I.I. Mechnikov North-Western State Medical University of the Ministry of Healthcare of Russia, Saint Petersburg
Abstract. Indirect oral anticoagulants use in some cases may be accompanied by an increased risk of bleeding in patients after orthopedic traumatological operations.
The aim of the study was to compare coagulological, biochemical and hematological laboratory parameters while rivaroxaban and apixaban intake in patients after hip arthroplasty (HA) operation.
Material and methods. 38 patients aged 58±15 (33–85) years with hip joint osteoarthritis diagnosis were involved in the study. Laboratory study included the measiring of hemostasis parameters, biochemical parameters and hematological parameters on the analyzer. Rivaroxaban and apixaban concentration was measured in blood plasma using an ACL TOP 500CTS analyzer (Werfen, USA) on the 1st day after surgery and on the 7th day after HA.
Results. In patients receiving rivaroxaban, on the first day after HA, the average Cmax value of rivaroxaban in blood plasma was 122,4 (94–178) ng/ml, at discharge from the hospital – 186,47 (152,8-239) ng/ml, which corresponded to the therapeutic intervals. In patients using apixaban, similar indexes were 60,3 (14–95,2) and 79,85 (14–196,4) ng/ml, which also corresponded to the therapeutic intervals. While taking rivaroxaban, patients showed a statistically significant increase in INR (p <0,05), in contrast to the group of patients receiving apixaban.
Conclusion. Intake of rivaroxaban and apixaban in patients with hip joint osteoarthritis during HA was not accompanied by hemorrhagic complications. Patients in the apixaban group had higher markers of inflammation than in the rivaroxaban group. Taking into account the data obtained during this work when comparing hemostasis and C-reactive protein indexes, it is more preferable to take rivaroxaban in order to reduce the inflammatory response.
rivaroxaban
apixaban
hip arthroplasty
hemostasis
ВВЕДЕНИЕ
Антикоагулянтная терапия – важнейшая составляющая в профилактике тромботических и тромбоэмболических осложнений у пациентов, перенесших ортопедические хирургические вмешательства [1]. За счет разработки и внедрения в клиническую практику прямых ингибиторов факторов свертывания крови для перорального приема удалось значимо снизить риск венозных тромбоэмболических осложнений (ВТЭО). Эти препараты не требуют рутинного контроля свертывания крови [2–4]. Вместе с тем у пациентов со скрытыми нарушениями в системе гемостаза применение ривароксабана и апиксабана может сопровождаться повышенным риском развития интраоперационного и послеоперационного кровотечения. Особенно актуальна данная проблема у больных травматолого-ортопедического профиля, так как объемные ортопедические вмешательства могут сопровождаться значительной кровопотерей [5]. Это обстоятельство обусловливает необходимость оценки вероятности возникновения кровотечения у пациентов, получающих прямые оральные антикоагулянты, не требующие регулярного мониторинга коагуляции [6].
В настоящее время универсального теста для оценки антикоагулянтной активности прямых ингибиторов факторов свертывания, кроме определения концентрации ривароксабана и апиксабана в крови, нет, причем последнее исследование доступно лишь единичным лабораториям [5]. В повседневной практике следует учитывать совокупность клинических признаков и результатов коагулологических, биохимических и гематологических анализов [7].
Цель предлагаемого исследования – сравнить коагулологические, биохимические и гематологические лабораторные показатели при приеме ривароксабана и апиксабана у больных с остеоартритом после эндопротезирования тазобедренного сустава.
МАТЕРИАЛ И МЕТОДЫ
Дизайн работы: проспективное динамическое сравнительное исследование.
В исследование были включены 38 пациентов, находившихся в клинике травматологии и ортопедии ФГБОУ ВО «Северо-Западный государственный университет им. И.И. Мечникова» Минздрава России c диагнозом «остеоартрит тазобедренного сустава» для выполнения планового эндопротезирования тазобедренного сустава (ЭТБС). Критериями исключения служили острые воспалительные и инфекционные заболевания, включая COVID-19, сердечно-сосудистые заболевания в стадии субкомпенсации, болезни почек (клиренс креатинина менее 50 мл/мин), дыхательная недостаточность, онкологические заболевания.
Средний возраст пациентов составил 58±15 (33; 85) лет. В зависимости от проводимой терапии, пациенты были разделены на 2 группы:
- первая группа – 25 пациентов (12 женщин и 13 мужчин), получавших ривароксабан (10 мг 1 раз/сут) в течение 7 дней;
- вторая группа – 13 пациентов (6 женщин и 7 мужчин), получавших апиксабан (2,5 мг 2 раза/ сут) в течение того же времени.
Исследование было одобрено этическим комитетом ФГБОУ ВО «Северо-Западный государственный университет им. И.И. Мечникова» Минздрава России и проводилось в соответствии с этическими стандартами, изложенными в Хельсинкской декларации. Все обследованные лица дали добровольное информированное согласие на участие в исследовании.
Всем больным были выполнены лабораторные исследования до операции (исходно), после операции (на фоне приема антикоагулянта) и на 7-е сутки после проведения ЭТБС. Лабораторное исследование включало определение показателей гемостаза (международное нормализированное отношение, активированное частичное тромбопластиновое время, фибриноген, D-димер) на анализаторе STA Compact (Stago, Франция), биохимических показателей (кальций общий, кальций ионизированный, сывороточное железо, С-реактивный белок) на анализаторе COBAS Integra 400plus и гематологических параметров на анализаторе LH-500 (Beckman Coulter, США).
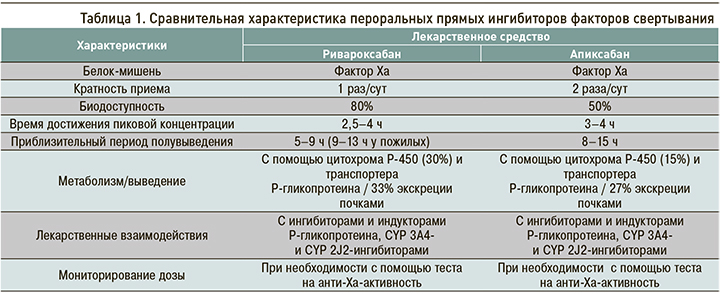
Концентрацию ривароксабана и апиксабана определяли в плазме крови на анализаторе ACL TOP 500CTS (Werfen, США) в первые сутки после операции и на 7-е сутки после ЭТБС. Все методики проводились по соответствующим инструкциям к наборам и анализаторам. Характеристика фармакокинетических и фармакодинамических свойств ривароксабана и апиксабана, а также особенности применения препаратов представлены в таблице 1.
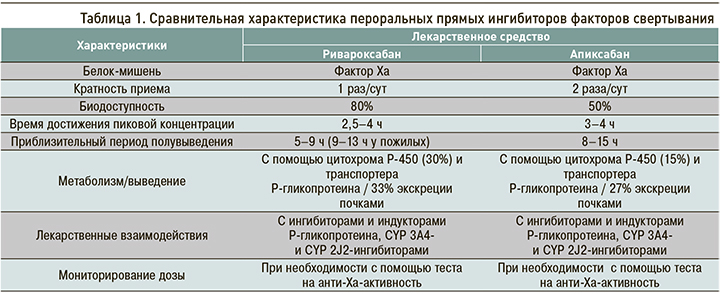
К преимуществам ривароксабана можно отнести его однократное применение, что способствует не только приверженности пациентов к лечению, но и профилактике кровотечений [8].
Статистическая обработка данных в рамках исследования осуществлялась с помощью статистической программы Jamovi. Числовые значения представлены в виде медианы Мe, 25-го и 75-го перцентилей. Для сравнения связанных количественных показателей использовался критерий Фридмана. Корреляции между показателями определяли по Спирмену. Различия считались статистически значимыми при р <0,05.
РЕЗУЛЬТАТЫ И ОБСУЖДЕНИЕ
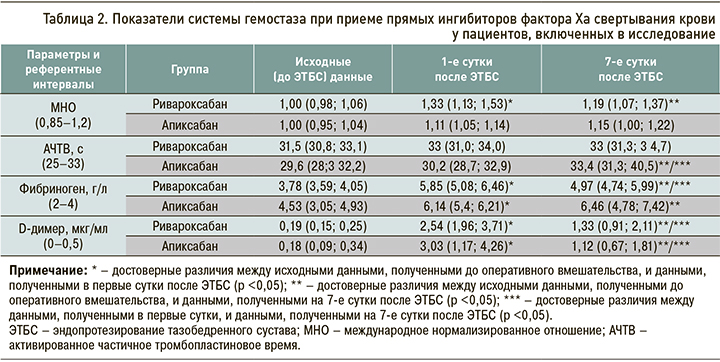
При поступлении у всех пациентов лабораторные показатели гемостаза, гематологические и биохимические маркеры находились в пределах референтных значений, кроме фибриногена, концентрация которого во 2-й группе была выше 4,53 (3,05; 4,93) г/л.
Оценка остаточного антикоагулянтного эффекта прямых ингибиторов фактора Ха (ривароксабана и апиксабана) выполнялась путем определения концентрации препарата в плазме крови. Определялась эффективность действия по максимальной концентрации (Сmax) лекарственного средства в плазме (взятие крови осуществлялось в момент достижения предполагаемой максимальной концентрации). У пациентов, получавших ривароксабан, в первый день после ЭТБС в плазме крови средняя Сmax препарата составила 122,4 нг/ мл (94; 178) и при выписке – 186,47 (152,8; 239) нг/мл, что соответствовало терапевтическим интервалам. Для апиксабана аналогичные показатели равнялись 60,3 (14; 95,2) и 79,85 (14; 196,4) нг/мл, что также соответствовало терапевтическим интервалам.
После операции при анализе показателей системы гемостаза у пациентов (табл. 2), получавших ривароксабан и апиксабан, было выявлено достоверное повышение концентрации фибриногена и D-димера по сравнению с исходными данными, что было обусловлено хирургическим вмешательством. У пациентов на фоне приема ривароксабана наблюдалось статистически значимое повышение международного нормализированного отношения (МНО, р <0,05) в отличие от группы пациентов, получавших апиксабан. Однако, по данным различных авторов, не существует унифицированного коагулологического теста, который указывал бы на эффективность антикоагулянтной активности ривароксабана или апиксабана [9, 10].
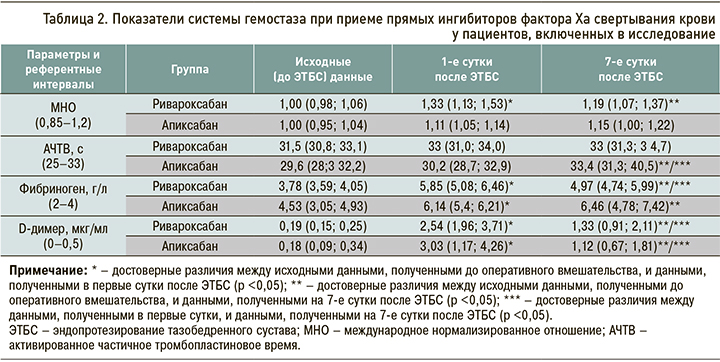
На 7-е сутки после хирургического вмешательства содержание D-димера достоверно снизилось как в группе ривароксабана, так и апиксабана, но не достигло референтных интервалов, тогда как показатели фибриногена и активированного частичного тромбопластинового времени (АЧТВ) у пациентов, получавших апиксабан, оставались высокими. Повышение фибриногена как белка острой фазы может быть обусловлено имевшим место воспалительным процессом. Таким образом, у пациентов, принимавших апиксабан, в процессе терапии воспалительная реакция не уменьшилась.
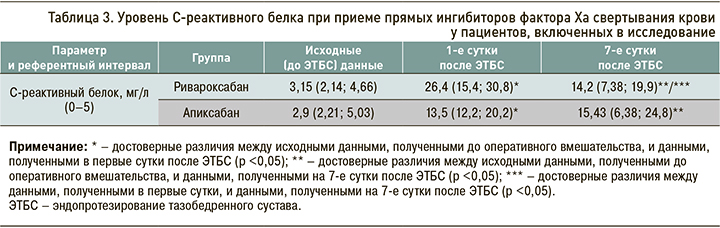
При сравнении уровней С-реактивного белка (СРБ), полученных исходно и в первые сутки после оперативного вмешательства, наблюдалось статистически значимое его повышение в обеих группах. На 7-е сутки после ЭТБС концентрация СРБ у пациентов, получавших апиксабан, оставалась высокой, тогда как в группе ривароксабана она была достоверно ниже в сравнении с концентрацией сразу после операции (табл. 3). Таким образом, в группе пациентов, принимавших апиксабан, СРБ, служащий маркером воспаления, был выше, чем в группе ривароксабана.
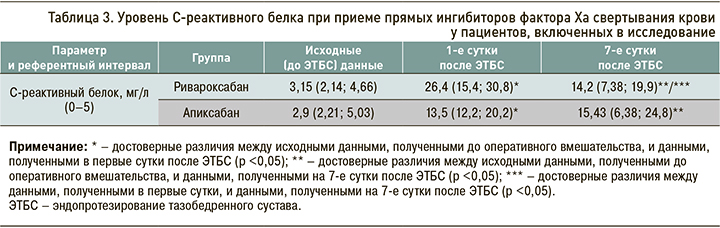
Таким образом, новые пероральные антикоагулянты ривароксабан и апиксабан обеспечивали благоприятное соотношение риска и пользы при приеме у пациентов после ЭТБС, что подтверждается литературными данными об использования этих лекарственных средств у пациентов, перенесших ортопедические оперативные вмешательства [11]. Оба препарата показали высокую эффективность и безопасность в отношении развития кровотечений [12]. В то же время, по результатам нашего исследования, у пациентов, получавших апиксабан, показатели воспаления были выше, чем в группе пациентов, применявших ривароксабан.
Опираясь на результаты исследований, посвященных новым оральным антикоагулянтам [13–16], а также данные, полученные в ходе нашей работы, можно сделать вывод, что для пациентов, перенесших ЭТБС, предпочтителен прием ривароксабана в сравнении с апиксабаном.
ЗАКЛЮЧЕНИЕ
При применении ривароксабана и апиксабана у больных после ЭТБС не наблюдалось геморрагических осложнений. Оценка концентрации этих препаратов в плазме крови показала эффективность их антикоагулянтного действия и подтвердила необходимость их приема для профилактики тромботических осложнений при высоком риске таких осложнений у пациентов после тотальной артропластики тазобедренного сустава. Учитывая полученные в этой работе данные при сопоставлении показателей гемостаза и СРБ в группах пациентов, получавших указанные прямые ингибиторы фактора Ха свертывания крови, с целью снижения воспалительной реакции можно считать предпочтительным использование ривароксабана.
- Ortel T.L., Neumann I., Ageno W. et al. American Society of Hematology 2020 guidelines for management of venous thromboembolism: Treatment of deep vein thrombosis and pulmonary embolism. Blood Adv. 2020; 4(19): 4693–738. doi: 10.1182/bloodadvances.2020001830.
- Samama M.M., Martinoli J-L., LeFlem L. et al. Assessment of laboratory assays to measure rivaroxaban – an oral, direct factor Xa inhibitor. Thromb Haemost. 2010; 103(4): 815–25. doi:10.1160/TH09-03-0176.
- Christersson C., Oldgren J., Wallentin L., Siegbahn A. Treatment with an oral direct thrombin inhibitor decreases platelet activity but increases markers of in-flammation in patients with myocardial infarction. J Intern Med. 2011; 270(3): 215–23. doi: 10.1111/j.1365-2796.2011.02354.x.
- Tamigniau A., Douxfils J., Nicolas J-B. et al. [Why, when and how to monitor new oral anticoagulants]. Rev Med Suisse. 2014; 10(416): 326–33.
- Ревишвили А.Ш., Шляхто Е.В., Замятин М.Н. с соавт. Особенности оказания экстренной и неотложной медицинской помощи пациентам, получающим прямые оральные антикоагулянты. Согласительный документ междисциплинарной группы экспертов. Вестник аритмологии. 2018; 92: 59–72. [Revishvili A.Sh., Shlyakhto E.V., Zamyatin M.N. et al. Features of the provision of emergency and urgent medical care to patients receiving direct oral anticoagulants. Consensus document of the interdisciplinary expert group. Vestnik aritmologii = Herald of Arrhythmology. 2018; 92: 59–72 (In Russ.)]. https://dx.doi.org/10.25760/VA-2018-92-59-72.
- Lindhoff-Last E., Samama M.M., Ortel T.L. et al. Assays for measuring rivaroxaban: their suitability and limitations. Ther Drug Monit. 2010; 32(6): 673–79. doi: 10.1097/FTD.0b01381f2f264.
- Douxfils J., Ageno W., Samama C-M. et al. Laboratory testing in patients treated with direct oral anticoagulants: a practical guide for clinicians. J Thromb Haemost. 2018; 16(2): 209–19. doi: 10.1111/jth.13912.
- Сычев Д.А., Синицына И.И., Цомая И.В. с соавт. Клинико-фармакологическое и клиническое обоснование кратности применения новых пероральных антикоагулягтов. Кардиология. 2017; 11: 84–93. [Sychev D.A., Sinitsyna I.I., Tsomaya I.V. et al. Clinical, pharmacological and clinical substantiation of the frequency of use of new oral anticoagulants. Kardiologiya = Cardiology. 2017; 11: 84–93 (In Russ.)]. https://dx.doi.org/10087/cadio.2017/11/10058.
- Cuker A., Siegal D.M., Crowther M.A., Garcia D.A. Laboratory measurement of the anticoagulant activity of the non-vitamin K oral anticoagulants. J Am Coll Cardiol. 2014; 64(11): 1128–39. doi: 10.1016/j.jacc.2014.05.065.
- Spyropoulos A.C., Al-Badri A., Sherwood M.W., Douketis J.D. To measure or not to measure direct oral anticoagulants before surgery or invasive procedures: Comment. J Thromb Haemost. 2016; 14(12): 2556–59. doi: 10.1111/jth.13505.
- Highcock A.J., As-Sultany M., Finley R., Donnachie N.J. A Prospective cohort comparative study of rivaroxaban, dabigatran, and apixaban oral thromboprophylaxis in 2431 hip and knee arthroplasty patients: Primary efficacy out-comes and safety profile. J Arthroplasty. 2020; 35(11): 3093–98. doi: 10.1016/j.arth.2020.06.032.
- Connors J.M. Testing and monitoring direct oral anticoagulants. Blood. 2018; 132(19): 2009–15. doi: 10.1182/blood-2018-04-791541.
- Battistelli S., Fortina M., Carta S. et al. Serum C-reactive protein and procalcitonin kinetics in patients undergoing elective total hip arthroplasty. Biomed Res Int. 2014; 2014: 565080. doi: 10.1155/2014/565080.
- Jiang Y., Li J., Liu Y. et al. Risk factors for deep vein thrombosis after orthopedic surgery and the diagnostic value of D-dimer. Ann Vasc Surg. 2015; 29(4): 675–81. doi: 10.1016/j.avsg.2014.12.022.
- Paruk F., Chausse J.M. Monitoring the post surgery inflammatory host response. J Emerg Crit Care Med. 2019; 3: 47. doi: 10.21037/jeccm.2019.08.06.
- Poredos P., Poredos P., Jezovnik M.K. et al. Time course of inflammatory and procoagulant markers in the early period after total hip replacement. Clin Appl Thromb Hemost. 2021; 27: 1076029620985941. doi: 10.1177/1076029620985941.
Ksenia N. Zamyatina, postgraduate student at the Department of biological and general chemistry named after V.V. Sokolovsky, I.I. Mechnikov North-Western State Medical University of the Ministry of Healthcare of Russia. Address: 191015, Saint Petersburg, 41 Kirochnaya Str. E-mail:
ksenija.zamyatina@yandex.ru. ORCID: 0000-0002-6890-6357
Sergey A. Sayganov, MD, professor, rector of I.I. Mechnikov North-Western State Medical University of the Ministry of Healthcare of Russia. Address: 191015, Saint Petersburg, 41 Kirochnaya Str. E-mail:
rectorat@szgmu.ru. ORCID: 0000-0001-8325-1937
Vadim I. Mazurov, MD, professor, academician of RAS, Chief scientific consultant, head of the Department of therapy, rheumatology, temporary disability and medical care quality examination named after E.E. Eichwald, I.I. Mechnikov North-Western State Medical University of the Ministry of Healthcare of Russia. Address: 191015, Saint Petersburg, 41 Kirochnaya Str. E-mail:
rectorat@szgmu.ru. ORCID: 0000-0002-0797-2051
Larisa B. Gaykovaya, MD, associate professor, head of the Department of biological and gleneral chemistry named after V.V. Sokolovsky, I.I. Mechnikov North-Western State Medical University of the Ministry of Healthcare of Russia. Address: 191015, Saint Petersburg, 41 Kirochnaya Str. E-mail:
Larisa.Gaikovaya@szgmu.ru. ORCID: 0000-0003-1000-1114
Alexander N. Tkachenko, MD, professor, professor of the Department of traumatology, orthopedics and mlilitary field surgery, I.I. Mechnikov North-Western State Medical University of the Ministry of Healthcare of Russia. Address: 191015, Saint Petersburg, 41 Kirochnaya Str. Е-mail:
altkachenko@mail.ru. ORCID: 0000-0003-4585-5160
Irina L. Urazovskaya, PhD, assistant of the Department of hospital surgery and cardiologynamed after M.S. Kushakovsky, I.I. Mechnikov North-Western State Medical University of the Ministry of Healthcare of Russia. Address: 191015, Saint Petersburg, 41 Kirochnaya Str. E-mail
langelova@yandex.ru. ORCID: 0000-0003-4165-4599
Dzhalolidin S. Mansurov, PhD, assistant at the Department of traumatology, orthopedics and military field surgery, I.I. Mechnikov North-Western State Medical University of the Ministry of Healthcare of Russia. Address: 191015, Saint Petersburg, 41 Kirochnaya Str. E-mail
jalolmedic511@gmail.com. ORCID: 0000-0002-1799-641X
Valery M. Khaidarov, PhD, associate professor of the Department of traumatology, orthopedics and military field surgery, I.I. Mechnikov North-Western State Medical University of the Ministry of Healthcare of Russia. Address: 191015, Saint Petersburg, 41 Kirochnaya Str. E-mail:
drxaydarov@mail.ru. ORCID: 0000-0002-0754-4348
Alexander G. Balgley, assistant at the Department of traumatology, orthopedics and military field surgery, I.I. Mechnikov North-Western State Medical University of the Ministry of Healthcare of Russia. Address: 191015, Saint Petersburg, 41 Kirochnaya Str. E-mail:
balgley.aleksandr@szgmu.ru. ORCID: 0000-0003-0964-6871