Острые нарушения мозгового кровообращения (ОНМК) являются второй по значимости причиной смерти и основной причиной инвалидности во всем мире. Заболеваемость увеличивается из-за старения населения. Ишемический инсульт встречается чаще, но геморрагический инсульт вызывает большее количество смертей. Заболеваемость и смертность от инсульта различаются между странами, географическими регионами и этническими группами. В настоящее время примерно от 3 до 4% общих расходов на здравоохранение в западных странах тратится именно на инсульт [1].
Бремя инсульта у людей моложе 65 лет увеличилось за последние несколько десятилетий, при этом заболеваемость во всем мире выросла на 25% среди взрослых в возрасте от 20 до 64 лет [2]. Наблюдается тревожный сдвиг его распространенности в сторону более молодого возраста. Так, заболеваемость артериальным ишемическим инсультом составляет 2,4 на 100 000 среди 20–24-летних, 20 на 100 000 среди 35–44-летних и 1200 на 100 000 среди пациентов в возрастной группе 75–84 лет [3, 4].
В настоящее время отдельно изучается группа заболеваний, которая связана с врожденной патологией соединительной ткани (СТ), проявляющейся снижением ее прочности. В развитии дисплазий СТ ведущее значение имеют мутации генов, кодирующих синтез и пространственную организацию коллагена, ответственных за формирование компонентов матрикса, а также ферментов, принимающих участие в процессах фибриллогенеза [5]. Выделяют группу наследственных заболеваний СТ (НЗСТ): на сегодняшний день описано более 200 таких заболеваний, поражающих СТ различных систем органов, включая сердце, кровеносные сосуды, кости, глаза, кожу, суставы и легкие. За открытием этих НЗСТ последовала идентификация мутаций в широком диапазоне генов, кодирующих структурные белки, модифицирующие ферменты и др. Три типичных примера НЗСТ – синдром Марфана (СМ), синдром Элерса–Данлоса (СЭД) и синдром Лойса–Дитца (СЛД). Эти синдромы демонстрируют некоторую степень фенотипического совпадения сердечно-сосудистых, скелетных и кожных особенностей [6].
В работе Bascom R. et al. (2019) при исследовании 1009 участников с широким спектром наследственных фенотипов СТ (средний возраст 39±18 лет; 71% женщин и 29% мужчин; 83% респондентов отнесли себя к кавказской национальности) с учетом диагностических критериев выявлялись СЭД (классический – 50 случаев, гипермобильный – 99, сосудистый – 101, редкие и неклассифицированные формы – 178), СМ (n=33), синдром Стиклера (n=60), фибромускулярная дисплазия (n=135), другие дисплазии СТ (n=72) [7].
Считается, что пациенты с такими заболеваниями СТ, как синдром СМ, СЭД и СЛД, подвержены более высокому риску ряда цереброваскулярных заболеваний – внутричерепных аневризм, диссекций артерий и острых ишемических инсультов. Наиболее общепринятое этиологическое объяснение такой связи заключается в том, что генетические мутации, участвующие в указанных заболеваниях СТ, влияют на коллаген и протеогликаны, образующие внеклеточный матрикс; это приводит к повреждению стенки сосуда [8].
СИНДРОМ МАРФАНА
СМ – наиболее часто наследуемое заболевание СТ, частота которого составляет 2–3 случая на 10 000 человек. Аутосомно-доминантная мутация гена фибриллина 1 (FBN1) выступает наиболее частой причиной СМ. На спорадические de novo мутации приходится 25% случаев заболевания. В отношении СМ не установлена расовая или гендерная предрасположенность [9].
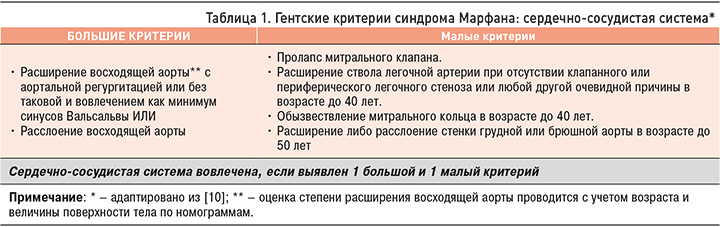
Диагностика СМ сегодня по-прежнему основана на Гентских критериях [10]. Поражения сердечно-сосудистой системы, относящиеся к большим и малым критериям СМ, приведены в таблице 1. Сердечно-сосудистая система вовлечена в патологический процесс, если выявлен один большой или один малый критерий.
При СМ в крупных и средних артериях дефект фибриллина ассоциируется с распадом эластических волокон, что предрасполагает к развитию аневризм и артериальных диссекций [11–14]. Это может быть причиной церебральных и спинальных инфарктов и кровоизлияний.
По данным ретроспективного исследования 513 больных с СМ, 3,5% участников имели васкулярные события; у 83% из них были ишемические инсульты (11 транзиторных ишемических атак, 2 церебральных инфаркта, 2 инфаркта спинного мозга), у 16% (n=3) – геморрагические ОНМК (2 – субдуральные гематомы, 1 – спинальное субарахноидальное кровоизлияние). Средний возраст пациентов в этой серии исследований составил 39,6 лет. Источник высокого риска сердечной эмболии был выявлен в 77% случаев, кардиоэмболическая причина (протезирование клапанов сердца, фибрилляция предсердий) ишемического инсульта имелась у 12 из 13 пациентов с СМ [15]. Gott V.L. et al. описали развитие церебральных эмболии у 25 из 675 пациентов с СМ (3,7%) после операций на аорте [16]. Другие авторы наблюдали пациентов с вероятным СМ или семейным анамнезом этого заболевания, у которых были выявлены патологические изменения в виде кистозного медионекроза аорты, ассоциированного с диссекцией церебральных артерий [17, 18]. Расслоение брахиоцефальных и общих сонных артерий может привести к ишемическому инсульту при СМ [19, 20].
Был проведен ряд исследований для изучения связи между внутричерепными аневризмами и СМ [21, 22]. Аневризмы при СМ могут быть мешковидными, веретеновидными или расслаивающими. При СМ аневризмы могут располагаться в проксимальном отделе внутричерепной сонной артерии [23].
В недавно опубликованном исследовании Kim S.T. et al. показали, что распространенность внутричерепных аневризм среди пациентов с СМ составляла 14% (8/59) [21]. Из 59 пациентов, которым была выполнена ангиография головы, у 8 человек (14%) было всего 12 внутричерепных аневризм – 9 мешковидных и 3 веретенообразных. Средний размер внутричерепных аневризм был равен 5,5±7,4 мм. Среди пациентов с аневризмами 2 из 8 (33%) были мужчинами и 2 пациента были моложе 50 лет. Другими внутричерепными находками были прямой кавернозный свищ сонной артерии (n=1) и диссекция (n=2). У 1 пациента с диссекцией был ишемический инсульт, у другого – транзиторная ишемическая атака. Случаи субарахноидального кровоизлияния не отмечались. Увеличение возраста было единственной переменной, независимо связанной с наличием внутричерепной аневризмы.
СИНДРОМ ЭЛЕРСА–ДАНЛОСА
СЭД – это группа заболеваний СТ, которая клинически и генетически неоднородна: все подтипы характеризуются аномалиями кожи, связок и суставов, кровеносных сосудов и внутренних органов. Наиболее типичными признаками этого заболевания являются гипермобильность суставов, гиперрастяжимость кожи и хрупкость сосудов.
До четверти пациентов с СЭД имеют аневризму аорты [24]. Предполагаемая распространенность СЭД колеблется от 1:5000 до 1:25 000 [25].
Диагностика СЭД, основанная на Вильфраншских критериях (1997), выделяет 6 различных подтипов СЭД в зависимости от типичных клинических характеристик: классический, гипермобильный, сосудистый, кифосколиотический, артрохалазия, дерматоспараксис [26]. Большими признаками сосудистого СЭД в соответствии с этими критериями служат тонкая, прозрачная кожа, разрывы стенки артерий, кишечника и/или матки, обширные кровоизлияния, характерный фенотип, малыми признаками – гипермобильность мелких суставов, разрыв сухожилий и мышц, косолапость, варикозное расширение вен с ранней манифестацией, артериовенозные каротидно-кавернозные фистулы, атрофия десневого края, пневмоторакс/пневмогидроторакс, положительный семейный анамнез, случаи внезапной смерти у близких родственников (многие пациенты не доживают до 50 лет из-за разрыва артерий или, что реже, кишечника).
Классический и сосудистый типы СЭД предполагают развитие диссекций церебральных артерий [27–29]. Последняя нозологическая классификация, предложенная в 2017 г., выделяет 13 подтипов СЭД и делает упор на молекулярной идентификации различных вариантов (табл. 2) [30].

Сосудистый подтип СЭД, ранее называвшийся «синдромом Элерса–Данлоса типа IV», наследуется по аутосомно-доминантному типу и вызывается мутациями в COL3A1. Его предполагаемая распространенность колеблется от 1:50 000 до 1:100 000 [31, 32] и составляет примерно 5% всех случаев СЭД [33]. Сосудистый подтип имеет худший прогноз среди всех подтипов СЭД из-за разрыва артерий [32]. Люди с этим подтипом заболевания, как сообщалось, имели среднюю продолжительность жизни менее 50 лет [34].
Большинство сообщений об инсульте и цереброваскулярных заболеваниях при СЭД касаются сосудистого подтипа и включают внутричерепные аневризмы, субарахноидальное кровоизлияние, спонтанное расслоение артерий и каротидно-кавернозную фистулу [35].
В исследовании Shalhub S. et al. [36] в 11 лечебных учреждениях были выявлены 173 человека (35,3% мужчин, 56,6% европеоидной расы) с сосудистым подтипом СЭД. 11 из них (9,8%) имели непатогенные изменения в COL3A1 и были исключены из анализа. Среди оставшихся лиц у 86 (47,7% мужчин, 68% европеоидов, 48,8% пациентов с положительным семейным анамнезом) наблюдались патогенные варианты COL3A1, а у 76 (19,7% мужчин, 19,7% европеоидов, 43,4% пациентов с положительным семейным анамнезом) были диагностированы только по клиническим критериям без подтверждения молекулярным тестированием [36]. В когорте с патогенными вариантами COL3A1 средний период наблюдения с момента постановки диагноза составил 8,2±8,28 года. За период наблюдения умерло 13 (15,1%) человек (средний возраст 40,3±15,5 лет). Причины смерти были следующим: 2 случая – инсульт, 1 – диссекция коронарной артерии, 1 –разрыв желудочка, 2 – расслоение аорты, 1 – гемоторакс, 1 – разрыв брыжеечной артерии. В остальных случаях причина была неизвестна. В когорте без молекулярного подтверждения СЭД средний срок наблюдения с момента постановки диагноза составил 9,8±8,8 года. В этой группе умерло 6 (7,8%) пациентов (средний возраст 35,8±15,6 года): 1 – из-за геморрагического инсульта, 1 – из-за расслоения и разрыва сосудов без указания локализации, 1 – из-за осложнений от перфорации внутренних органов. В 3 случаях причина смерти осталась неизвестна.
Потенциальная связь между дефицитом коллагена при СЭД и церебральными аневризмами обсуждалась давно [37, 38]. Внутричерепные аневризмы у пациентов с СЭД могут быть мешковидными или веретенообразными [23]. Исследования, изучающие распространенность аневризм и субарахноидального кровоизлияния у пациентов с СЭД, дали разные результаты. Pepin М. et al. в исследовании 419 пациентов с СЭД или семейным анамнезом заболевания обнаружили 6 больных с внутричерепными аневризмами [39]. North К. et al. в исследовании 202 пациентов отметили, что у 6 пациентов имели место каротидно-кавернозные фистулы, у 4 – разрыв внутричерепных аневризм, еще у 4 – внутричерепное кровоизлияние неясной этиологии [40]. Однако не все пациенты в этих исследованиях прошли скрининг на внутричерепные аневризмы с помощью визуализации.
Крупнейшее на сегодняшний день исследование распространенности неразорвавшихся внутричерепных аневризм среди пациентов с СЭД с помощью визуализации внутричерепных сосудов показало, что распространенность аневризм у них составляет 12% [21]. Из 99 пациентов, которым была выполнена ангиография сосудов головы, у 12 (12%) было в общей сложности 14 внутричерепных аневризм – 9 мешковидных и 5 веретенообразных. Средний размер внутричерепных аневризм был равен 6,9±6,5 мм. Из 12 пациентов с аневризмами и СЭД у 1 был СЭД I типа, у 3 – III типа, у 7 – IV типа. В одном случае подтип СЭД был неизвестен.
Дефект коллагена может предрасполагать к развитию спонтанных диссекций экстракраниальных отделов сонных и позвоночных артерий. Диссекция позвоночных, внутренних и наружных сонных артерий выступает типичным проявлением СЭД [26, 40–42].
СИНДРОМ ЛОЕСА–ДИТЦА
СЛД – редкое аутосомно-доминантное заболевание СТ, которое возникает в результате множества генетических изменений, приводящих к формированию аневризм аорты, генерализованной извилистости артерий, гипертелоризму, аномалиям язычка (раздвоение/широкий язычок) или волчьей пасти [43]. Впервые оно было описано бельгийским врачом Loeys B.L. и американским врачом Dietz H.S. в 2005 г. [44, 45]. Средняя продолжительность жизни пациентов с СЛД различна – от 26 до 37 лет [44, 45]. Летальный исход обычно наступает из-за расслоения или разрыва аневризмы аорты, других артерий крупного калибра и внутричерепных кровоизлияний [46]. При данном заболевании развиваются мутации в генах, отвечающих за синтез белков-рецепторов трансформирующего фактора роста бета первого и второго типа (TGFR1 и TGFR2), а также гена SMAD3. Мутации в генах TGFβR1/TGFβR2 ведут к увеличению активности TGF-β в кровеносных сосудах, что ведет к избыточной продукции коллагена, потере эластина и неправильному расположению эластических волокон [47–49].
Имеется лишь несколько сообщений о распространенности внутричерепных аневризм у пациентов с СЛД [50–54]. В одном нейрорадиологическом исследовании, проведенном с участием 25 больных с положительным генетическим тестом на СЛД, 8 человек (32%) имели внутричерепные аневризмы, что свидетельствует о важности серийного неинвазивного визуализационного мониторинга у молодых пациентов [55]. Наряду с аневризмами авторы отметили наличие у 3 пациентов с положительным генетическим тестом на СЛД диссекции сонной и вертебробазилярной артерий.
В другом исследовании, также среди 25 пациентов с клиническим или генетическим диагнозом СЛД, Kim S. et al. обнаружили, что у 7 (28%) из них имелись внутричерепные аневризмы [21]. По данным ангиографии сосудов головы, у этих 7 пациентов было всего 8 внутричерепных аневризм – 7 мешковидных и 1 веретенообразная аневризма. Средний размер внутричерепных аневризм составил 4,8±4,5 мм. Среди пациентов с аневризмами 4 из 7 (57%) были мужчинами и 4 были моложе 50 лет.
ЭЛАСТИЧЕСКАЯ ПСЕВДОКСАНТОМА
Эластическая псевдоксантома (ЭП) – генетическое заболевание с аутосомно-рецессивным наследованием, вызванное мутациями в ABCC6 гене [56]. Клиническая распространенность ее оценивается от 1 на 100 000 до 1 на 25 000 населения в целом с незначительным преобладанием у женщин [57, 58]. Первыми клиническими признаками ЭП, начинающимися обычно в детском или подростковом возрасте [59], как правило, являются характерные изменения кожи (мелкие желтые папулы диаметром до 10 мм) на затылке и по бокам шеи и на изгибах (таких как подмышечные впадины, локтевой ямки, а также в околопупочной области, паховых и подколенных областях) [60]. В редких случаях пациенты с генетически подтвержденной ЭП могут иметь гистологически нормальную кожу [61]. Наиболее серьезны офтальмологические проявления ЭП, так как они могут привести к слепоте на поздней стадии заболевания. Характерная глазная особенность ЭП – наличие ангиоидных полосок в сетчатке [62].
Сосудистые признаки (за исключением хромоты) при ЭП обычно проявляются спустя годы после появления кожных и глазных изменений [56]. Пациенты имеют повышенный риск развития сосудистых заболеваний, поскольку изменения отмечаются преимущественно в средней и нижней части дермы, где эластические волокна неравномерно распределены, утолщены, фрагментированы в виде комков, глыбок, своеобразно закручивающихся пучков или зернистых структур. Также характерно наличие кальция [63].
Об увеличении толщины интима-медиа (ТИМ) сонной артерии сообщалось в двух исследованиях на людях [64, 65] и еще в одном, недавно проведенном на мышах [66]. Повышенный ТИМ сонной артерии независимо связан с более высоким риском сердечно-сосудистых событий, что может представлять собой важный аргумент для объяснения ускоренного атеросклероза при ЭП с более высоким, чем обычно, риском развития кардиоваскулярных заболеваний [67].
Основным клиническим проявлением минерализации артериальной стенки при ЭП выступает перемежающаяся хромота как в нижних, так и в верхних конечностях, и заболевания периферических артерий [68, 69]. Есть данные об аневризмах [70, 71], инсультах [68, 71], транзиторных ишемических атаках [71, 72], стенозе артерий среднего размера (таких как лучевая артерия) [64, 73] и аорты [64].
Частота ишемического инсульта при ЭП, хотя и четко не установлена, однако, по всей видимости, выше, чем в общей популяции [74], со значением 15% в когорте из 38 пациентов с ЭП [68] и 7% в другой когорте из 100 пациентов [71]. В когорте из 100 пациентов ишемический инсульт был зарегистрирован у 7 пациентов, причем у 1 больного наблюдался рецидив этого ОНМК; в результате относительный риск ишемического инсульта составил 3,6 (95% доверительный интервал 3,3– 4,0) у пациентов в возрасте до 65 лет [71].
ЗАКЛЮЧЕНИЕ
Таким образом, наследственные заболевания СТ относятся к наиболее распространенным генетическим заболеваниям человека. Пациенты с этими заболеваниями подвержены более высокому риску ряда цереброваскулярных заболеваний, таких как внутричерепные аневризмы, расслоения и острые ишемические инсульты. Наиболее общепринятое причинное объяснение этой связи состоит в том, что генетические мутации, участвующие в таких заболеваниях СТ, влияют на коллаген и протеогликаны, которые образуют внеклеточный матрикс, что приводит к ослаблению стенки сосуда. Поскольку предполагается более высокая распространенность этих сосудистых осложнений у пациентов с заболеваниями СТ, то важно, чтобы различные специалисты знали о клинической картине этих заболеваний.
Определение этиологии инсульта является достаточно сложной диагностической задачей независимо от возраста пациентов, но более трудной у молодых. Использования новых методов нейровизуализации и молекулярно-генетических исследований – это прогресс в выявлении причин и механизмов инсульта на современном этапе ангионеврологии. Выявление случаев инсульта, вызванных моногенными расстройствами, важно как для принятия терапевтических решений, так и генетического консультирования.