСПИТАЛЬНОЙ ГИПЕРГЛИКЕМИИ НА РИСК РАЗВИТИЯ САХАРНОГО ДИАБЕТА 2 ТИПА
Оценке риска развития СД2 у больных с госпитальной гипергликемией в анамнезе посвящены единичные исследования. Из таблицы 1 видно, что большинство из представленных работ рассматривало прогностическую роль гипергликемии лишь в аспекте бронхолегочной патологии, не учитывая при этом ее значение как фактора риска развития СД2.
Вместе с тем D.A. McAllister et al. установили, что 3-летний риск развития СД2 у экстренно госпитализированных пациентов составил 2,3%. У больных, поступающих в стационар с уровнем глюкозы ≤5 ммоль/л, риск последующего развития СД2 был <1%, а при гликемии 15 ммоль/л и выше увеличивался до 15%. Отмечено также, что риск возникновения диабета ассоциируется с возрастом, полом и социально-экономической депривацией пациентов. В подгруппах больных, госпитализированных с инфарктом миокарда, ХОБЛ и инсультом, были получены сходные результаты [33].
В современной литературе существует и альтернативная точка зрения на клиническое и патофизиологическое значение госпитальной гипергликемии. В обзоре литературы, опубликованном P.E. Marik & R. Bellomo, гипергликемия легкой и умеренной степени рассматривается как защитная реакция при стрессе и критическом состоянии. Авторы высказывают гипотезу о положительном эффекте острой гипергликемии и отрицательном эффекте хронической гипергликемии [41].
Также Y. Kasirye еt al. исследовали 209 госпитализированных больных с обострением ХОБЛ для изучения факторов, ассоциированных с осложнениями, длительностью госпитализации, повторными госпитализациями в течение 30 дней после выписки и 90-дневной смертностью от любых причин. Авторами не было обнаружено корреляций между высоким уровнем глюкозы и нежелательными исходами заболевания, тогда как снижение глюкозы крови <4,9 ммоль/л (90 мг/дл) ассоциировалось с увеличением госпитальных осложнений и длительности пребывания в стационаре. В этом исследовании для выявления гипергликемии использовали среднесуточный уровень глюкозы крови, так как у больных с обострением ХОБЛ, получающих глюкокортикоиды, имеется тенденция к повышению содержания глюкозы крови в послеобеденное и вечернее время, поэтому оценка суточного профиля глюкозы крови является более информативной [42].
ЗАКЛЮЧЕНИЕ
Нарушения углеводного обмена, в том числе госпитальная гипергликемия, часто встречаются у больных с обострением бронхообструктивных заболеваний легких. Патогенез госпитальной гипергликемии обусловлен комплексом разно-образных факторов.
Особо необходимо отметить, что исследования, касающиеся изучения влияния госпитальной гипергликемии на исходы обострений ХОБЛ и БА, противоречивы, а данные о ее влиянии на формирование СД2 в последующем единичны. Таким образом, вышеизложенные данные подчеркивают актуальность темы и необходимость ее дальнейшего изучения.
Изучение этой проблемы поможет в разработке путей профилактики нарушений углеводного обмена у пациентов с бронхообструктивной патологией.